Diagnosing Coronary Disease in 2025
Objectives
-
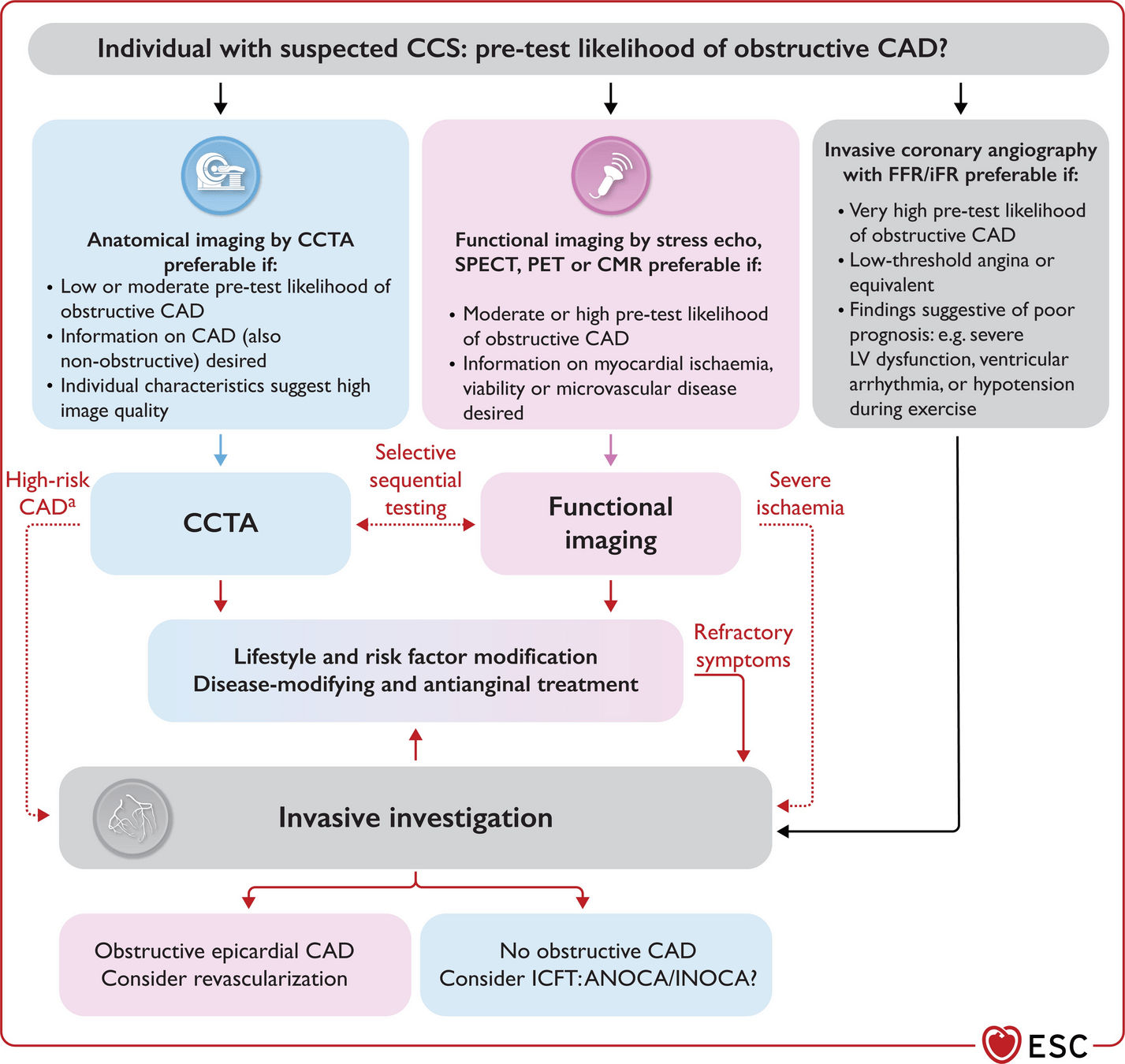
Overview of diagnostic modalities available for chronic coronary disease.
-
Approach to choosing the optimal test.
-
Special cases, new technologies, and future directions.
Relevant Guidelines
-
European: 2024 Guidelines for the management of chronic coronary syndromes
-
American: 2023 Multimodality Appropriate Use Criteria for the Detection and Risk Assessment of Chronic Coronary Disease
-
Canadian: 2014 (Outdated)
Rationale
-
Recent fellowships in Stress Echo and Nuclear Cardiology (SPECT and PET)
-
PET is expanding in Canada
-
Recent advances in Stress Echo (expanded protocols), Nuclear (PET + myocardial blood flow), and Clinical (ANOCA/INOCA)
Assessing Risk
Assessment
- Rule out ACS
- Non-cardiac causes
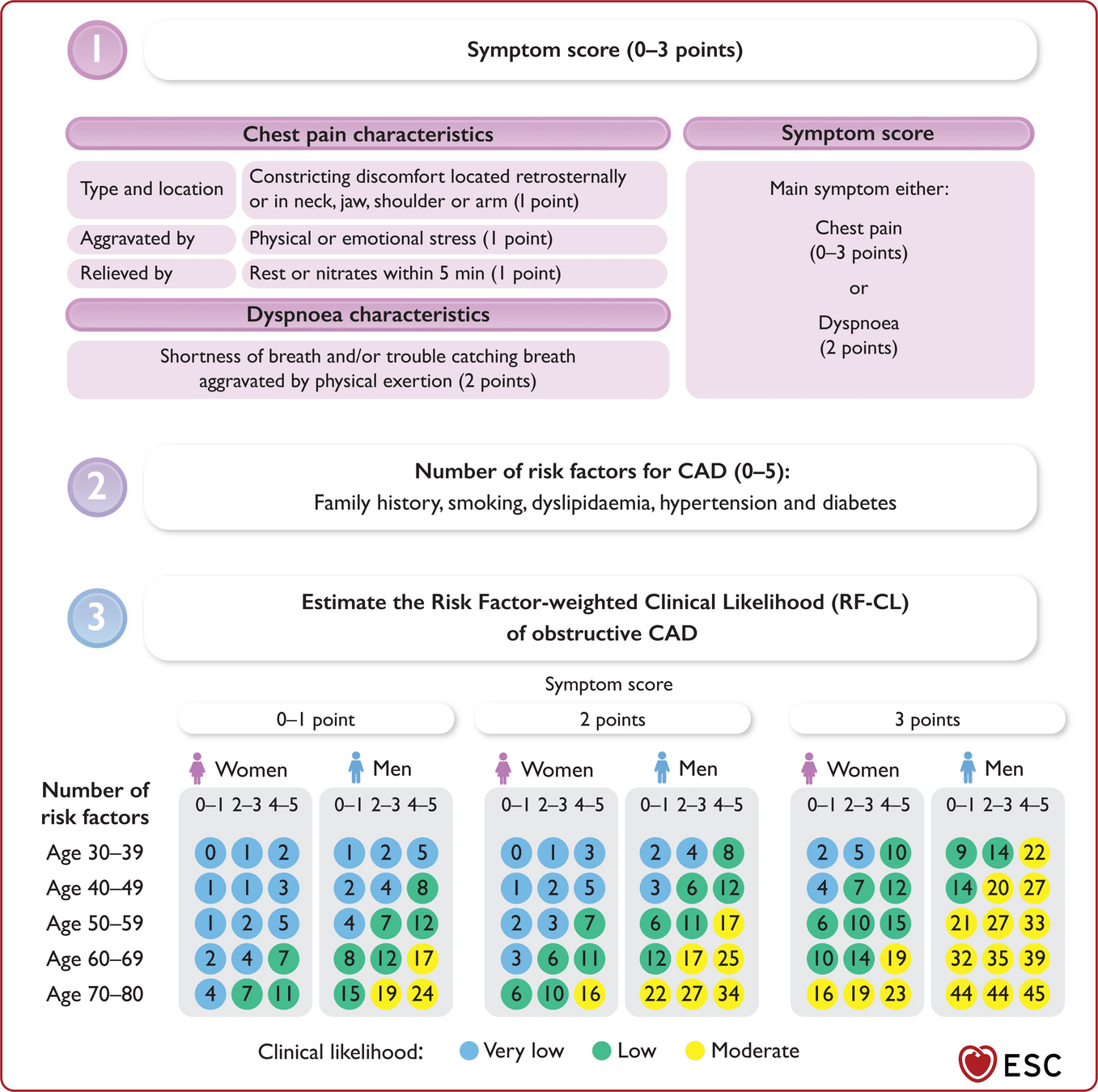
- Assess pre-test probability
History
- New studies show women and men present with typical chest pain similarly
- 2/3 of both men/women present with symptoms categorized as non-characteristic
- Women with CAD:
- Older, hypertensive, dyslipidemia, + family Hx
- Lower risk calculated by risk scores
- Asymptomatic: more often in DM2, elderly, severe disease
- Typical vs Atypical
- Typical can predict obstructive CAD but less predictive for microvascular disease and vasospasm
Baseline Tests
- ECG
- Risk factor blood work
- CBC, Lytes, Creatinine, Glucose, A1C, Lipids, TSH
- LP(a) [once in patient's life]
- Transthoracic Echo
Lipoprotein (a)
- LP(a)
- Genetically inherited cholesterol
- Stable over the course of a lifetime
- Associated with increased risk of CVD
- No current targeted drugs on market but in testing
- If elevated - aggressively manage other RFs
- Lower threshold to refer to Cardiology to risk stratify
CCS +
LP(a)
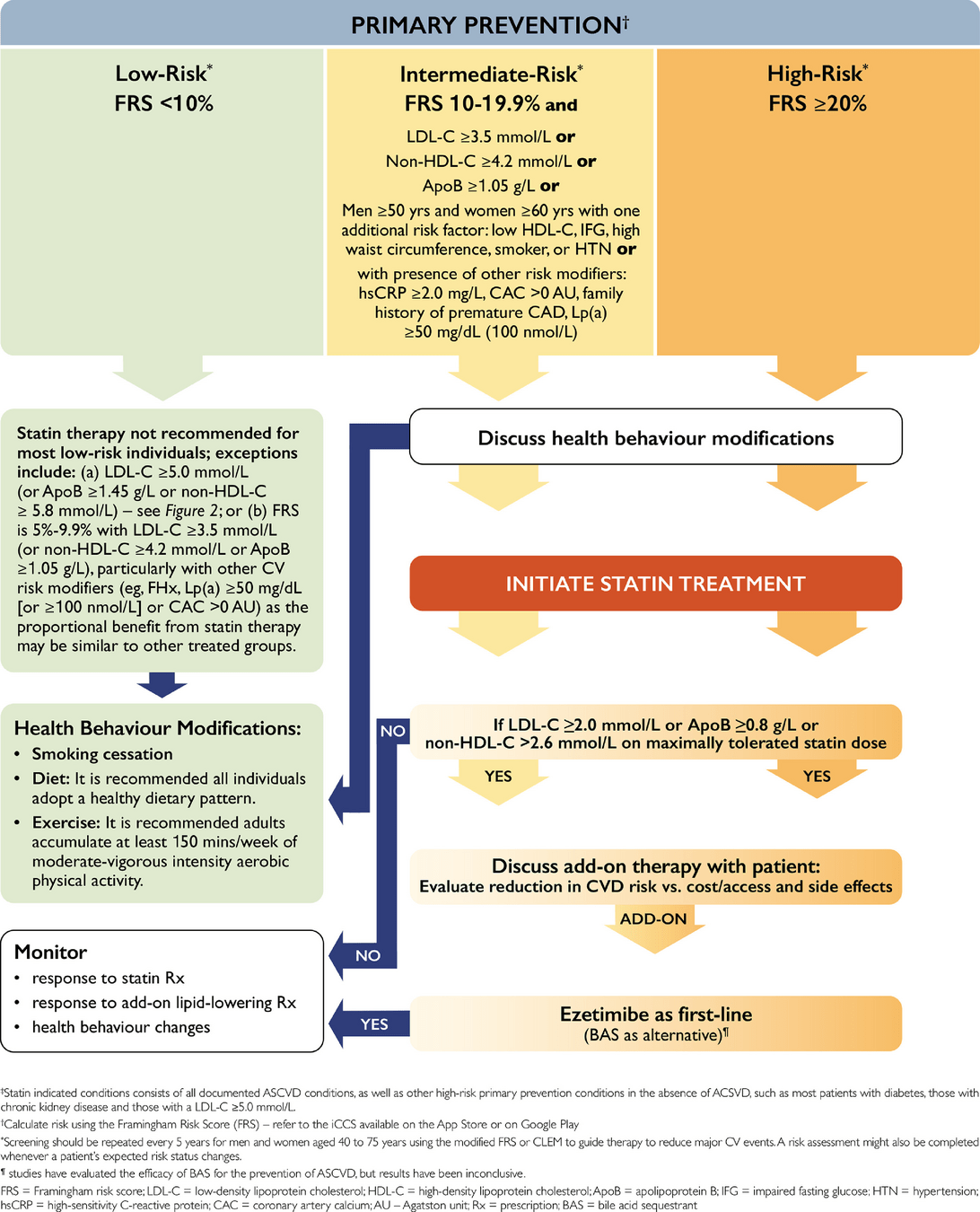
Note: FRS 5% + and elevated LP(a) should consider statin
Notes
- Modify risk % further if other strong RF (ie. FH or PAD) or other clinical data (ie. vascular calcium on imaging)
- Old risk tables based solely on chest pain, not accurate
Low Risk
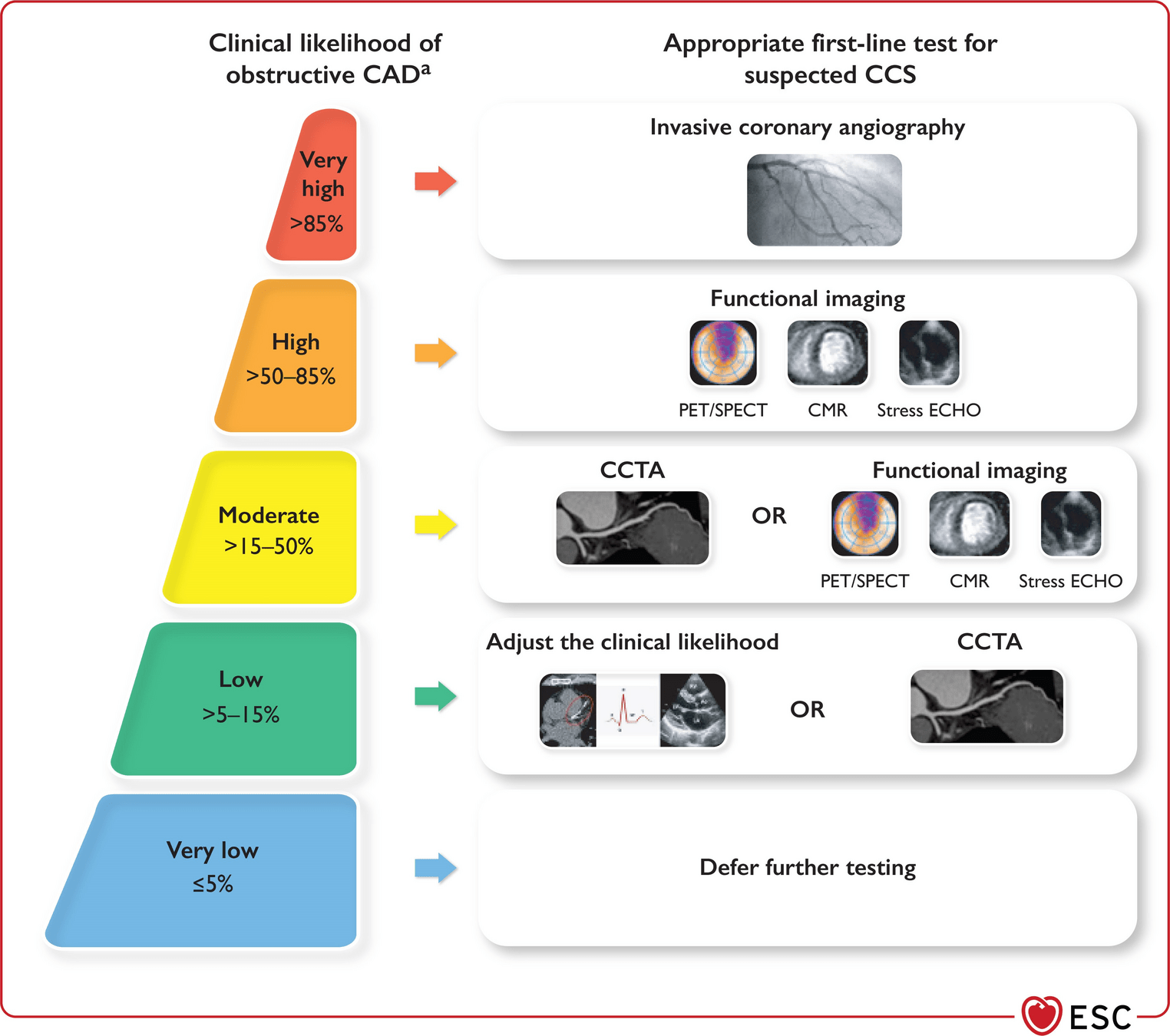
- <5% Very Low Risk - Defer testing
- 5-15% Low Risk
- Calcium score
- GXT
- Non-coronary imaging
- Aorta/Carotid US
- CT Thorax
- Help decide on statin
RF Score + Calcium Score
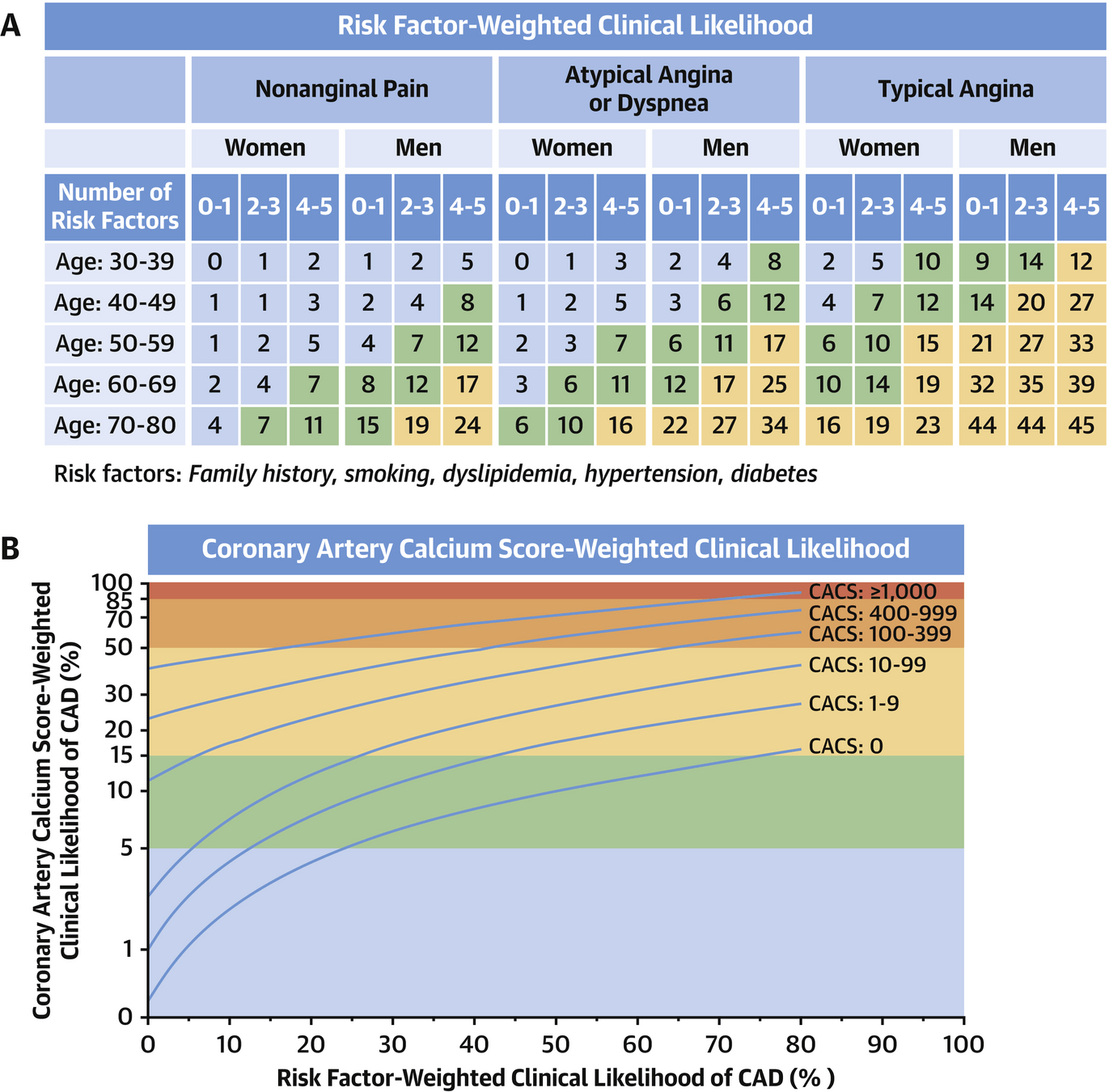
https://www.jacc.org/doi/10.1016/j.jcmg.2021.11.019
Intermediate
- Risk >15%:
- Stress Echo
- SPECT or preferably PET
- Stress Cardiac MRI
- CT Coronary (risk >5%)
- GXT not recommended first line
Note: no straight to cath option
ANOCA/INOCA
Definitions
-
INOCA: ischemia without obstructive CAD
-
ANOCA: angina without obstructive CAD
-
MINOCA: myocardial infarction without obstructive CAD
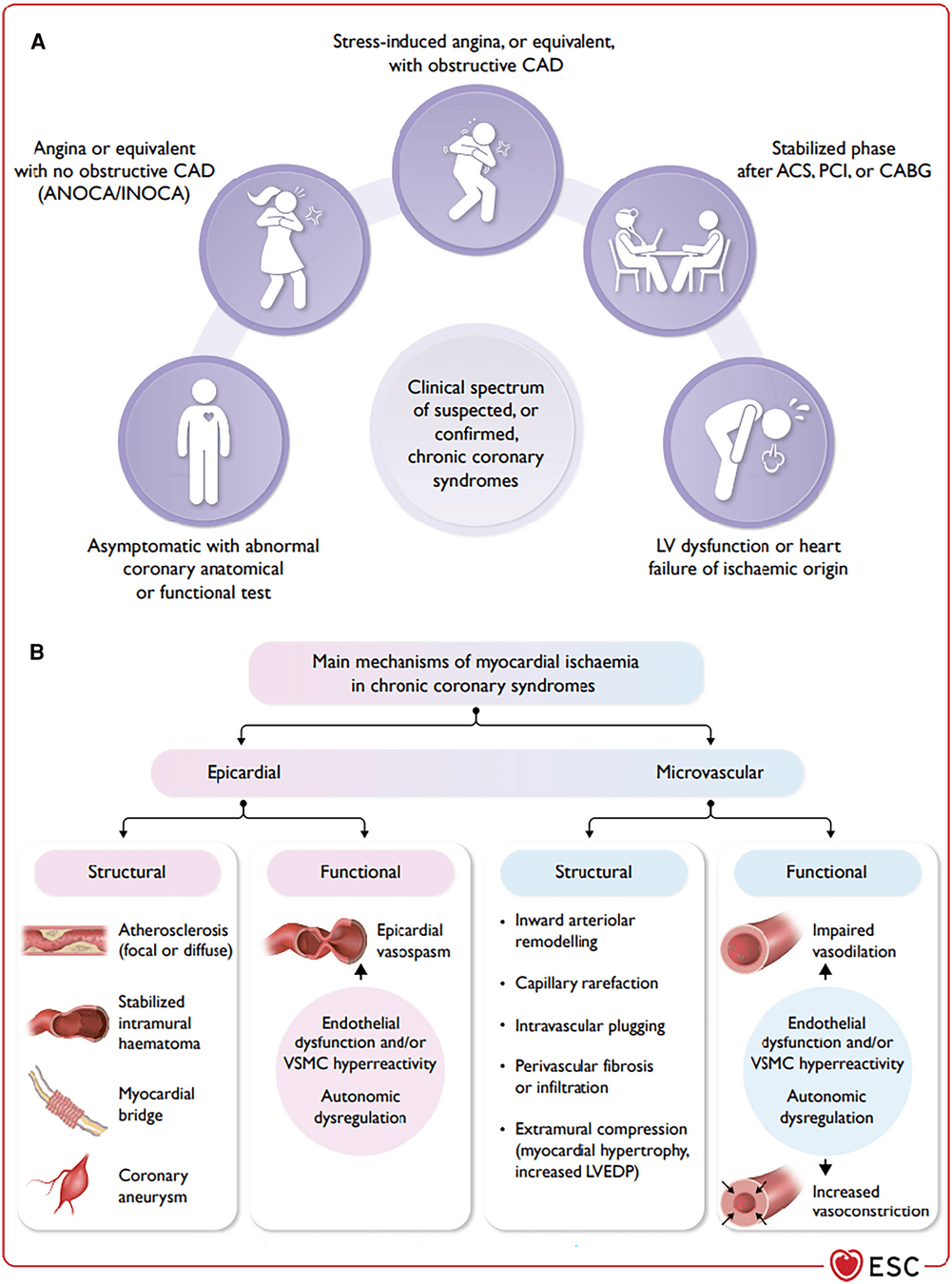
- Endotypes: vasospasm vs microvascular disease
- Vasospasm can be diagnosed on cardiac monitoring or provocative testing on cath (if high suspicion)
- Microvascular disease diagnosed on cath or non-invasive tests
- Treatment
- ASA if CAD
- Statin
- Anti-anginals
Stress Echo 2025
Traditional Stress Echo
- Identification of regional wall motion abnormalities to identify obstructive coronary artery disease
- Qualitatively assessed
- Other prognostic parameters:
- Exercise duration, BP response, ST-T changes and LV dilation (not reliably reported)
- Functional test: thus does not diagnose non-obstructive atherosclerotic disease that can still cause events
Compared to Alternatives
-
Advantages
- Inexpensive
- No radiation
- Portable
- Exercise and non-exercise
- Less environmental impact compared to MRI/SPECT
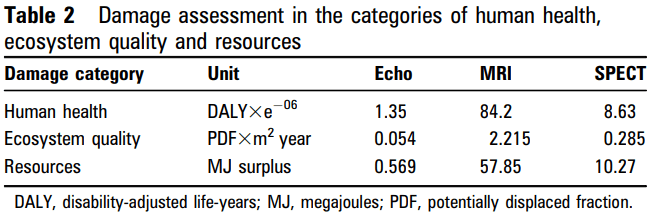
Compared to Alternatives
-
Disadvantages
- Functional testing thus may not pick up non-obstructive clinical atherosclerosis that can cause future events
- Compared to Coronary CT
- WMA are later in the ischemic cascade (not capturing perfusion changes)
- Compared to myocardial perfusion imaging
- WMA based protocol less useful in evaluating INOCA (ischemia with no obstructive CAD)
- Functional testing thus may not pick up non-obstructive clinical atherosclerosis that can cause future events
Rest
Post Exercise
LAD Ischemia
Why New Protocol?
- Change in referral pattern leading to a dropping positivity rate (<10% in some studies)
- Reduced predictive value
- Traditional stress echo protocol does not capture other areas of vulnerability in a heterogeneous population beyond identifying obstructive CAD
- ie. lung water, LV contractile reserve, coronary microcirculation and cardiac autonomic dysfunction
- New parameters are able to be implemented in Echo Labs without new technologies/sofware
ABCDE-SE Protocol
A - Wall motion abnormalities, volumes*
B - B Lines
C - Left ventricular contractile reserve*
D - Coronary flow reserve
E - Heart rate reserve*
*do not require additional imaging based on current protocol
Example: CAD
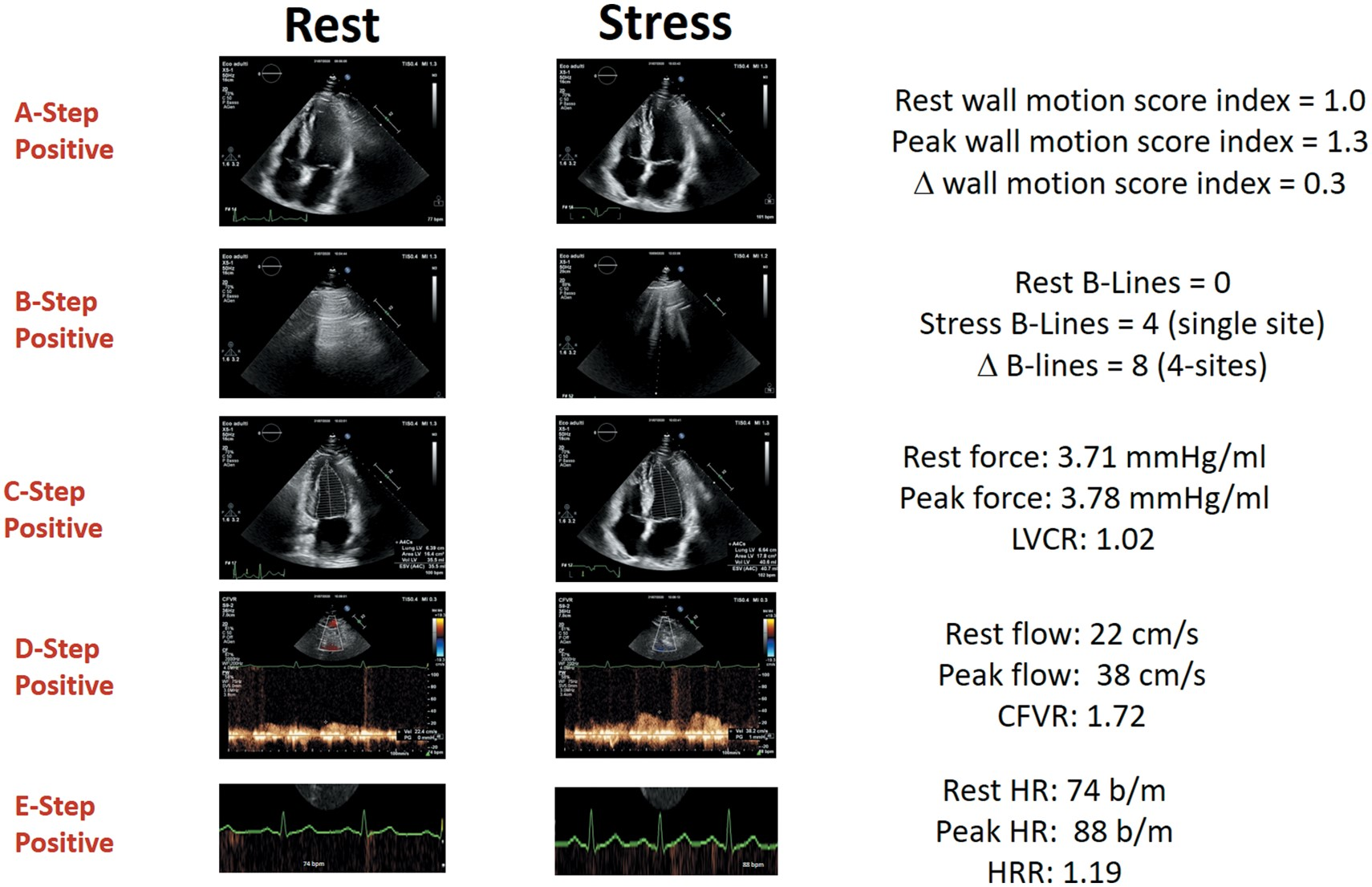
Example: Microvascular Dx
Study
European Heart Journal 2021
Ciampi et al.
Prognostic value of stress echocardiography assessed by the ABCDE protocol
Predictors of Mortality
-
Postive:
- B-lines
- Coronary flow velocity reserve
- Heart rate reserve
- ABCDE Score 3 or greater
-
Negative:
- Regional Wall Motion Abnormalities
- Left ventricular contractile reserve
- The mortality rate was 0.4%/year for a normal SE compared with 2.7%/year when all SE steps were abnormal.
Stress Echo 2030

ABCDE + F (regurgitant flow) G (LVOT gradients) L (left atrial volume/function) P ( pulmonary and LV pressures) L (RV function)
Practical Summary
- Patients are becoming more complex
- Canadian health care focuses on tech that provides value
- Stress Echo is a relatively inexpensive tool and we are currently not harnessing its full potential
-
Patients to consider extended stress echo protocols:
- Angina/ischemia with normal coronories (LAD flow)
- Unexplained dyspnea (Diastolic stress test with B-lines)
- High risk patients - further risk stratify (ABCDE protocol)
Ultrasound Enhancing Agents (UEAs)
- Stress echo is dependent on endocardial resolution and UEAs dramatically increases visualization
- Lipid microbubbles (unrelated to CT/MRI contrast)
- Contraindications:
- Hypersensitivity reaction to previous UEA or PEG
- Practical Summary:
- Academic hospital labs use UEA for the majority of patients, but workflow allows ad hoc usage
- Clinics need to plan time for contrast (if not ordered may not use)
- Unless known excellent images, recommend order with contrast and if issue, clinic will not use it
Perfusion Imaging 2025
SPECT
- Still the foundation of myocardial perfusion imaging
- Relatively cheaper (compared to PET)
- Readily available
- Calcium assessment*
- Significant advances in the technology
- Digital SPECT (no longer UNCLEAR medicine)
- Lower radiation
- Multiple positions
- Quicker scan times
- Most non-hospital clinics use DSPECT
- Digital SPECT (no longer UNCLEAR medicine)
Radiation
ASNC Board Review Course
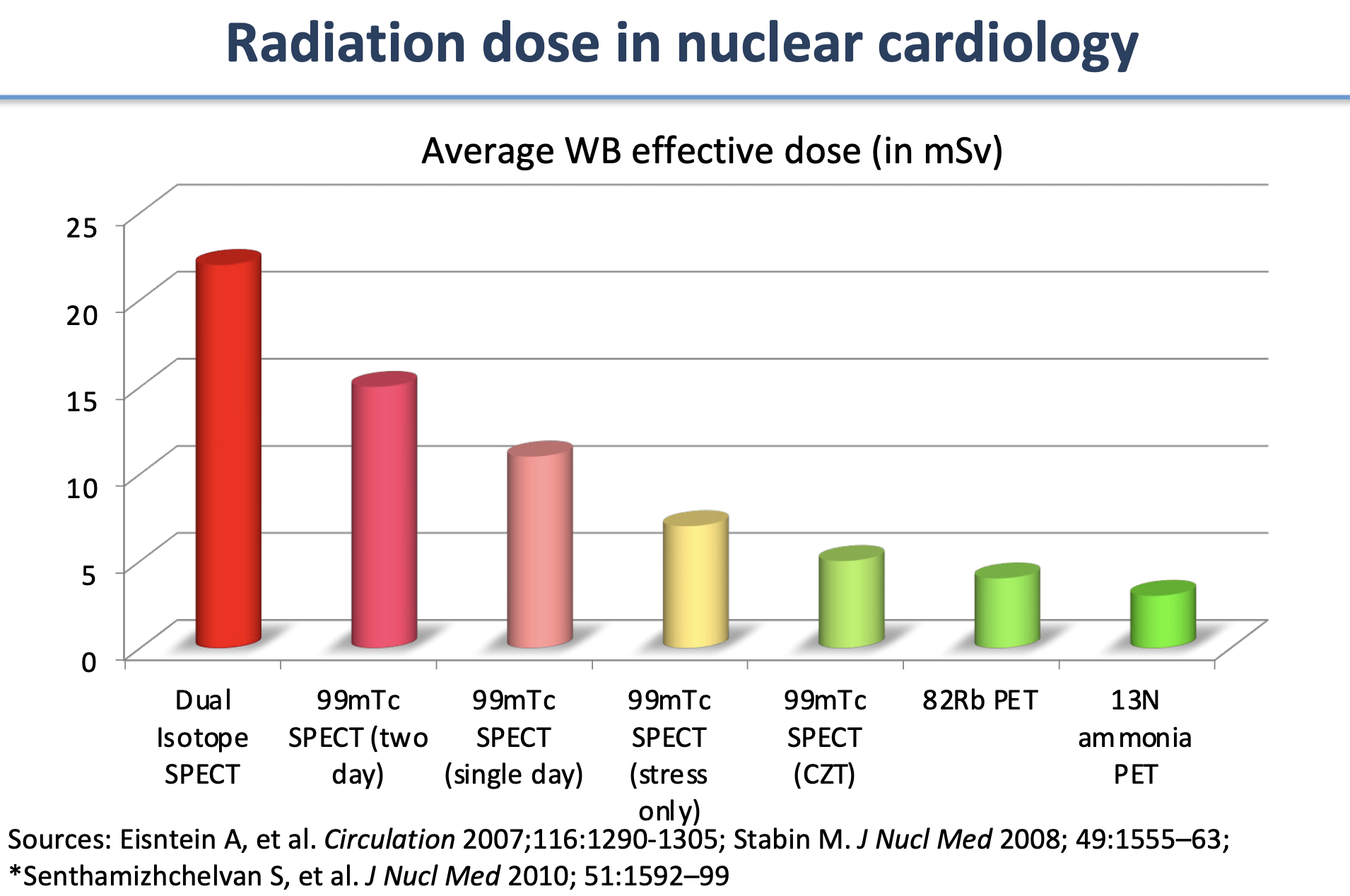
Average annual dose from natural background radiation in Canada is 1.8 mSv. A typical chest CT scan is 7 mSv.
Example
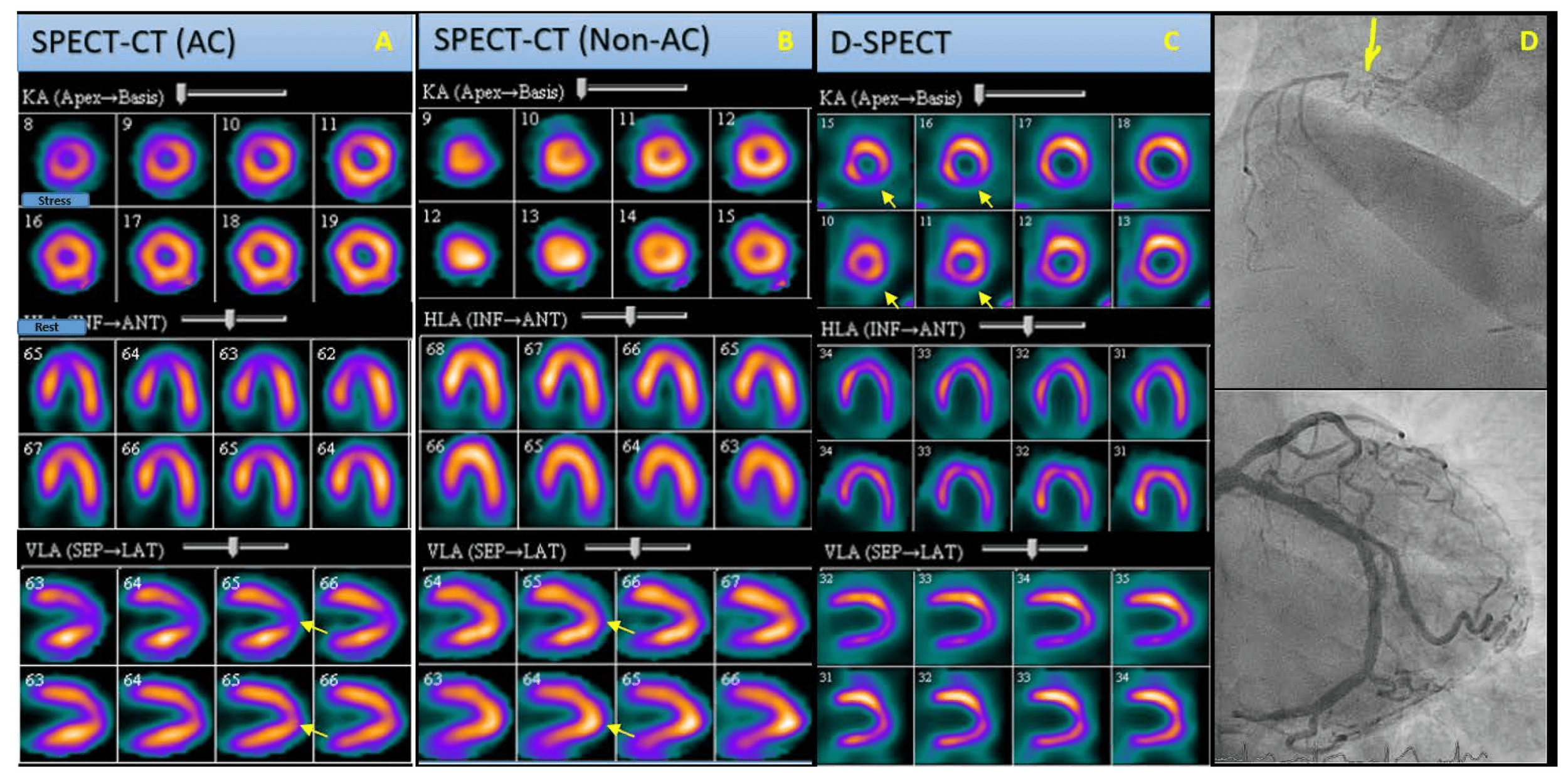
https://www.mdpi.com/2075-1729/13/9/1879
Cardiac PET
Why PET
- Higher diagnostic accuracy
- Consistent high image quality, independent of patient characteristics (ie. increased BMI)
- Reduced study times
- Lower radiation exposure
- Myocardial blood flow quantification
- Always calcium assessment
Why Not PET
- More expensive
- No exercise (currently, but will be possible soon)
- Low accessibility (geography and radioisotope factors)
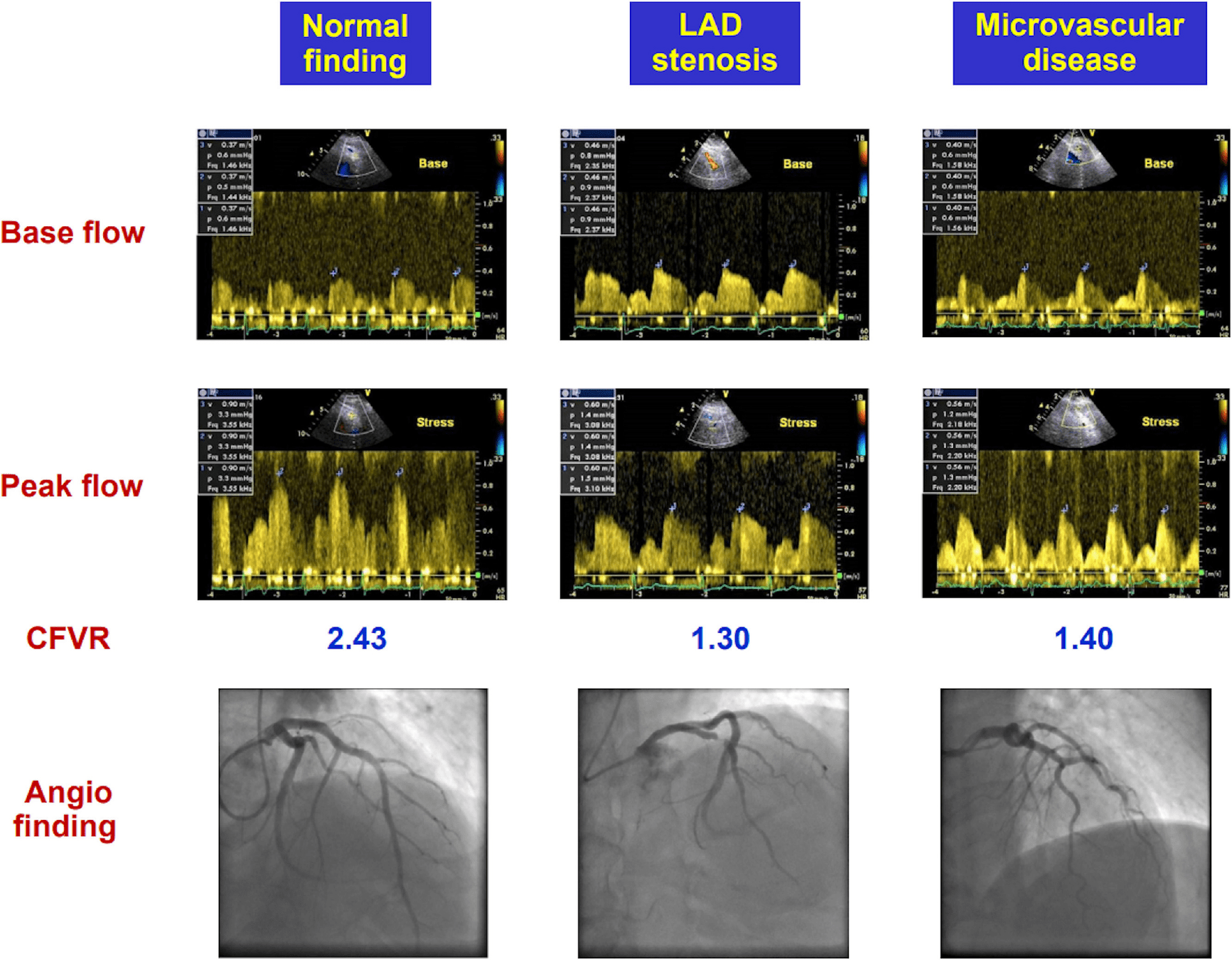
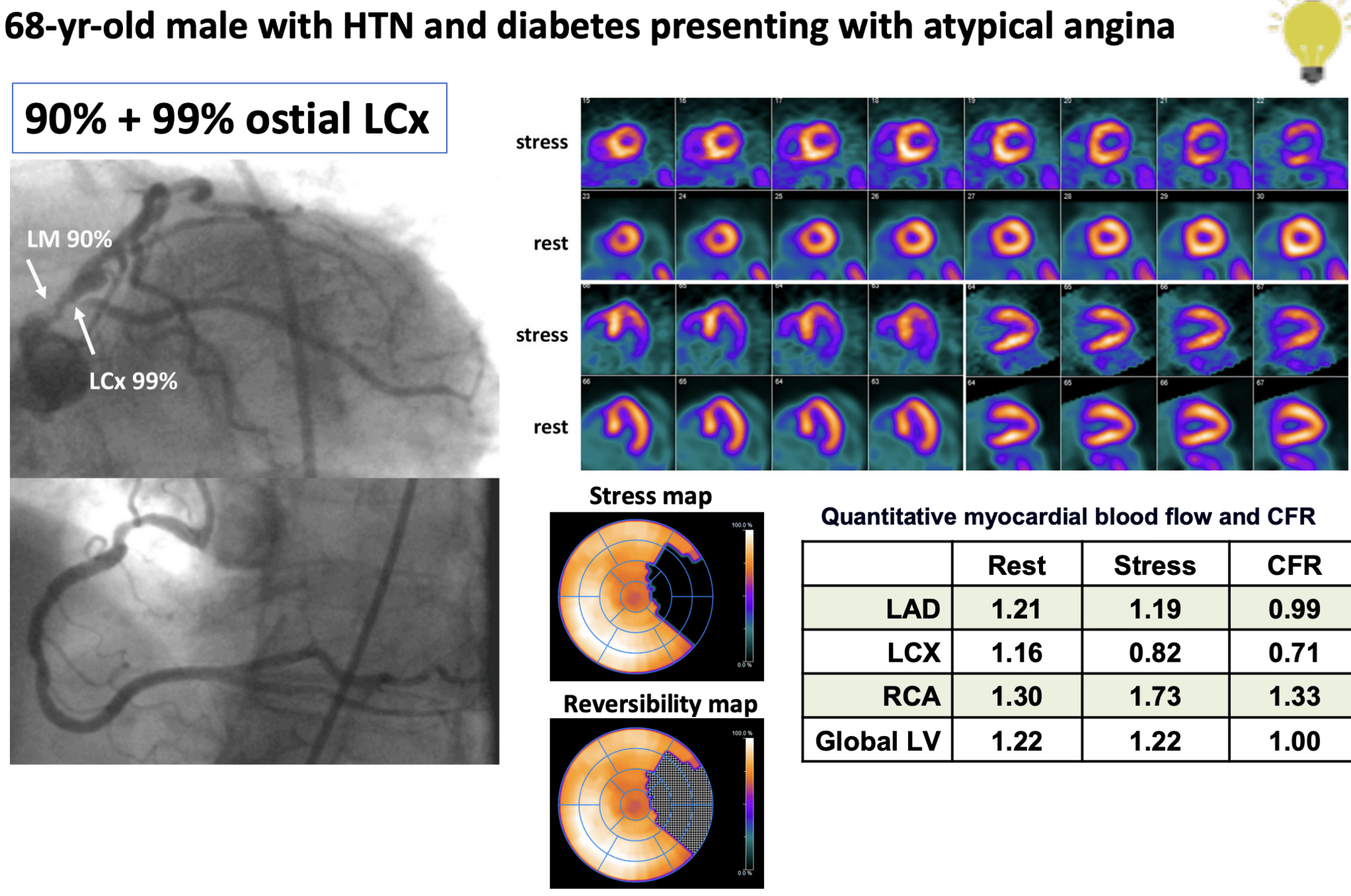
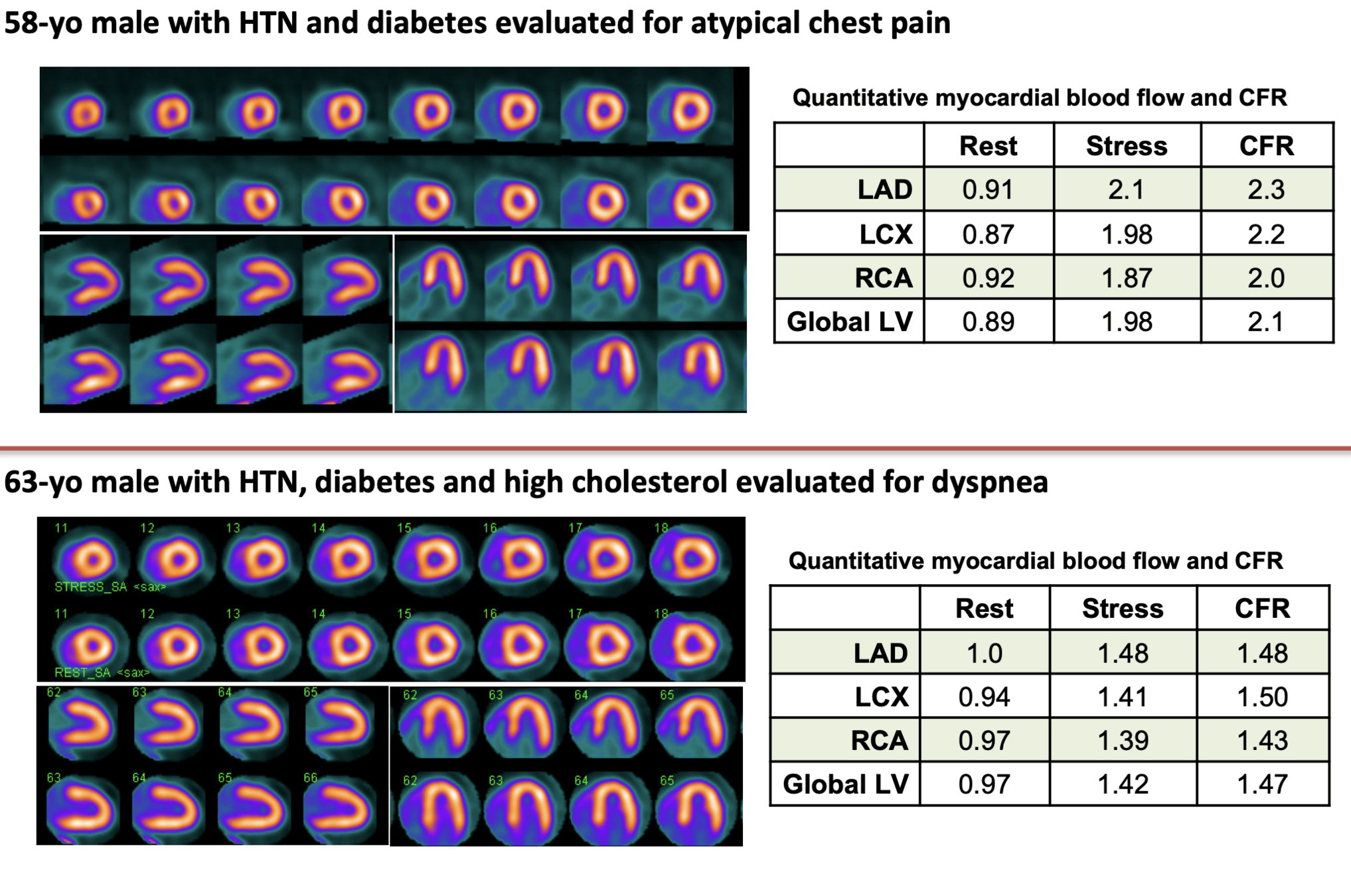
Myocardial Blood Flow
- Absolute quantification of blood flow through the coronary arteries
- Rather than perfusion imaging which is a relative assessment
- Measure blood at rest, stress and calculate relative change (reserve)
- Gives more confidence for obstructive CAD as there should be paired perfusion defect AND reduced blood flow
- Allows diagnosis of other endotypes of coronary disease
- Microvascular disease
Classic Examples
- Obstructive CAD
- Perfusion Defect
- Decrease in blood flow (stress, reserve, and +/- rest)
- Calcium on CT
- Abnormal cath
- Microvascular Disease
- Normal/abnormal perfusion
- Decrease in stress blood flow relative to rest
- No calcium on CT
- Normal cath
Example - Obstructive CAD
ASNC Board Review Course
Example - Normal Perfusion
ASNC Board Review Course
Practical Summary
- PET is expensive and not readily accessible but is a very high quality diagnostic tool
- Canada is fortunate as Cardiac PET is expanding across the country
-
Patients to consider Cardiac PET:
- Angina/ischemia with normal coronories
- Need to minimize radiation dose
- Cardiovascular Implantable Electronic Device Infections
- Query sarcoid
- High-risk patients - further risk stratify
Coronary CT
Why CT
- Anatomic test
- Even if non-obstructive, additional knowledge of atherosclerosis can guide risk factor treatment
- Relatively quick acquisition
- New protocols have relatively low radiation
- Evidence in low risk patients and higher
- Complementary test to functional imaging
- Non-invasive
Why Not CT
- Long wait times (up to one year unless private)
- No functional assessment
- IV contrast needed
Practical Summary
-
Patients to consider Cardiac CT:
- Postive function tests (Stress Echo/Nuclear)
- Rule out Left Main/Multivessel Disease which has evidence to intervene regardless of symptoms
- Assess for false positives
- Postive function tests (Stress Echo/Nuclear)
-
Patients NOT to consider Cardiac CT:
- Patients who likely need intervention
- High-risk stress tests
- Symptoms despite GDMT
- Long wait times not appropriate
- Patients who likely need intervention
Thank you
Questions?