IM AHD
Atul Jaidka
Outline
- Valve 2020 Guidelines
- Afib 2020 Guidelines
- ECG
Valvular Disease
Case
You are seeing a 78 year old female in your outpatient General Internal Medicine clinic for 1 year of progressive shortness of breath. History and physical are otherwise unremarkable but you hear a 2/6 systolic murmur heard throughout the precordium. How do you workup this patient?
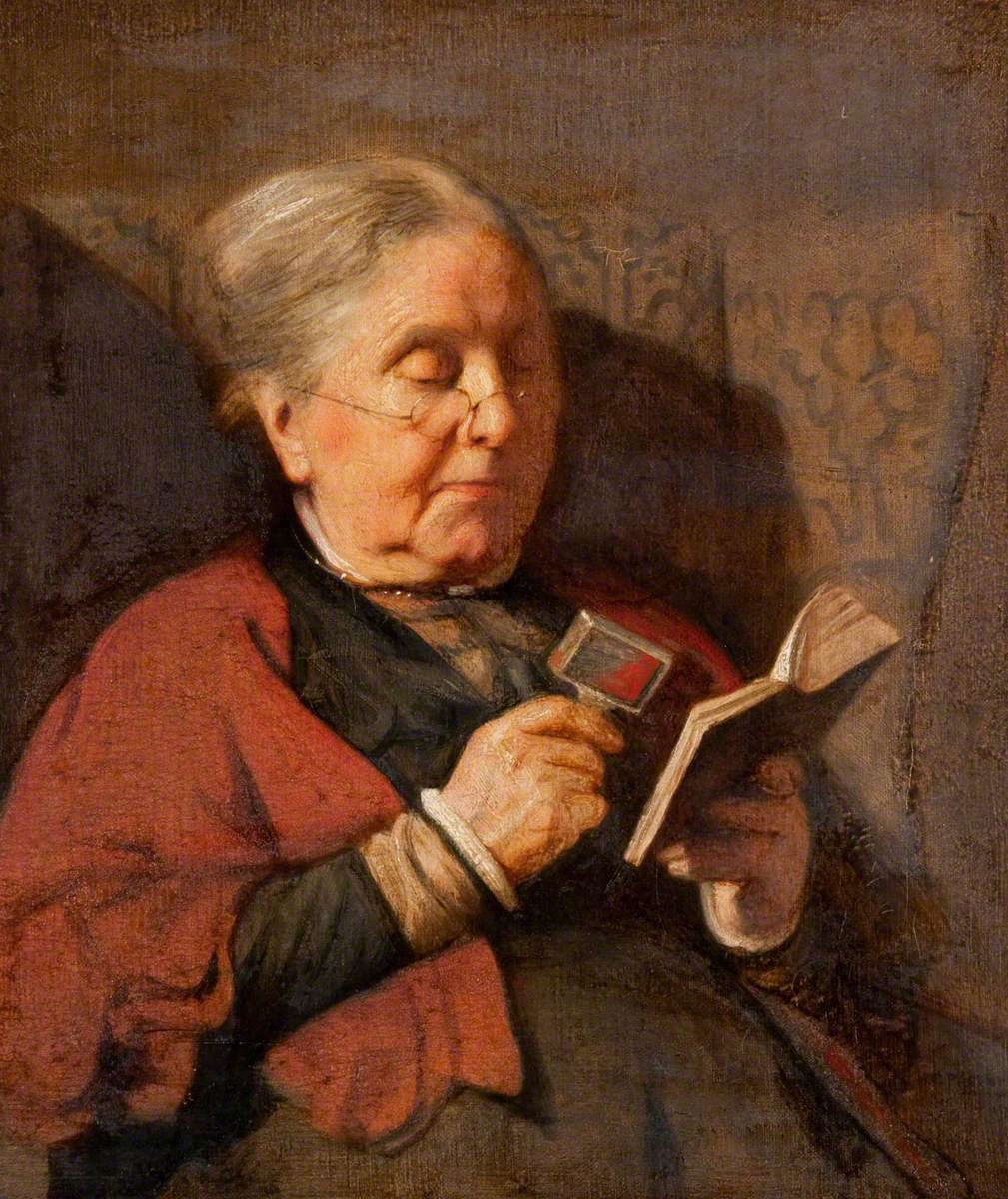
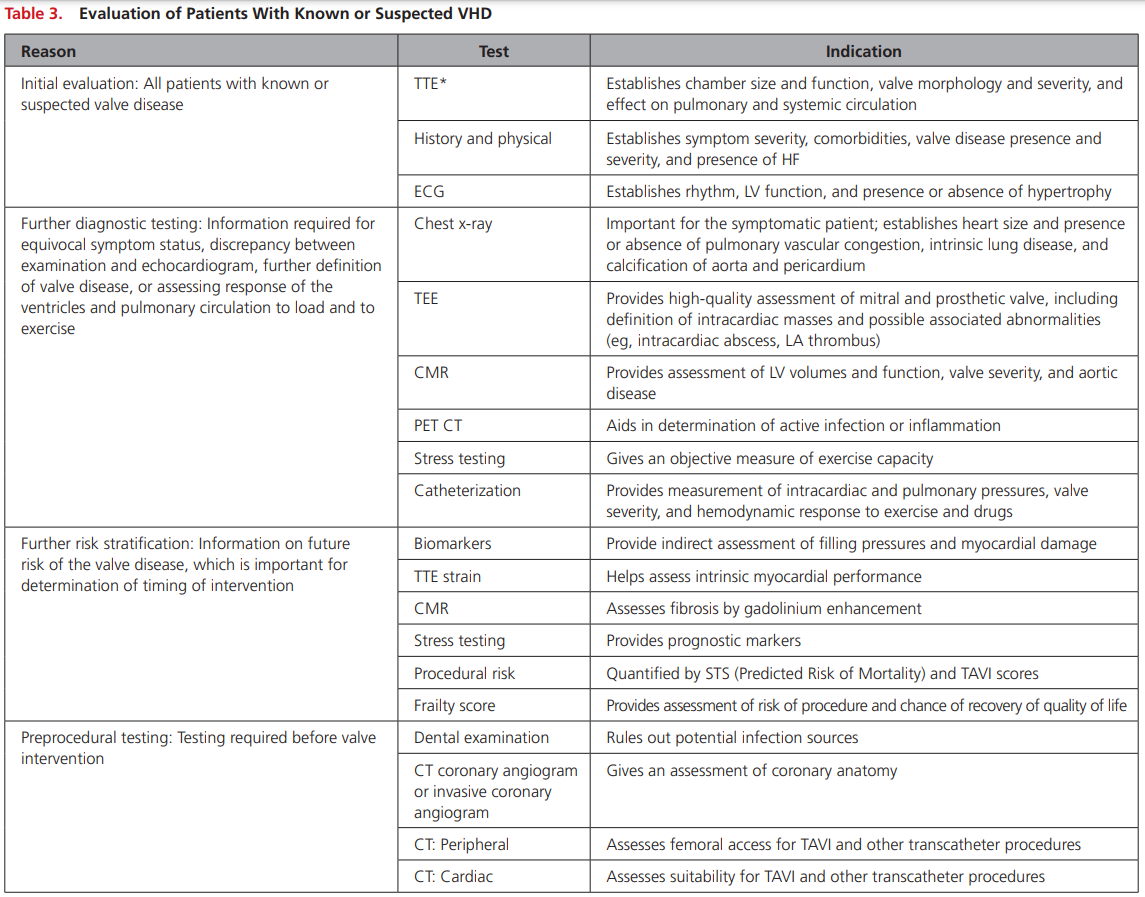
Workup
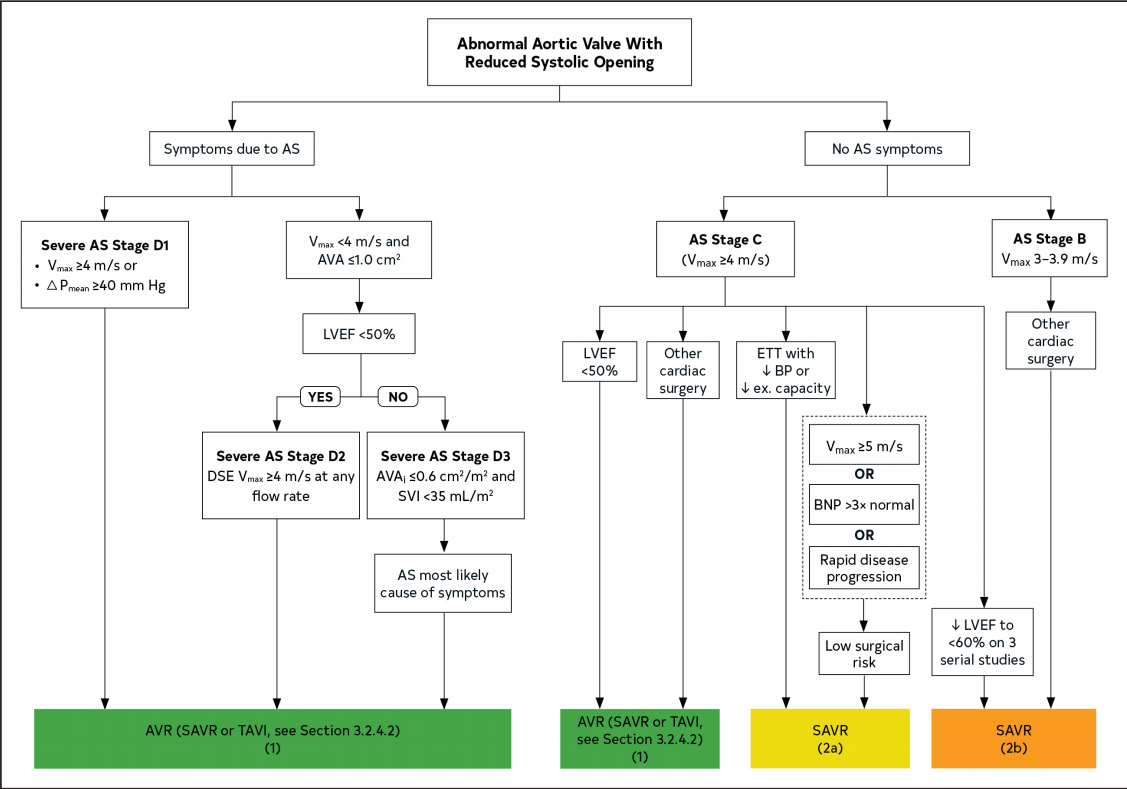
Case
Transthoracic Echo:
- Severe valvular aortic stenosis
- Left atrium is moderately dilated
- Ejection Fraction >70%
- Left ventricular size is normal.
- Mild concentric hypertrophy
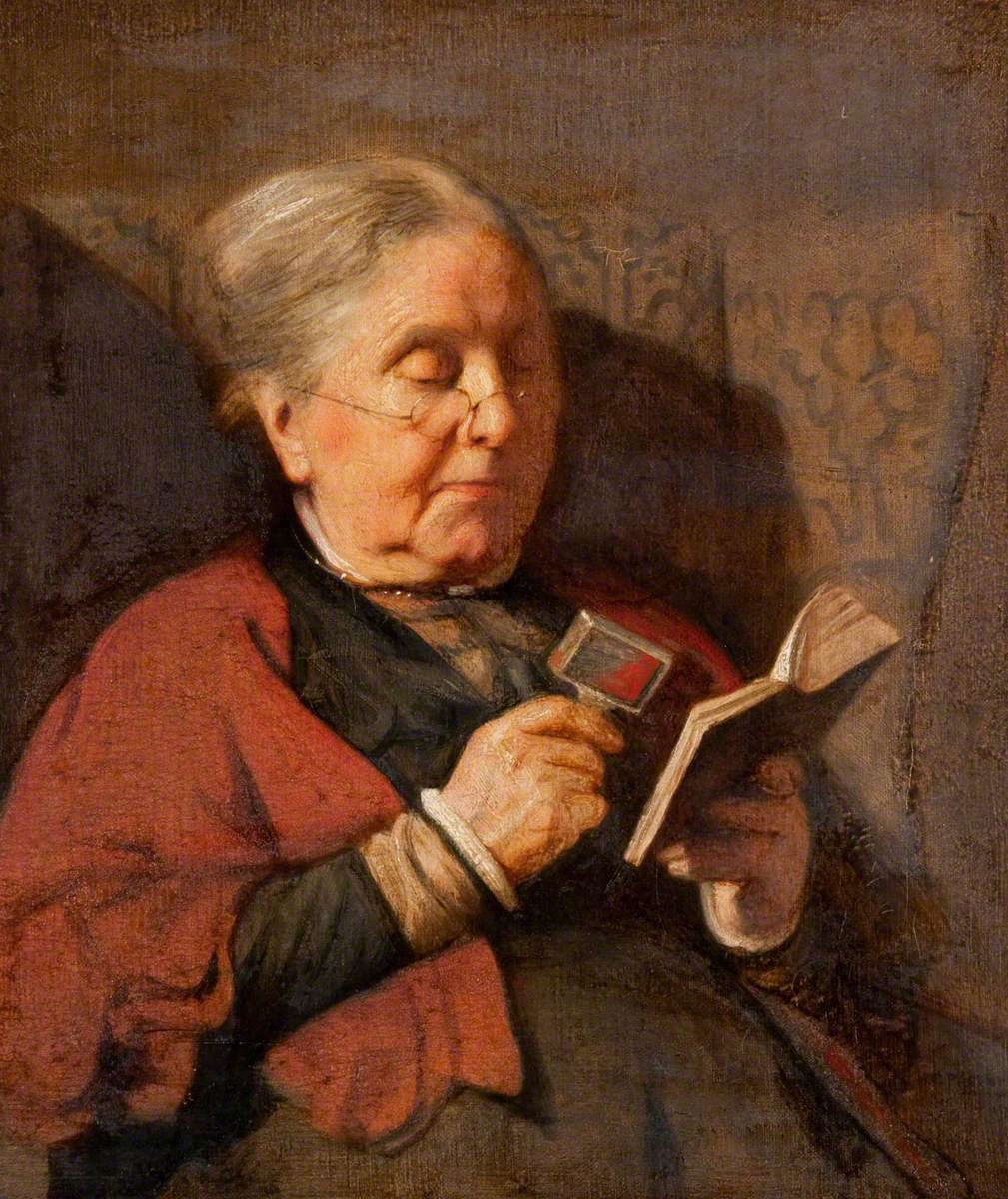
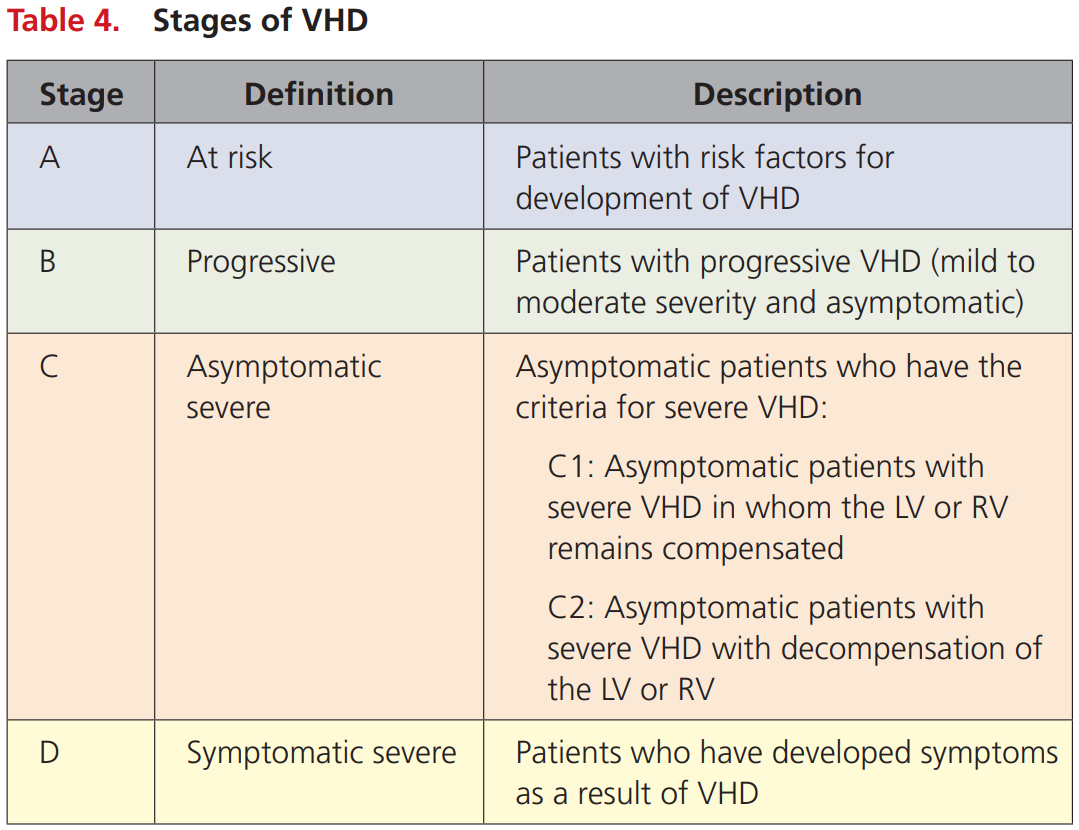
How would you stage this patient?
Stages
What is severe AS?
Severe AS
- Aortic Vmax ≥4 m/s or mean ∆P ≥40 mm Hg
- AVA typically is ≤1.0 cm2 (or AVAi 0.6 cm2 /m2 ) but not required to define severe AS
- Very severe AS is an aortic Vmax ≥5 m/s or mean P ≥60 mm Hg
Case
Given the recent echocardiographic findings, how will you manage this patient?
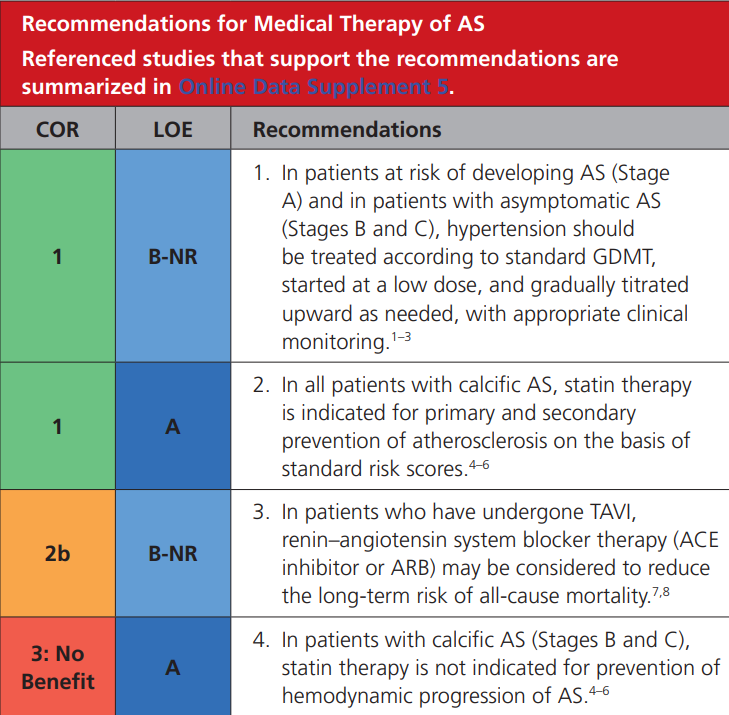
Ace Inhibitor?
Ace Inhibitor
- Actually has evidence of benefit before and after AVR
- Start low and go slow
Review article: https://www.ahajournals.org/doi/pdf/10.1161/JAHA.120.016911
Case
How will you decide if she is a candidate for intervention and what intervention should she get?
Assess Risk/Frailty
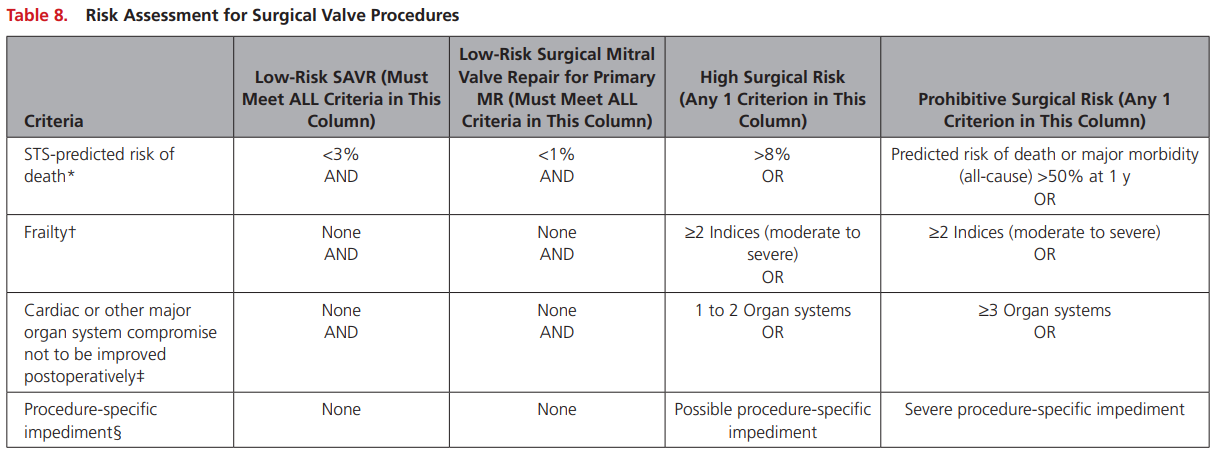
*Risk can be assess with STS or EUROSCORE II
†Assess by ADLs or score (ie. FRAILTY-AVR 4 point score)
Note: don't memorize scores but understand what the contain
Text
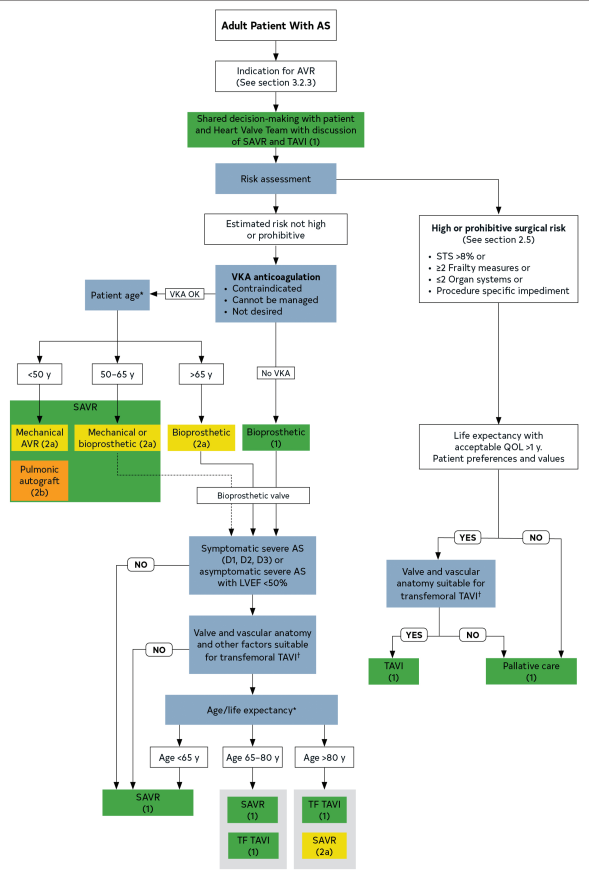
TAVI/SAVR
- GIM goal should be to refer patients to a multi-disciplinary Valve team
- TAVI for sure if high risk or frail
- SAVR for sure if not high risk and <65
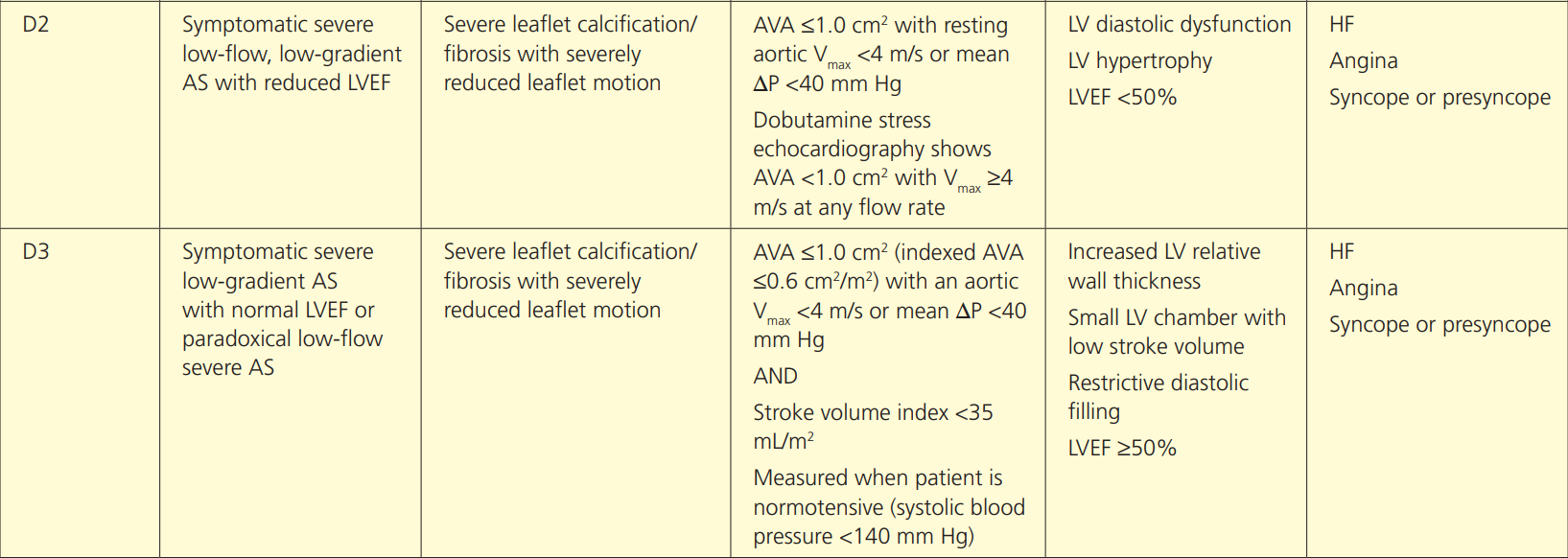
Low Flow Low Gradient Aortic Stenosis
Low flow low graident AS
- Know it exists and the theory
- Determine by dobutamine stress echo
- Don't need to know cutoffs etc
Case
You are seeing her in clinic for new onset of palpitations while waiting for TAVI and Holter monitor shows atrial fibrillation. How will you manage her new diagnosis?
Anticoag and AF
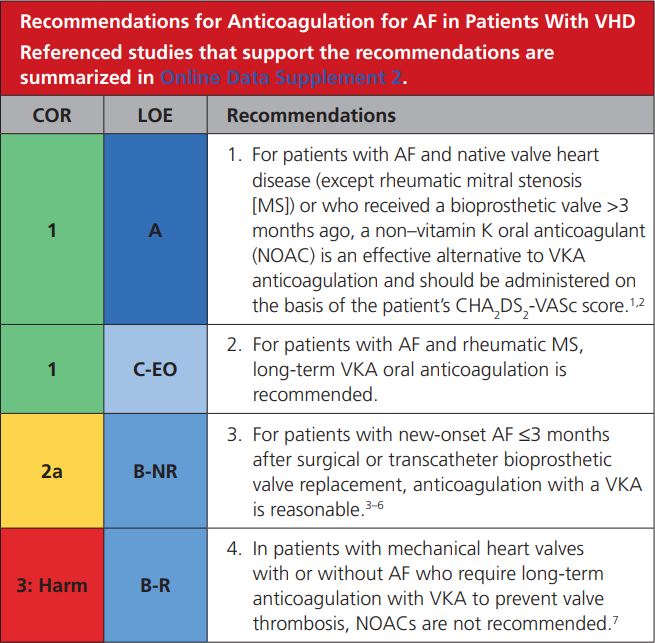
Guideline Standoff

CCS always wins. CCS Afib 2020:
"The current definition of “valvular AF” is limited to AF in the presence of any mechanical heart valve, or in the presence of moderate to severe mitral stenosis (rheumatic or nonrheumatic)."
Case
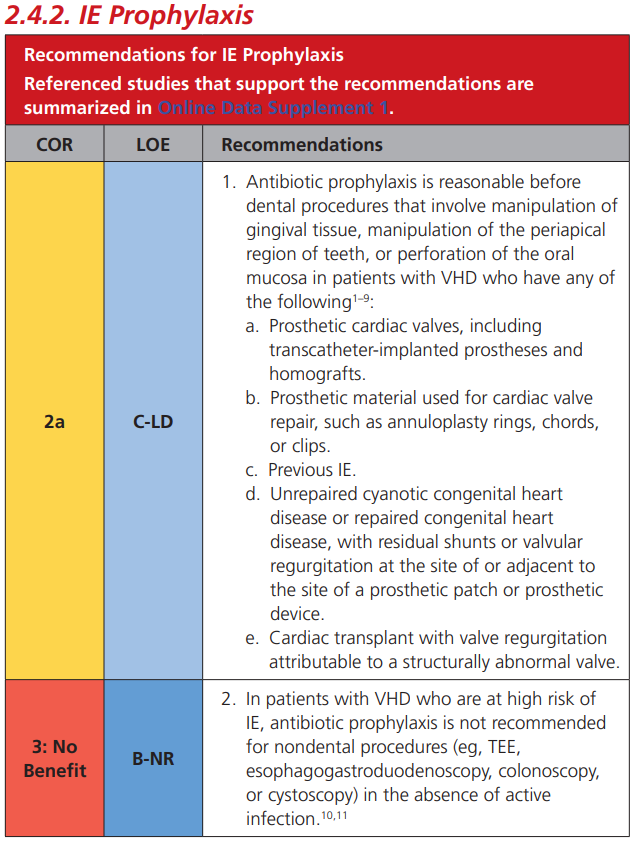
You are seeing her in clinic 1 year after her TAVI and he remembers the TAVI coordinator saying something about antibiotics before certain procedures. How will you counsel her?
IE Prophylaxis
Aortic Regurgitation
Acute AR
- Generally not managed by IM
- Surgical emergency and should not be delayed by medical therapy
Chronic AR
- Bicuspid and aortopathy most common causes
- Medical therapy: treat hypertension
- ACE/ARB/ARNI recommended
- Surgery (Class 1):
- severe + symptomatic
- Asymptomatic + EF<55% or other cardiac surgery
- Lower grade for asymp + dilated LV
Mitral Regurgitation
Acute MR
- Caused by ischemia, IE
- Surgical emergency
- Medical temporizing
- IABP
- Afterload reducing agents
Chronic MR
- Primary
- problem with valve
- Ie. myxomatous
- Secondary (functional)
- due to LV dilation
- Primary MR: no class 1 medical therapy
- don't delay surgery
- treat LV dysfunction with GDMT
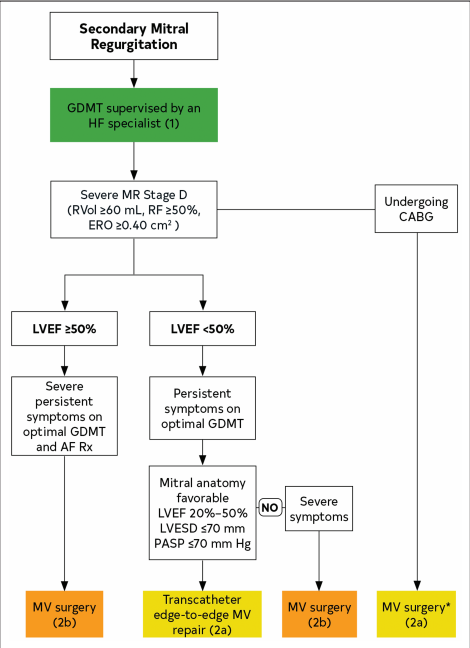
- Secondary MR:
- treat with GDM and HF specialist
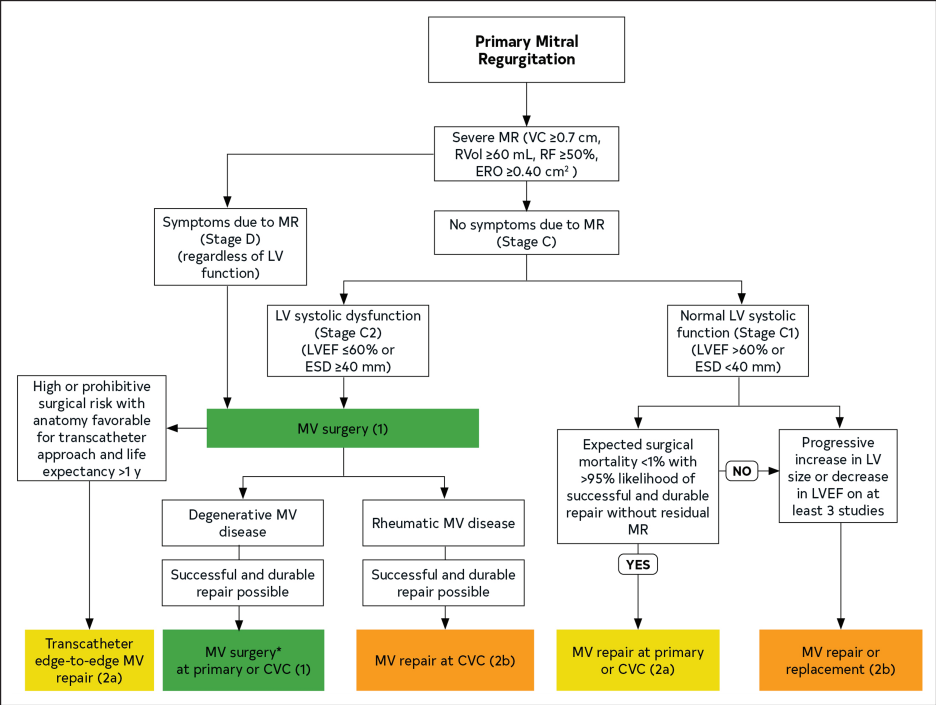
Primary MR
- Severe + symptomatic
- regardless of LV function
- Severe + asymptomatic + LV dysfunction (LVEF <60 or LVESD > 40mm)
Secondary MR
- No Class 1 intervention
- Focus on GDMT including CRT and revasc
- Despite max GDMT consider PMVR (mitra-clip) if still symptomatic
Mitral Stenosis
Mitral Stenosis
- Rheumatmic and Degenerative most common
- Anticoag if afib, prior embolic event, LA thrombus
- Control heart rate
- Surgery (Class I)
- Severe + symptomatic
- PMBC or MV surgery (multi-disciplinary team decision)
Tricuspid Regurgitation
- Class 1 Indication for surgery: severe TR and left sided surgery, tricuspid surgery recommended
Summary
Summary
- What do know
- Know physical exam for oral component
- Know Class 1 indications
- Severity criteria (except severe AS) not needed
- Treatment
- Medical: temporizing
- Surgery: effective but risk
- Catheter based: for select patients
- Symptoms
- Classic angina, HF (SOB), and syncope
- Symptom equivalent: LV dysfunction
Atrial Fibrillation
Case
You are seeing a 68 year old male in the emergency medicine department who presents with anxiety. His brother developed atrial fibrillation and he is wondering whether he should have screening. How do you counsel him and if screening is appropriate how would you do so?

Screening

Screening in Stroke
- At least 24 hours of ambulatory ECG monitoring
- Prolonged monitoring in select older patients if AF is still suspected
ECG
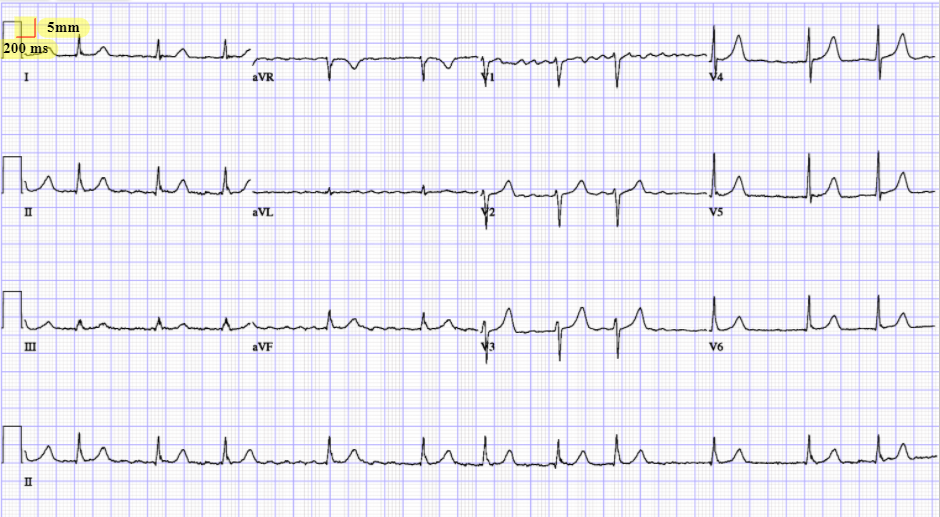
How will you workup this patient in Emerg?
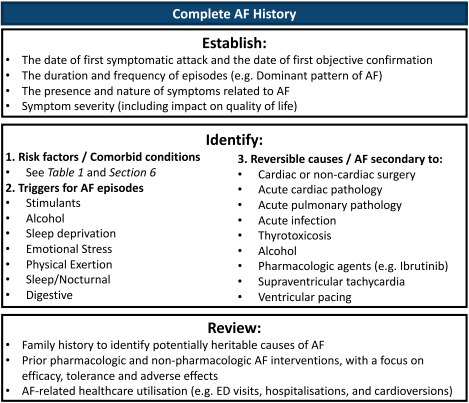
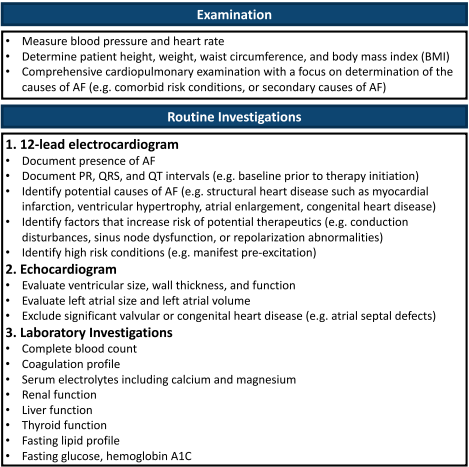
Workup
CCC QoL
- Know the score exists and that you would assess QoL
- Important aspect of outpatient management

Case
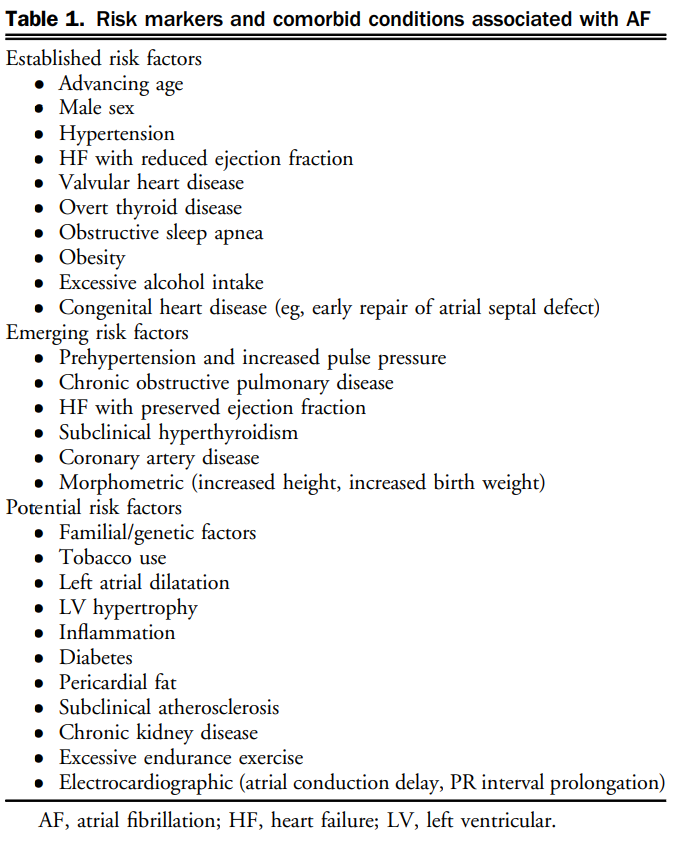
What are risk factors for atrial fibrillation and how would you counsel the patient on modifying them?

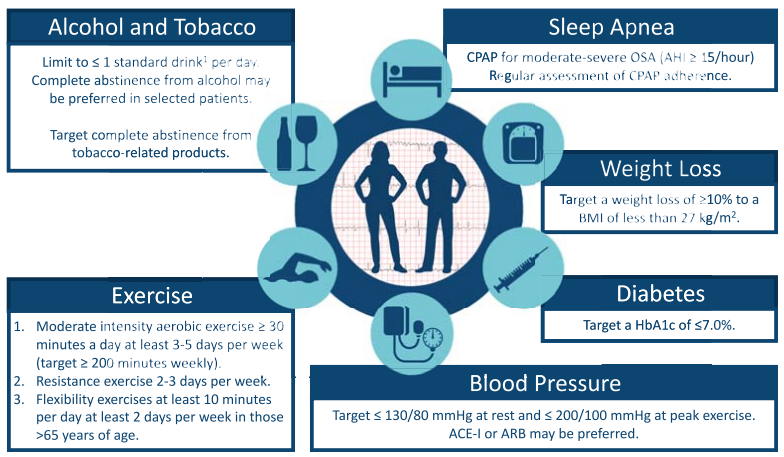
We suggest a structured, integrated, multidisciplinary, patient-focused approach to care should be implemented for patients with AF (Weak Recommendation; Moderate-Quality Evidence).
Risk Factors
Case
You have initiated a multi-disciplinary non-pharmacologic plan for the patient and now move to the pharmacologic component. How will you manage this patient?

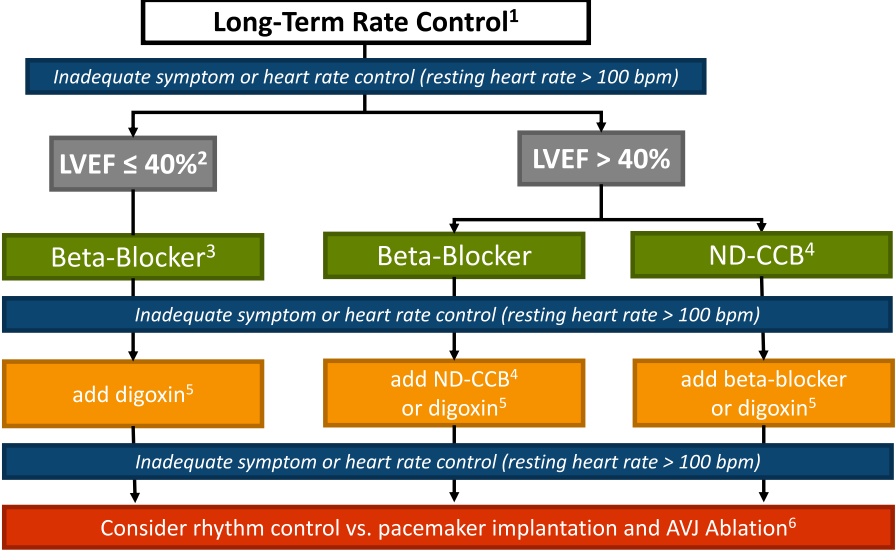
Rate vs Rhythm Control

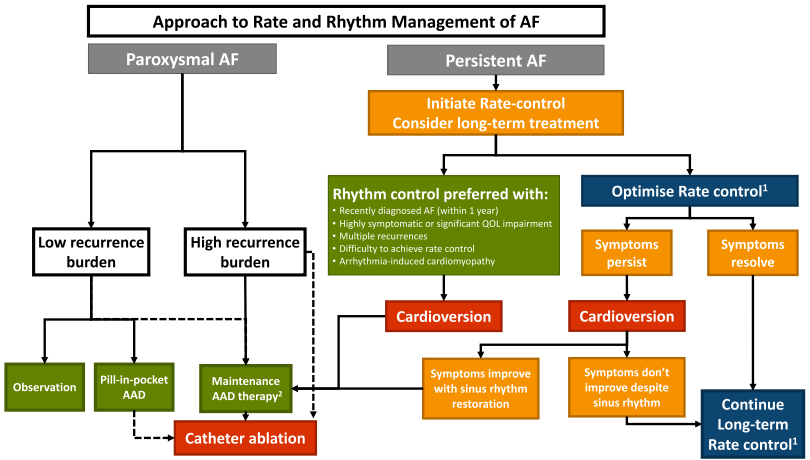
- New recommendation: We suggest that a rhythm control strategy be considered for most stable patients with recent-onset AF
- Evolving evidence, but broadly consider rhythm control in symptomatic, cannot rate control or paroxysmal. Unlikely to have to prescribe.
Anticoagulation
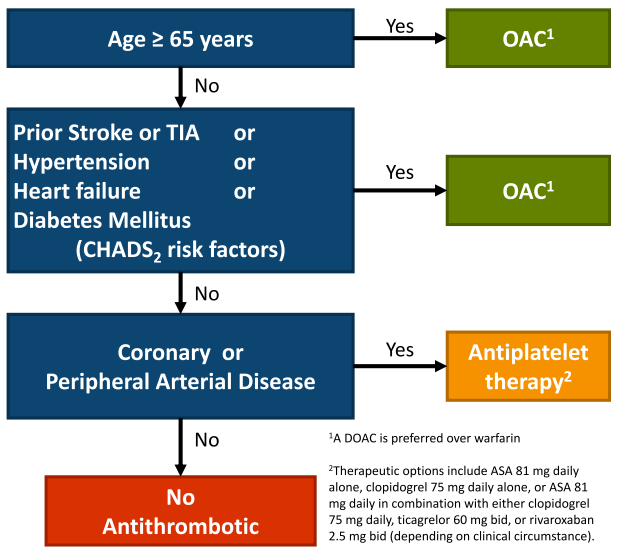
- Note: annual reassessment
- NVAF is defined as AF in the absence of mechanical heart valves or moderate to severe mitral stenosis
Special Circumstances
Renal Failure
- Stage 3 CKD or better (eGFR > 30 mL/min): we recommend that such patients receive antithrombotic therapy as determined by the “CCS algorithm” (YES)
- Stage 4 CKD (eGFR 15-30 mL/min): we suggest that such patients receive antithrombotic therapy as determined by the “CCS algorithm” (YES)
- Stage 5 CKD (eGFR < 15mL/min or dialysis dependent): we suggest that such patients not routinely receive antithrombotic therapy for stroke prevention in AF (NO)
Renal Failure
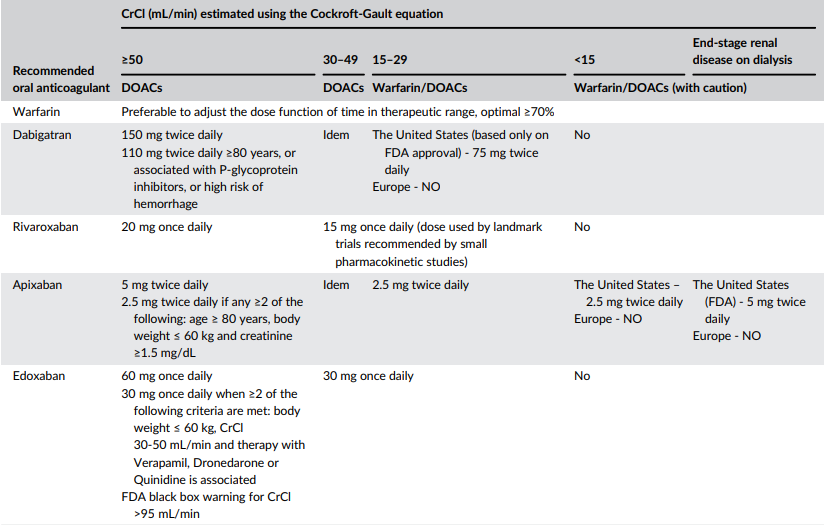
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6671778/
CAD
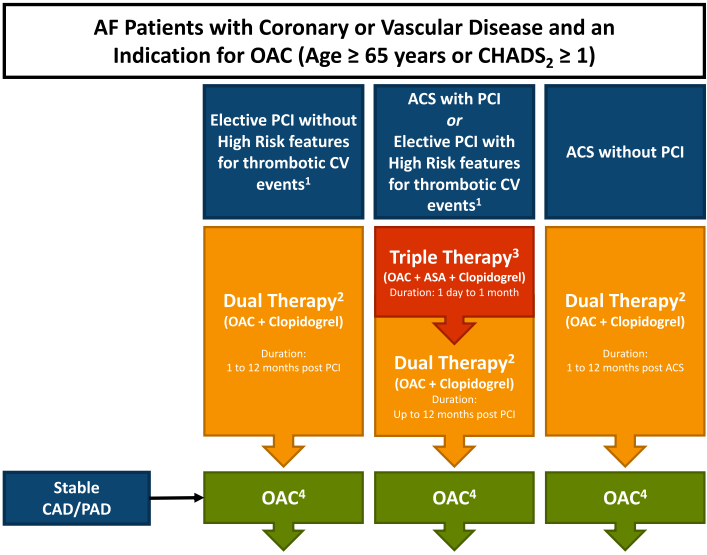
Dual: warfarin, apixiban 5mg, dabigatran 110/150, edoxaban 60, rivaroxaban 15
Triple: warfarin INR 2-2.5, rivaroxaban 2.5, apixaban 5 (DOAC preferred)
Duration of Triple Therapy
- Interventionalist will dictate when
- Balance risk of bleeding to risk of ischemic events
- patients factors, angiographic factors, ACS
- Exam: discuss with Cardiology while weighing risks and benefits
Other Special Populations
-
Liver disease: “We recommend that OAC not be routinely prescribed in Child-Pugh
class C or liver disease associated with significant coagulopathy.” - Cancer: Individualize OAC treatment in pts with active cancer. Consider DOAC> VKA.
-
Frail Elderly
- OAC for most frail elderly – individualizing recommendations if high risk bleed
-
Secondary AF (clearly provoked by a transient/reversible risk factor such as severe sepsis, thyrotoxicosis):
- No OAC:
- Exceptions: patient’s underlying ‘abnormal substrate’ and risk for recurrence estimated to be high
• OAC for “most patients during acute thyrotoxicosis until euthyroid state is restored”
- Exceptions: patient’s underlying ‘abnormal substrate’ and risk for recurrence estimated to be high
- No OAC:
Case
Patient comes back to the emergency department with rapid atrial fibrillation. He is hemodynamically stable. Emergency medicine doctors asks if it is safe to cardiovert. His CHADS65 score is 2 and the symptoms clearly started 16 hours ago. How would you proceed?

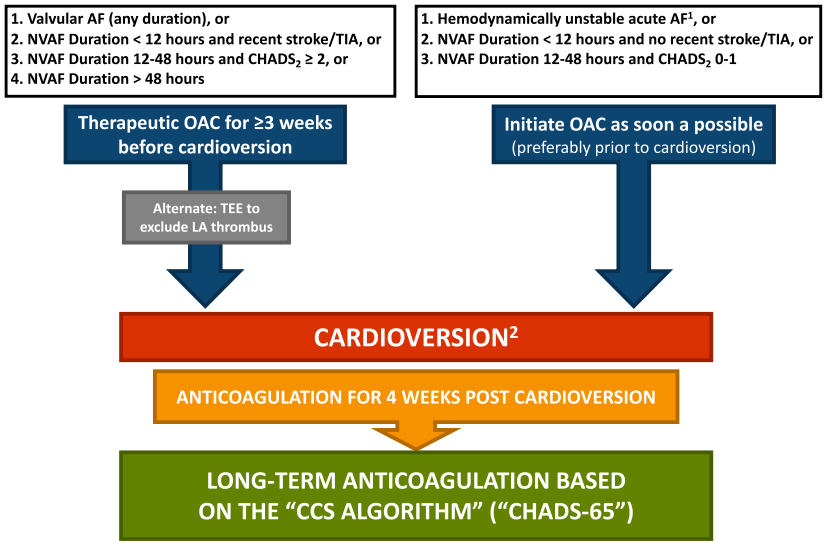
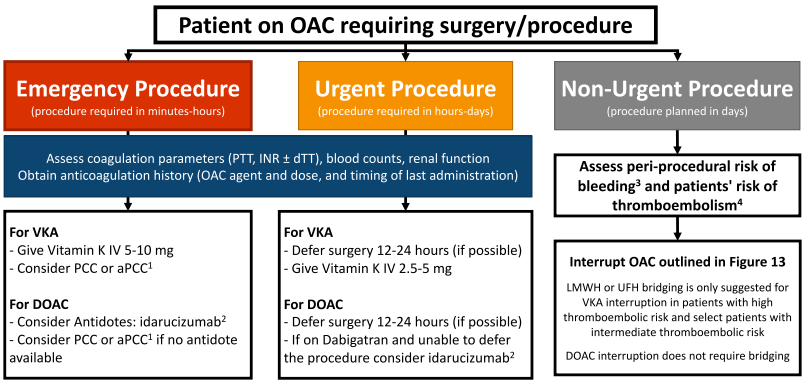
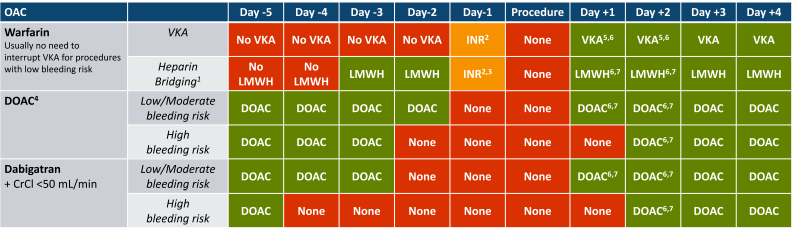
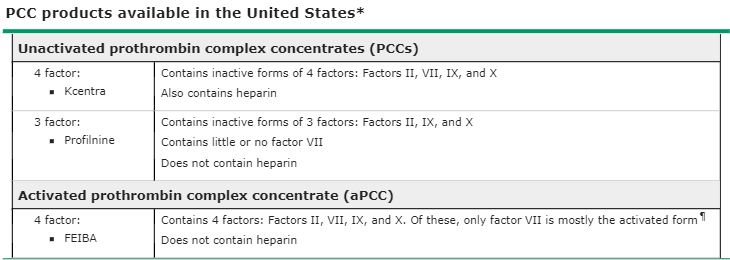
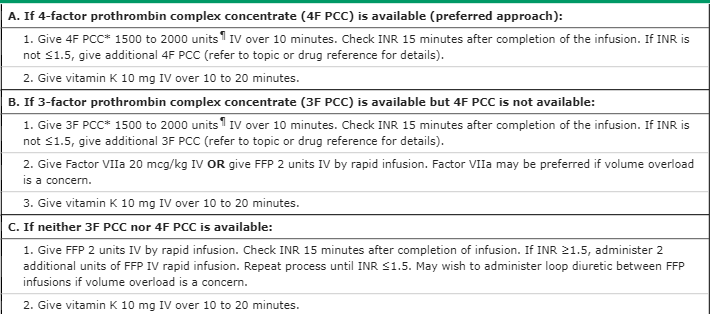
Interrupting Anticoagulation