DOACs - Are These Drugs a Panacea?
Atul Jaidka
Background
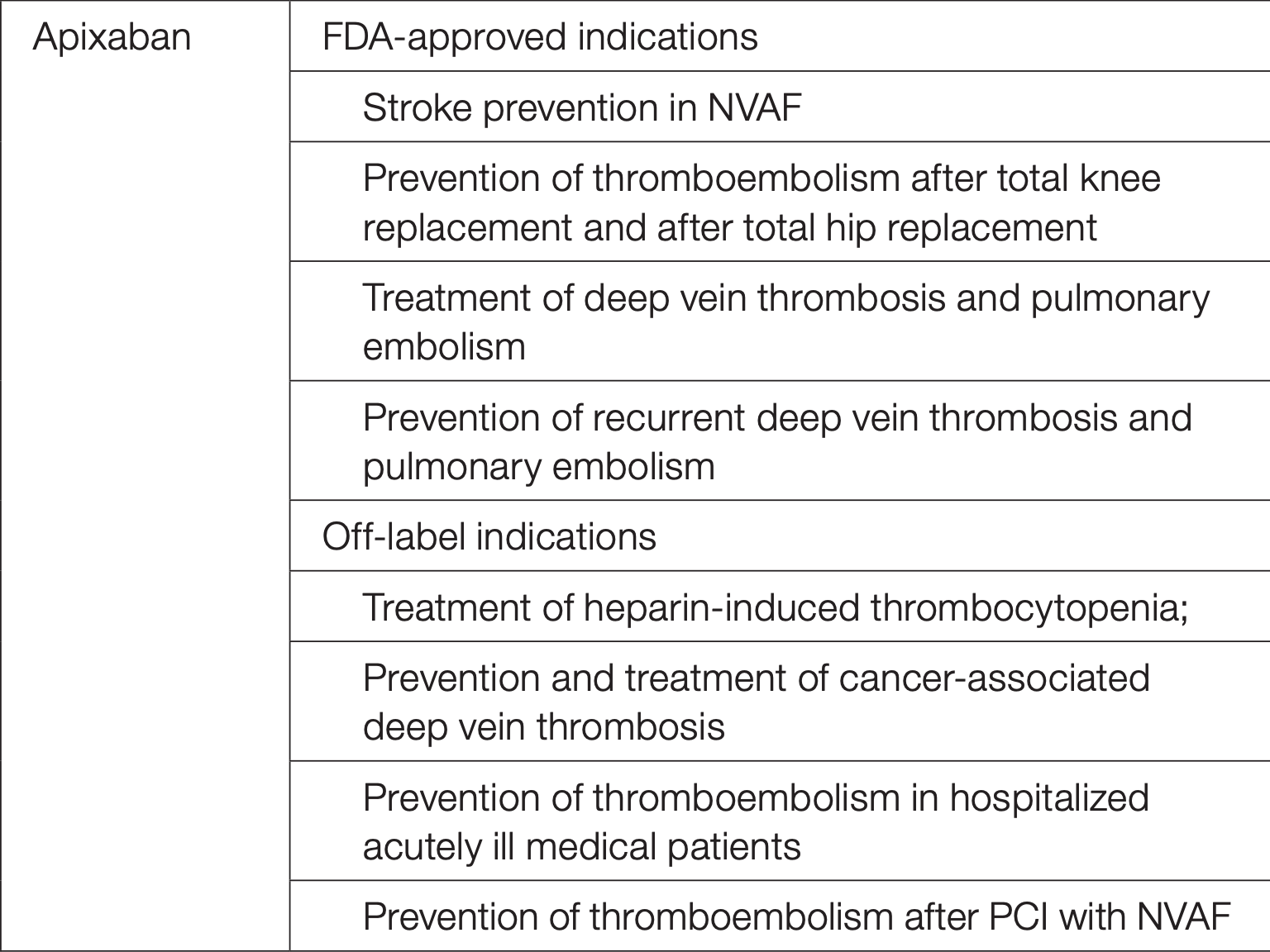
Indications
https://www.ahajournals.org/doi/pdf/10.1161/JAHA.120.017559
Indications
https://www.ahajournals.org/doi/pdf/10.1161/JAHA.120.017559
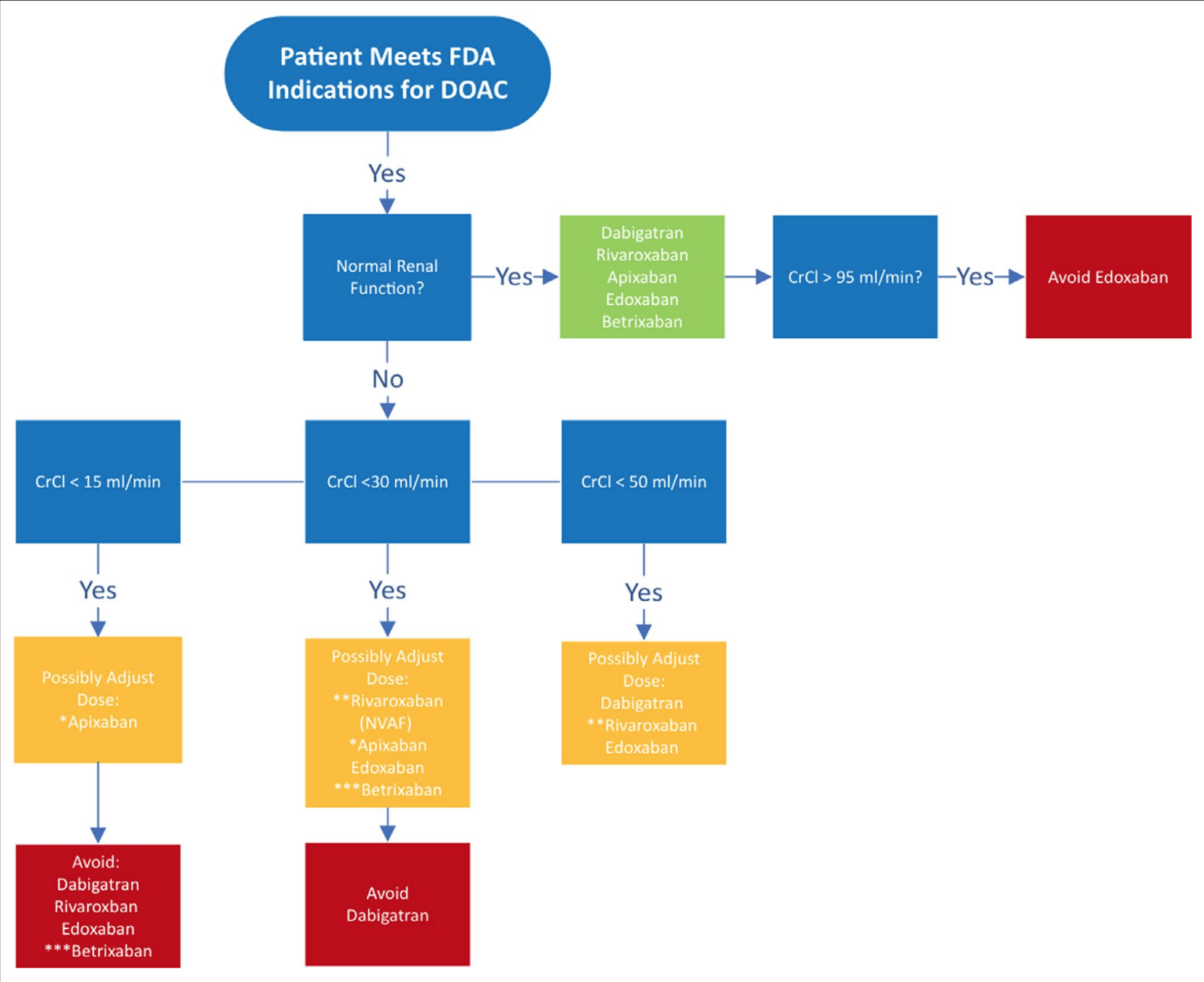
Severe or end-stage renal disease (ESRD) not requiring dialysis: Apixaban or warfarin is considered appropriate (AHA/ACC/HRS [January 2014]; AHA/ACC/HRS [January 2019]). Some experts recommend apixaban 2.5 mg twice daily for CrCl 15 to 29 mL/minute (ACCP [Lip 2018]).
Indications
https://www.ahajournals.org/doi/pdf/10.1161/JAHA.120.017559
Not Indicated

-
The use of dabigatran in patients with mechanical heart valves was associated with increased rates of thromboembolic and bleeding complications, as compared with warfarin, thus showing no benefit and an excess risk.
Not Indicated

-
Direct anticoagulants are currently used in patients with thromboembolism, irrespective of the presence of antiphospholipid antibodies.
-
This trial shows an increased rate of events with rivaroxaban compared with warfarin in patients with antiphospholipid syndrome.
DOACs
Panacea
???
LV Thrombus
LV Thrombus
LV Thrombus
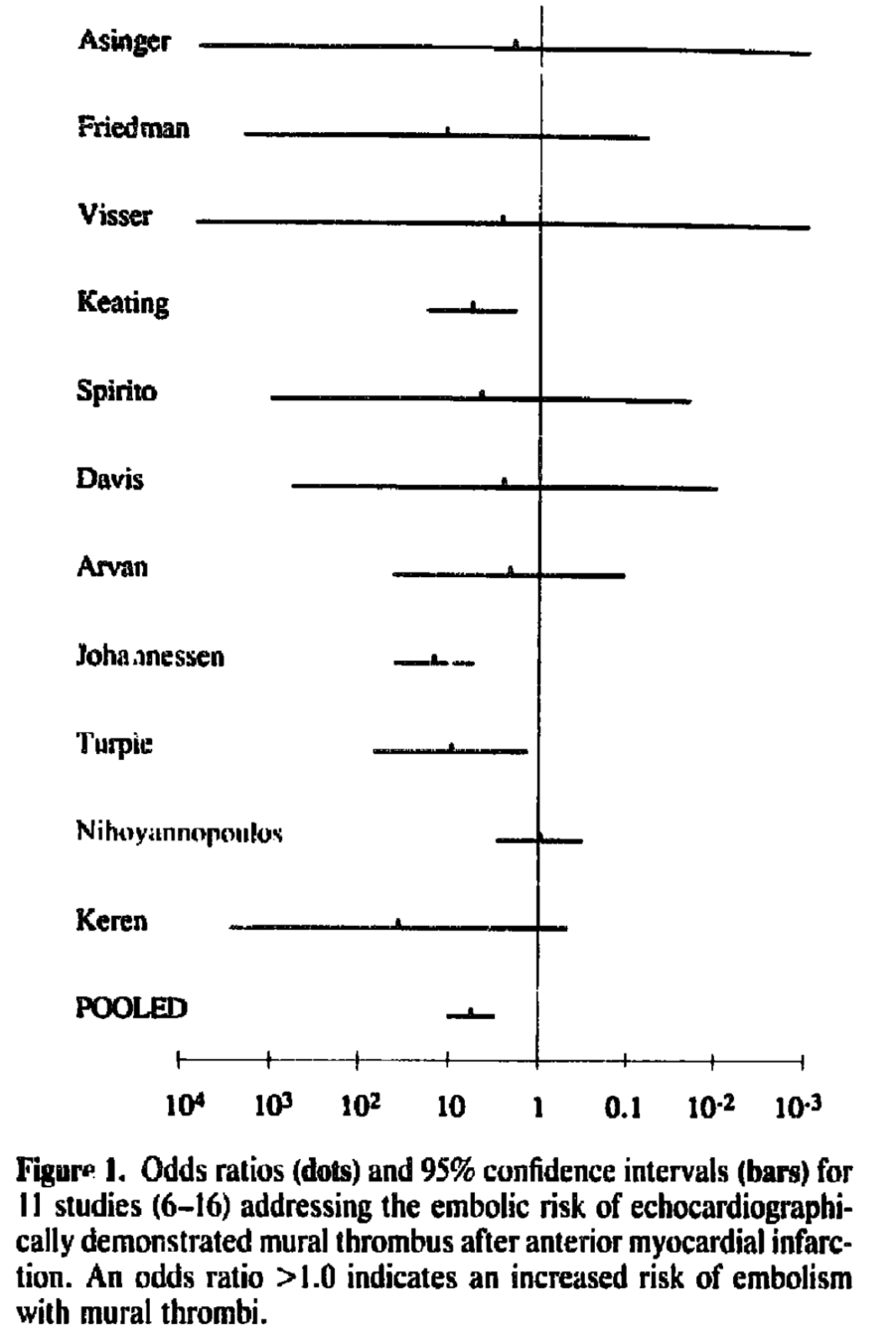
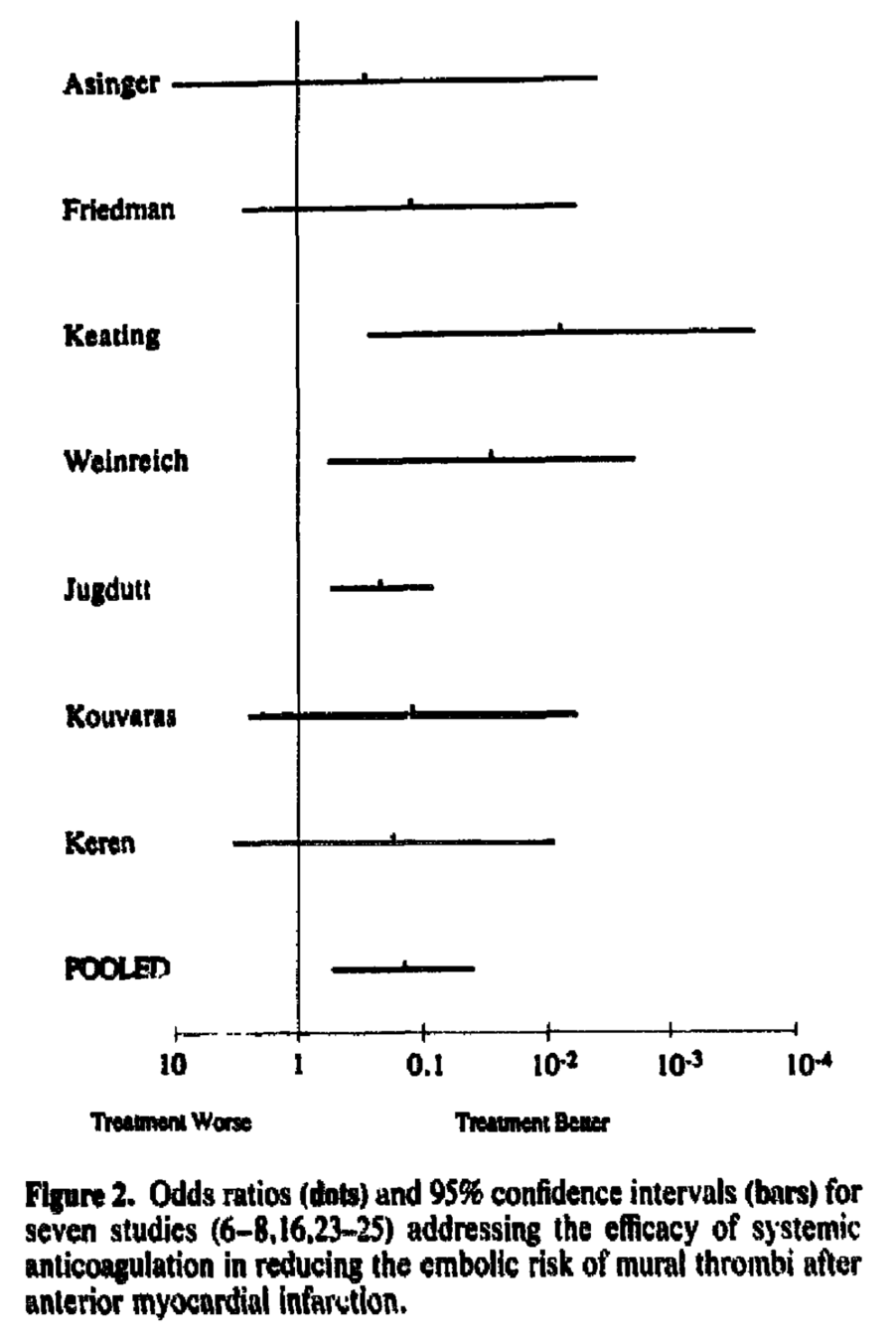
Most Rigorous Data
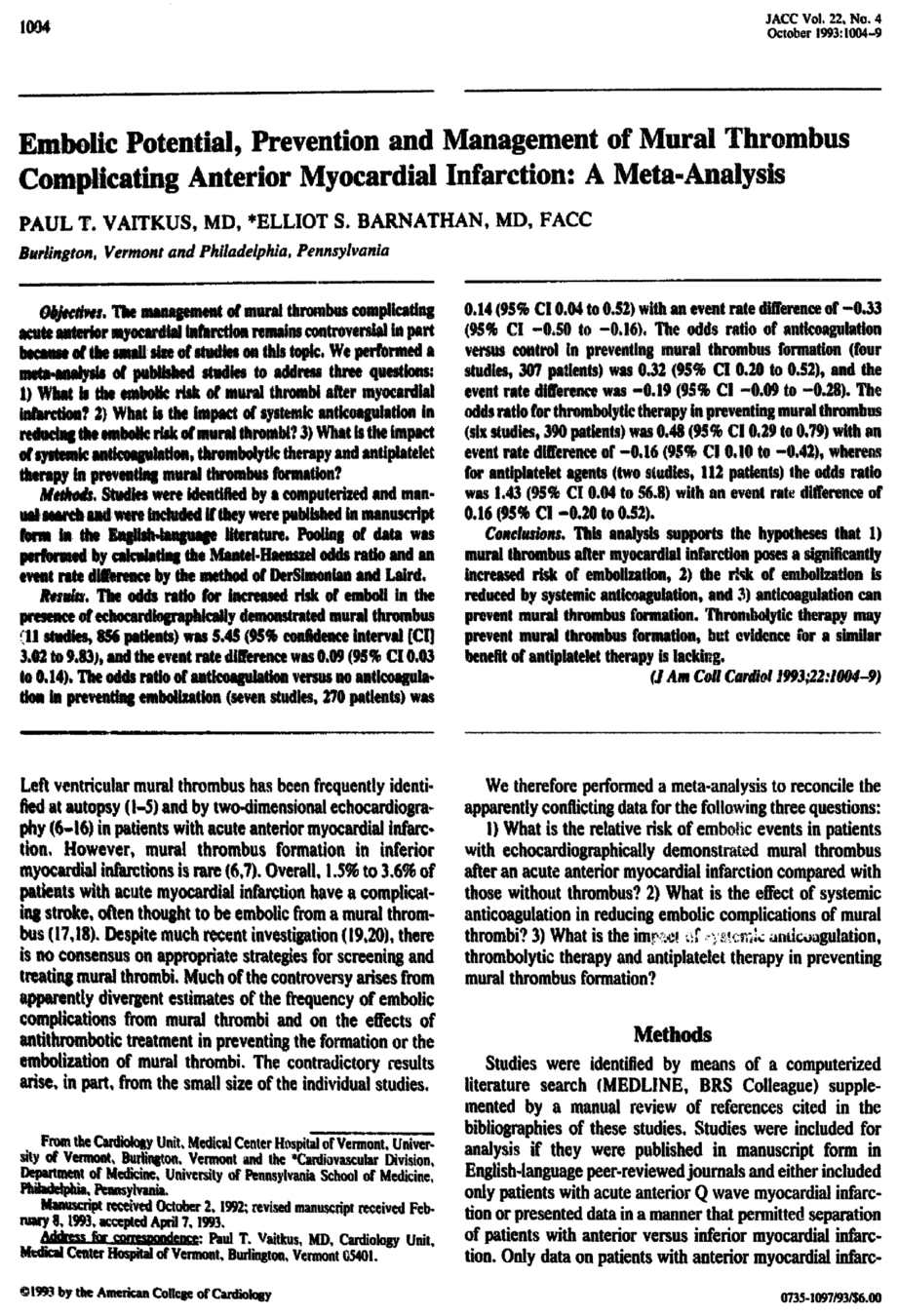
Meta-analysis from 1993 that looked at embolization and benefit of anticoagulation
LMWH?
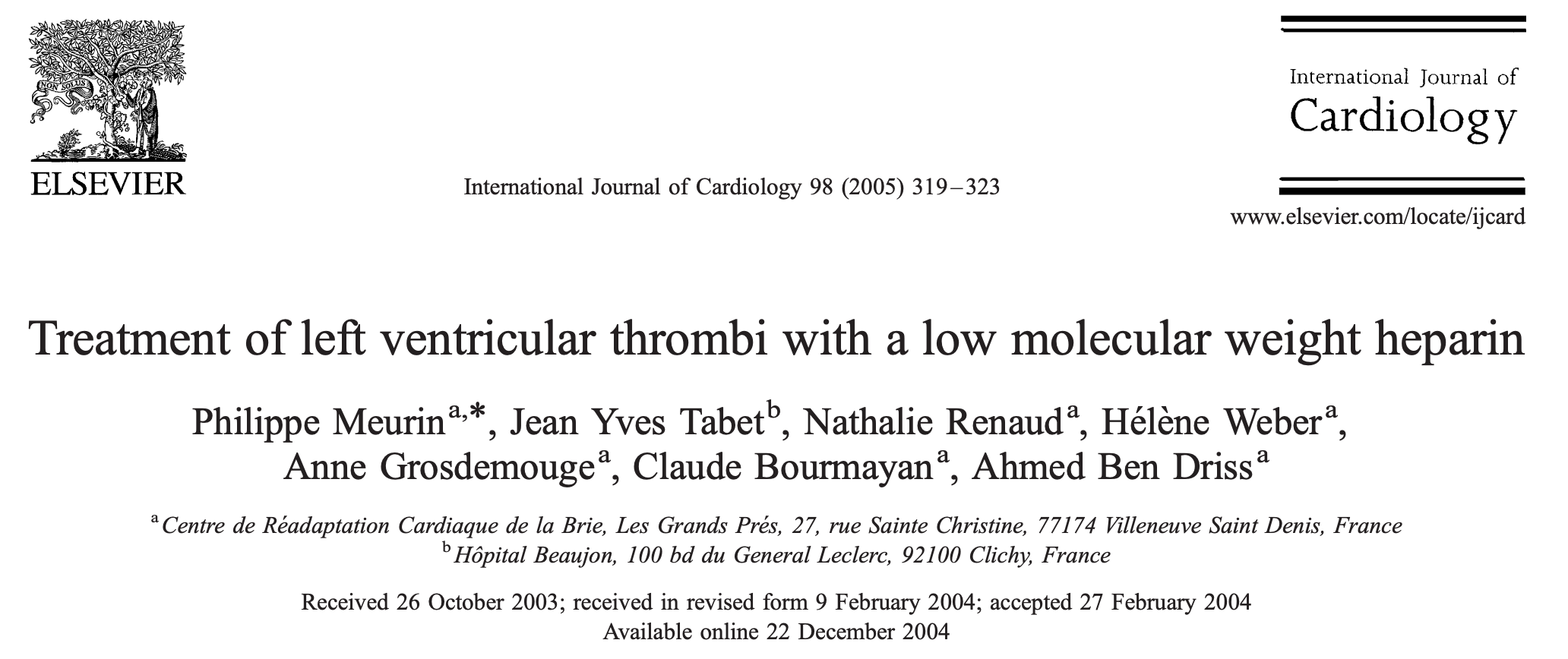
- Prospective, non-randomized, open-label trial.
- 26 left ventricular thrombi were diagnosed over the 3-year study period
- Nineteen thrombi out of twenty-six (73%) disappeared during the treatment period. No thrombocytopenia or hemorrhagic events were observed. One transient ischemic attack was reported
DOACs
Panacea
???
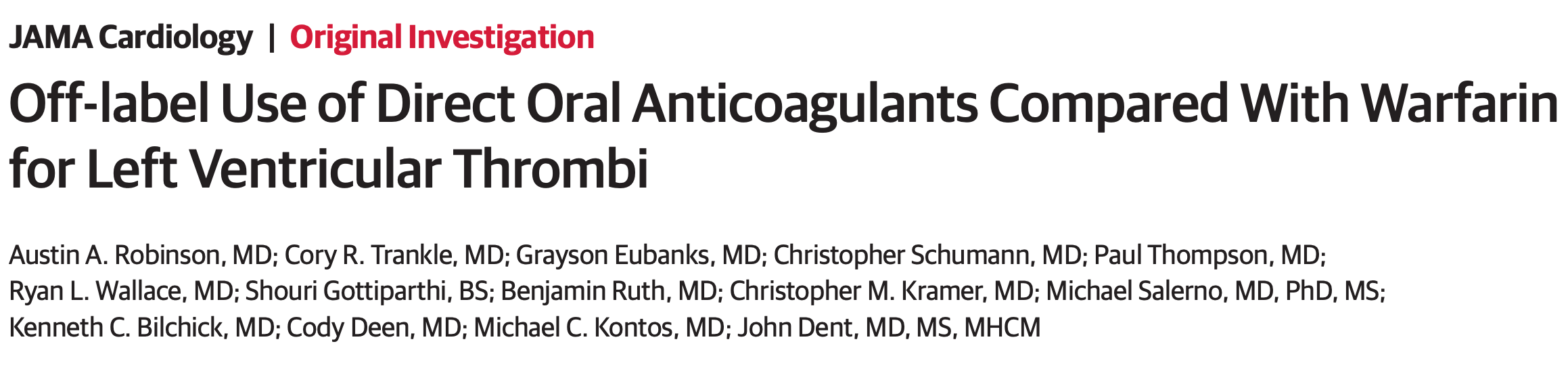
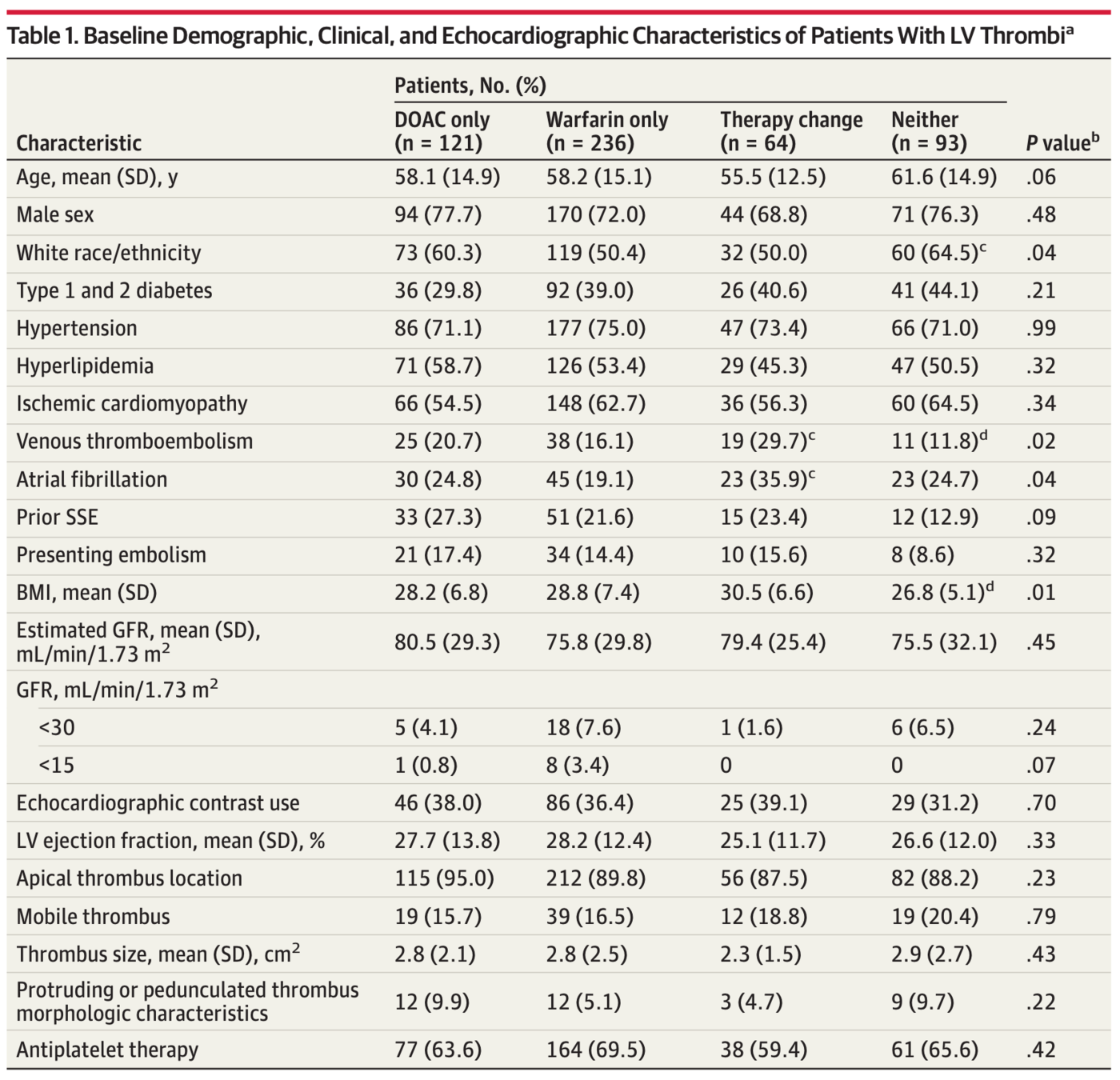
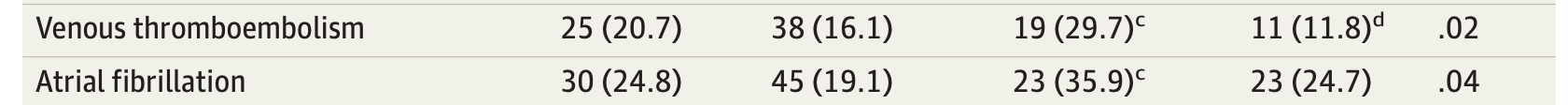
Study Design
- Cohort, retrospective, observational study
- 3 tertiary academic centres
- LV Thrombus diagnosed by Echo
- Exposure: Warfarin vs DOAC
- Outcome: Clinically apparent SSE (stroke or systemic embolism)
- SSE confirmed my medical record review and phone call
Results
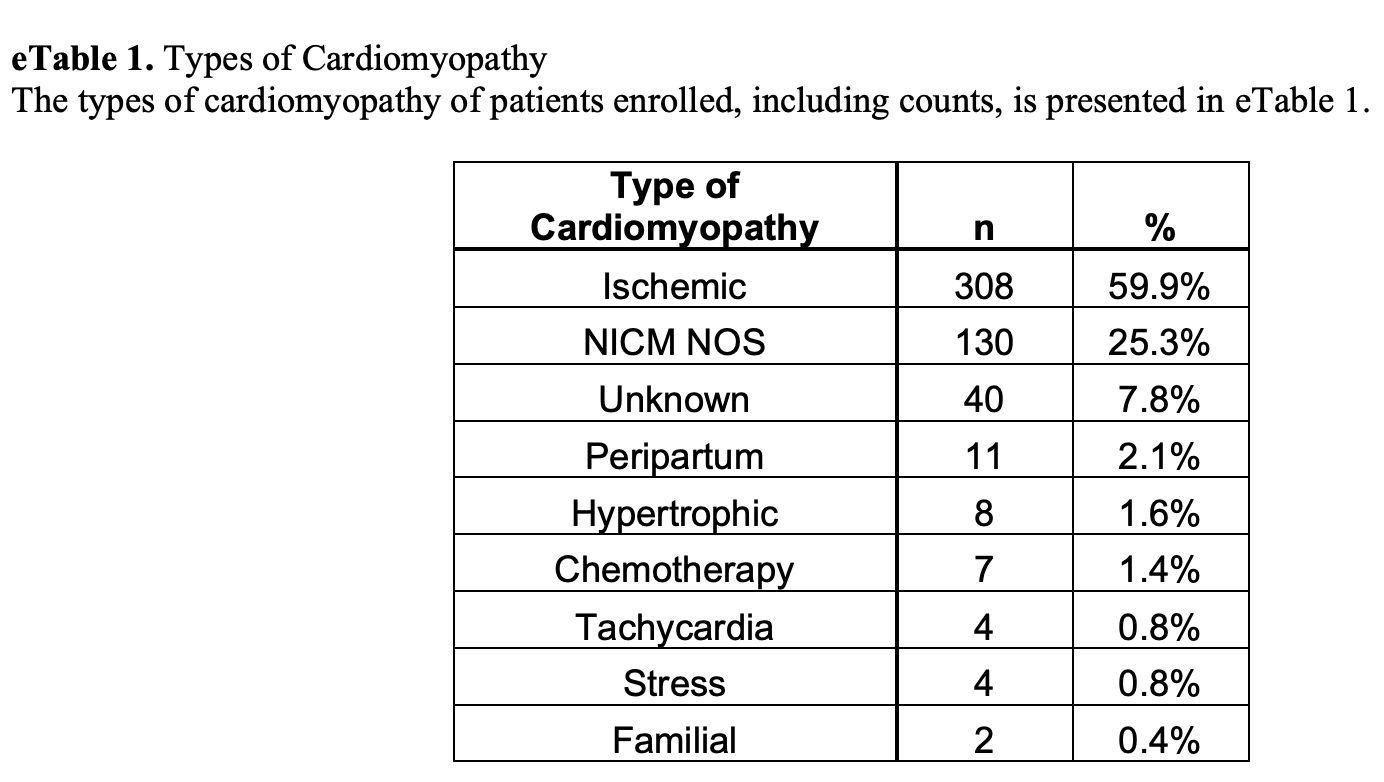
A total of 514 patients (379 men; mean [SD] age, 58.4 [14.8] years) who had echo diagnosed LV thrombi were identified
Results
Results
Results
Results
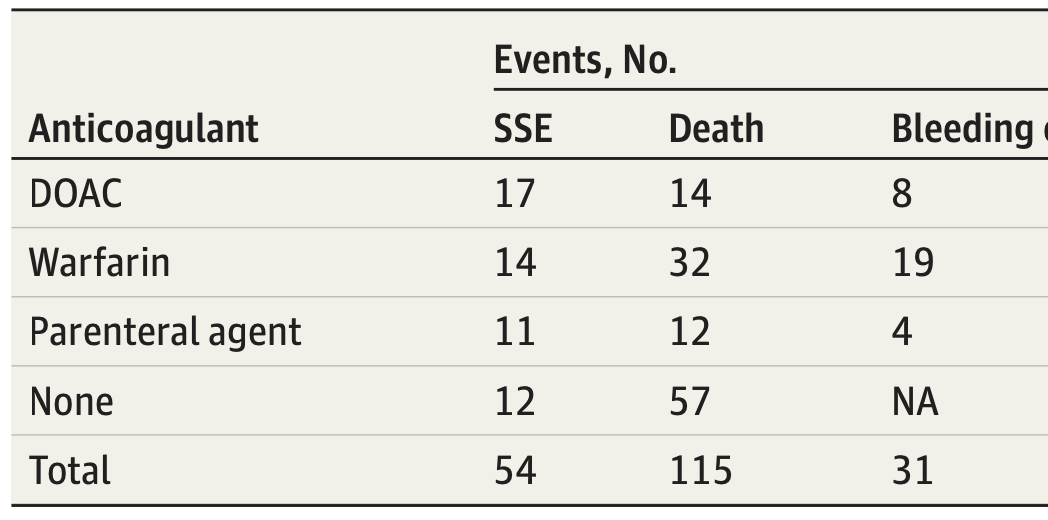
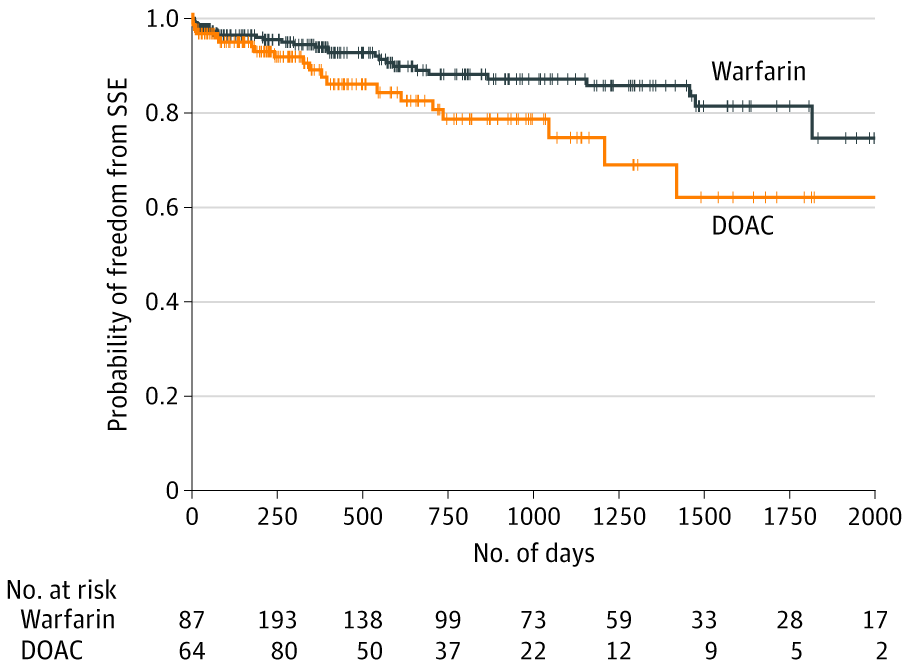
Mantel-Byar P < .001.
Results
Landmark Analyses
- Excluding first 10 days: DOAC higher SSE
- Events in first 3 months: no difference
- Only 3 months of anticoagulation: DOAC higher SSE
- Removing events after 1 year: DOAC higher SSE
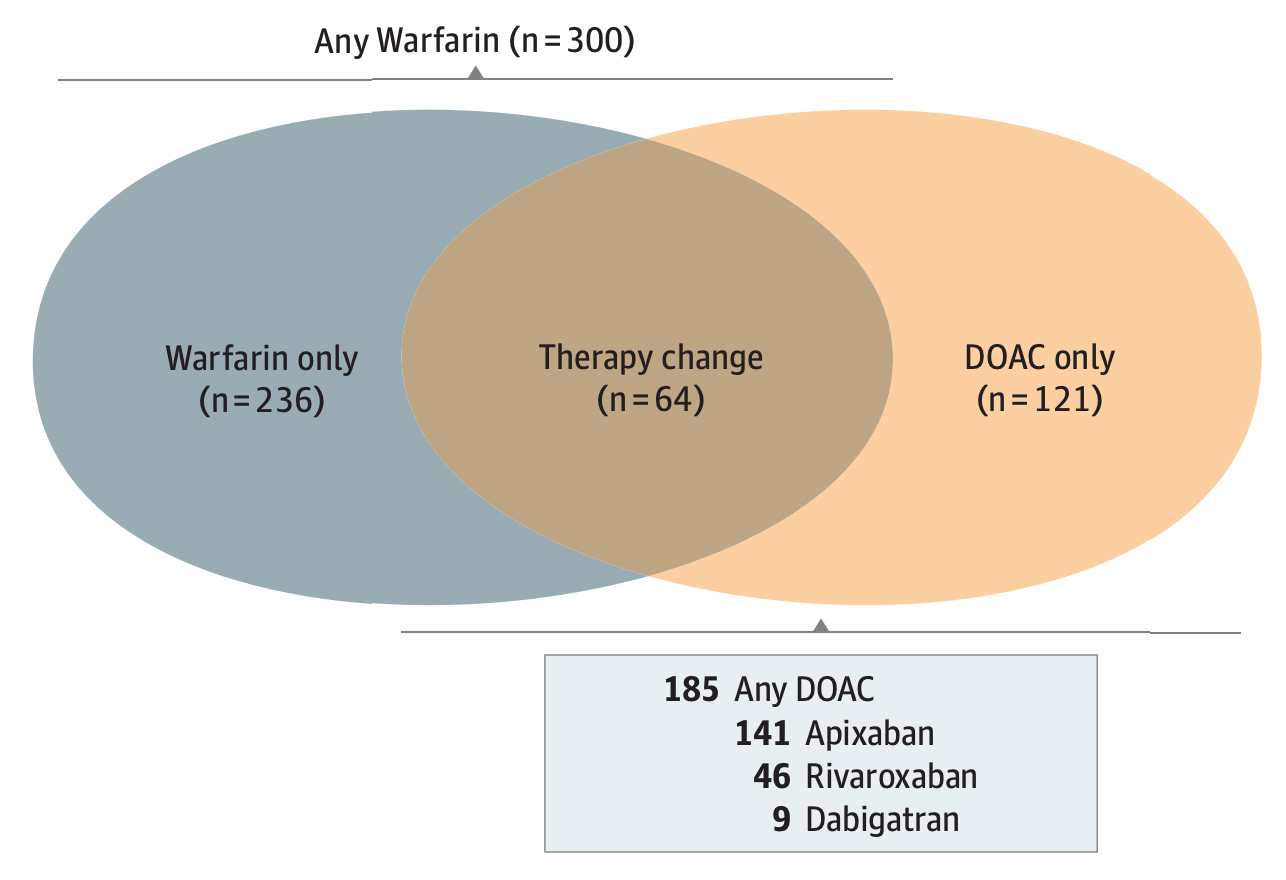
Treatment Switching
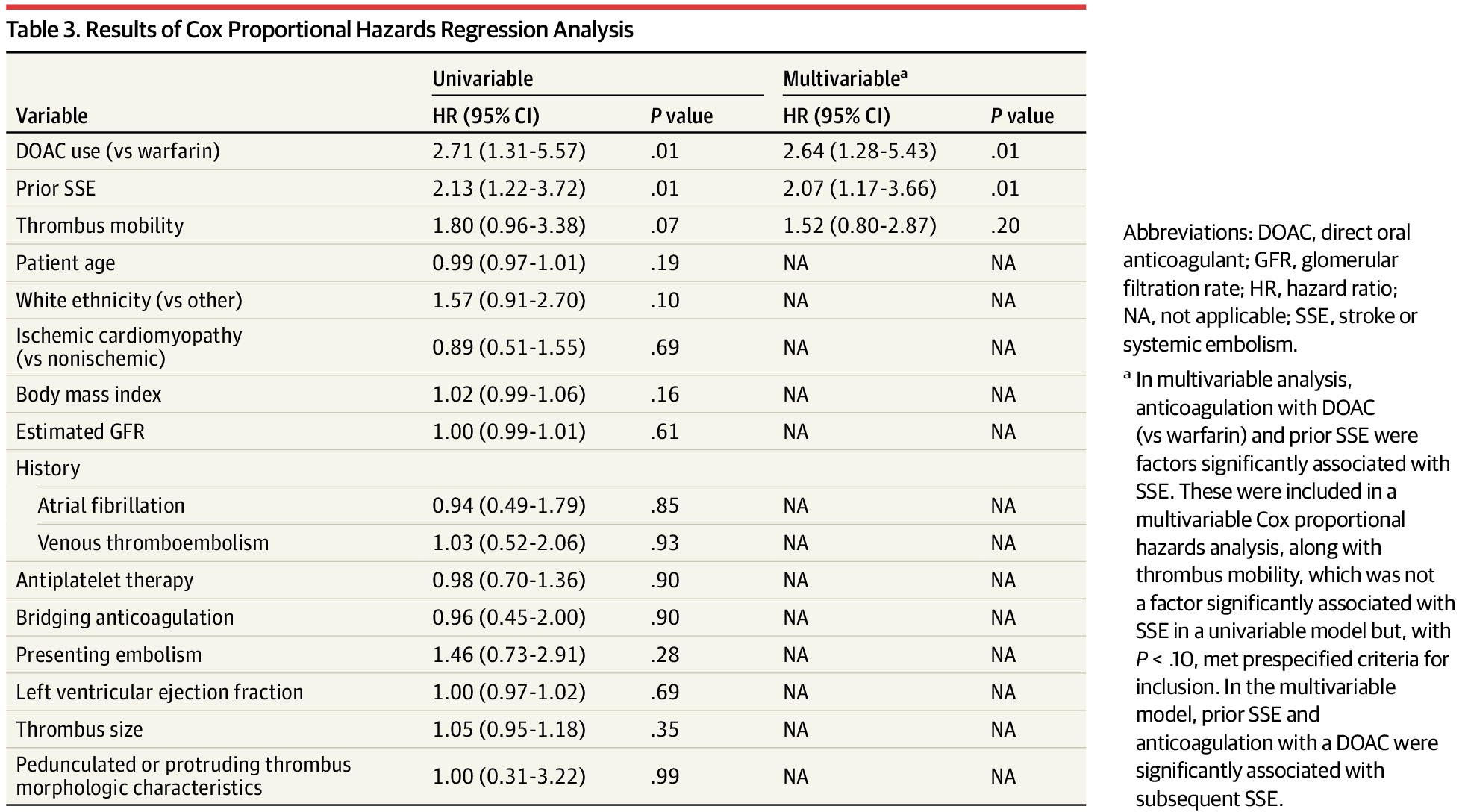
- On univariable Cox proportional hazards regression, the first oral anticoagulant was not associated with subsequent SSE (HR for DOAC vs warfarin, 1.42; 95% CI, 0.68-2.96; P = .35).
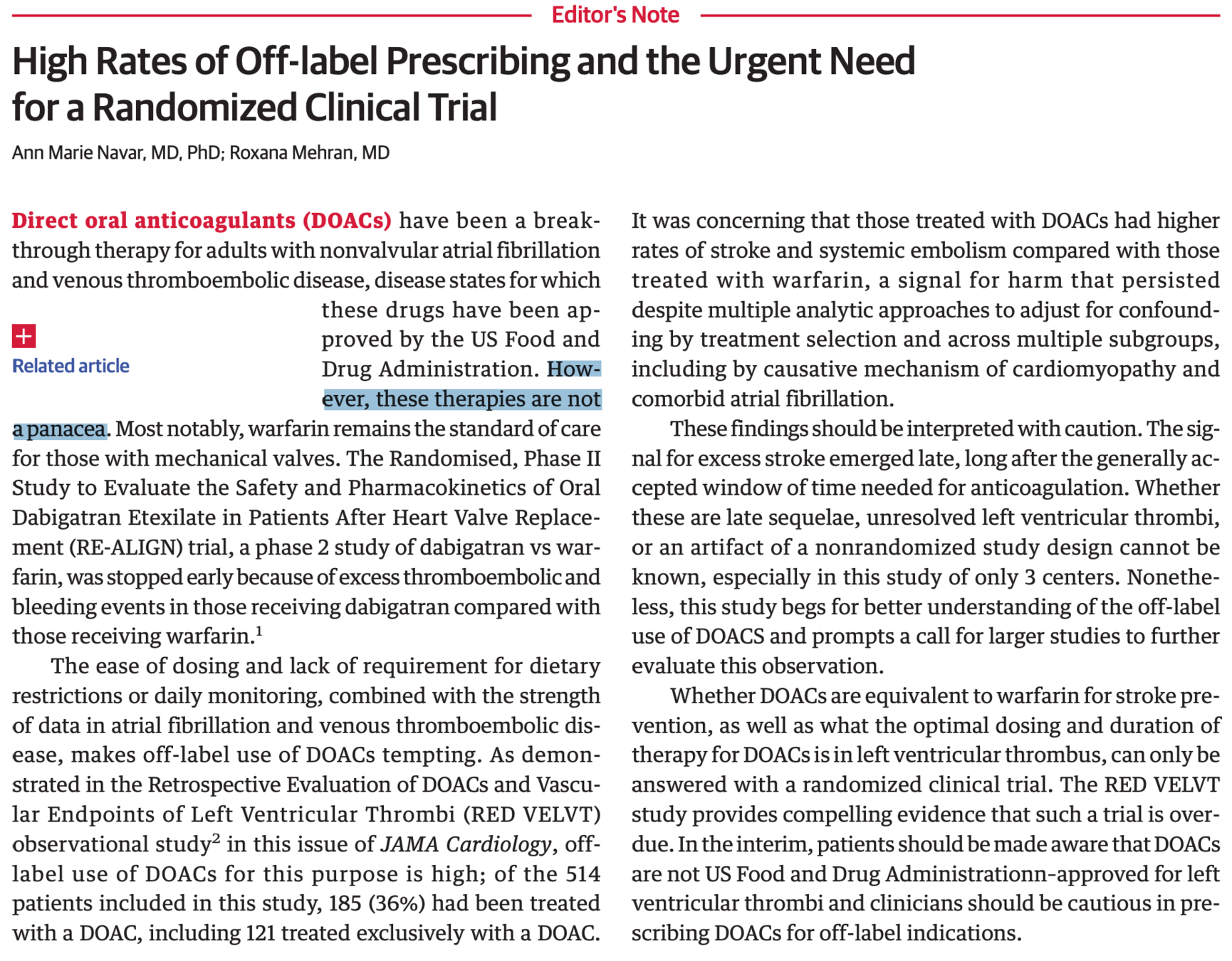
Conclusions
- DOAC associated with increase risk of SSE compared for warfain, even after adjustment for other factors
- Reason?:
- DOAC developed to prevent + treat clot whereas LV thrombus is just treating clot
- Individual DOAC may have varying effectiveness
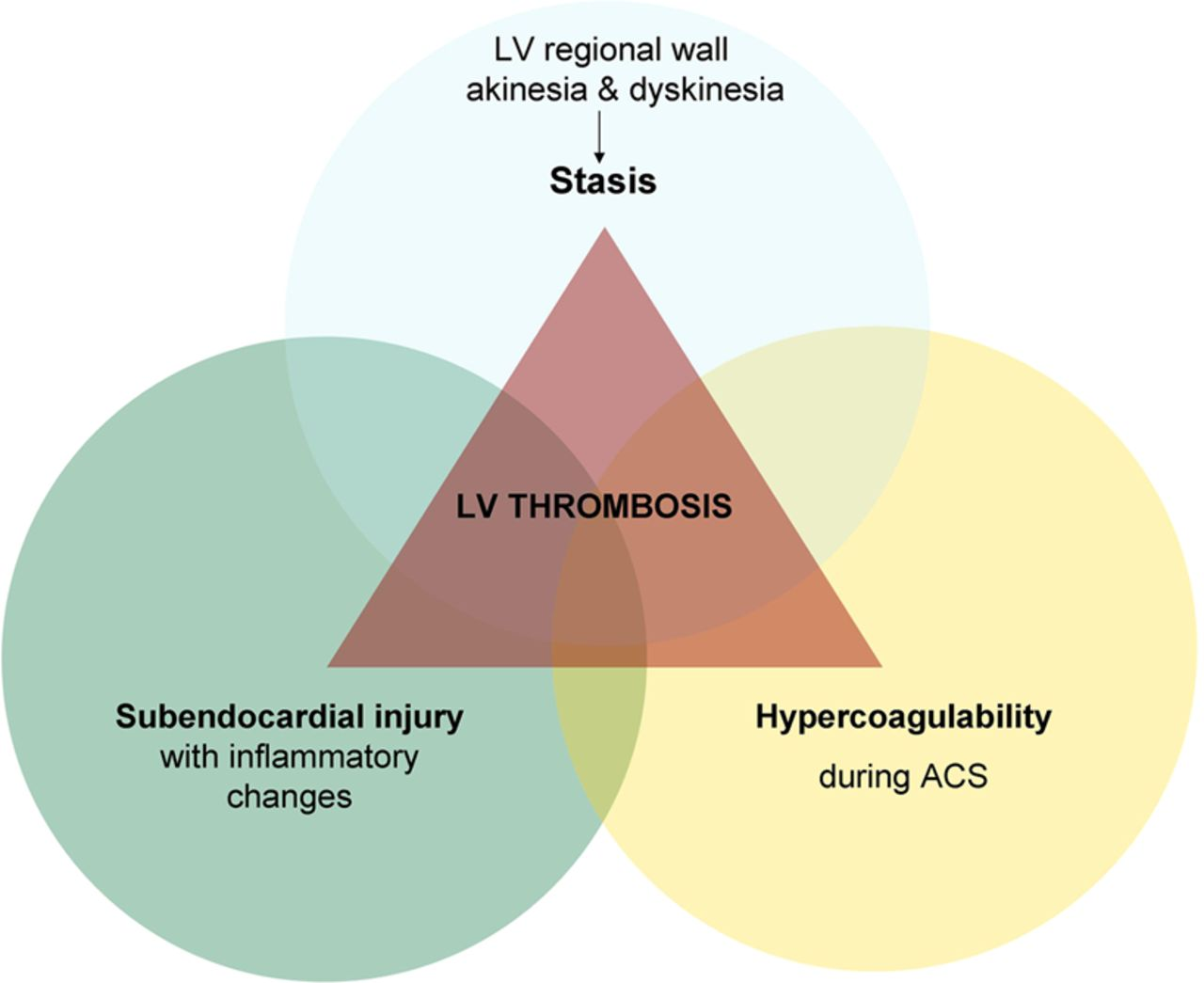
- LAA thrombus are based on stasis while LV thrombus is stasis + endocardial changes
Conclusions
- Largest study to date and multi-centre
- Review of medical records + telephone calls
- Explains low rate of events in other studies
- Other studies rely on thrombus resolution as a marker but lots of issues with that end point (poor followup, poor sensitivity of echo, or clot embolized)
- Patient centred outcome is ideal
Limitations
- Late separation of even curves, largely after initial anticoagulation window
- Confounder vs other variable that is differential treated by DOAC vs Warfarin
- Retrospective, observational design can have biases
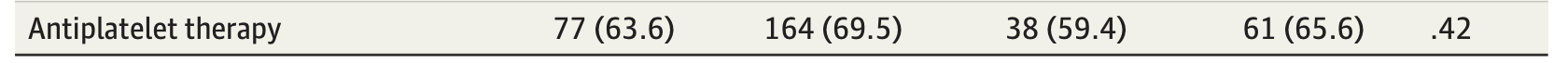
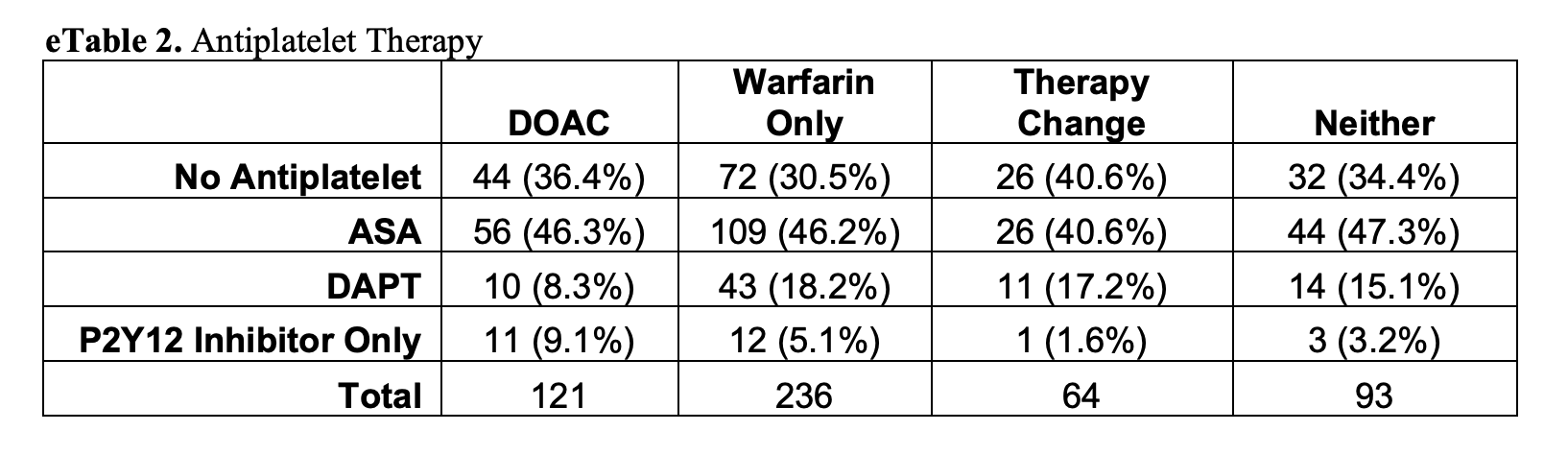
- DAPT usage
- No centralized review of echo images
- Low amount of contrast imaging
- Bleeding events not tracked and thus not compared
- No information on dosing or adherence
https://jamanetwork.com/journals/jamacardiology/fullarticle/2764430
"These therapies are not a panacea"