Diagnostic Rounds 2049
53M smoker, pneumonia resolved, persistant PLEFF
Serum
- Protein: 70 (64-83)
- LDH: 200 (<225)
Pleural Fluid (straw coloured)
- Protein: 50
- LDH: 300
- pH: 7.1
- Glucose: 3.1
Light's Criteria
- Pleural fluid protein to serum protein ratio >0.5
- Pleural fluid LDH to serum LDH ratio >0.6
- Pleural fluid level >2/3 of upper value for serum LDH
Other tests:
- Low glucose and low pH concerning for infection vs malginancy
-
Exudate (local disease) (High protein). Local factors influence the accumulation or clearance of fluid.
- Malignancy – Lung, breast, pleural.
- Infection – Pneumonia, empyema, pleuritis, viral disease
- Autoimmune – Rheumatoid, SLE
- Vascular – PE
- Cardiac – Pericarditis, CABG
- Respiratory – Haemothorax, Chylothorax
- Abdominal – Subphrenic abscess
-
Transudate (systemic illness) (Low protein <30g). Imbalance between oncotic and hydrostatic pressures
- Cardiac – Heart Failure
- Liver – Ascites, Cirrhosis
- Renal – Glomerulonephritis, Nephrotic syndrome
- Ovarian – Meigs syndrome
- Autoimmune – Sarcoid
- Thyroid – Myxoedema
When do they need a chest tube?
When to chest tube?
-
drainage frank pus/cloudy
-
positive gram stain or culture
-
pH <7.2 (if unavailable use glucose <3.4 mmol/L)
-
loculations on imaging

Diagnosis and most common cause?
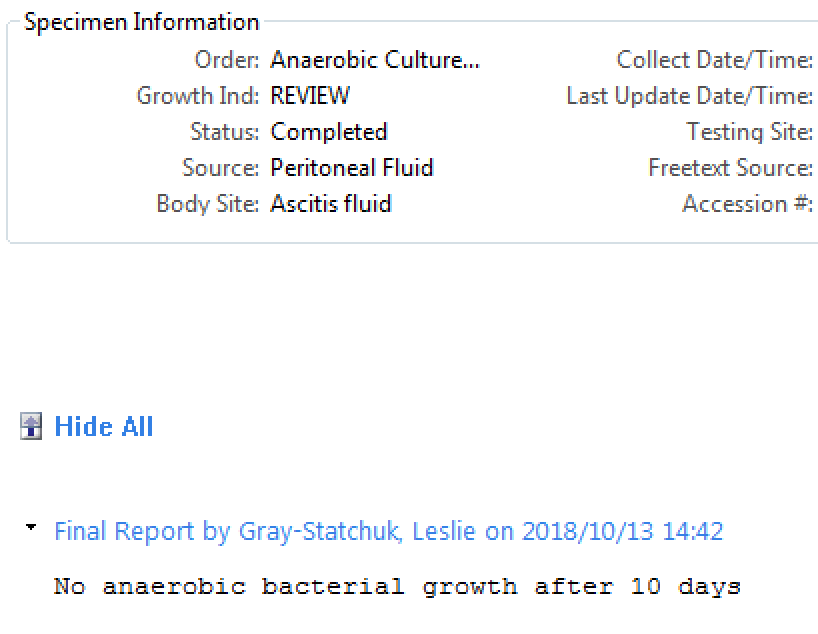
61F with PBC, new ascites + abdominal pain. SBP? Tx?
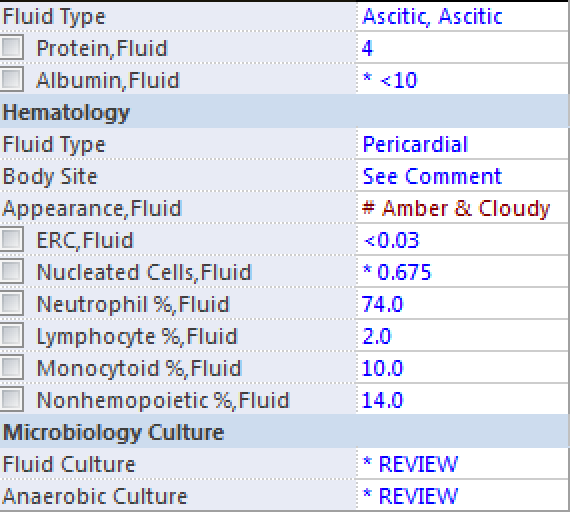
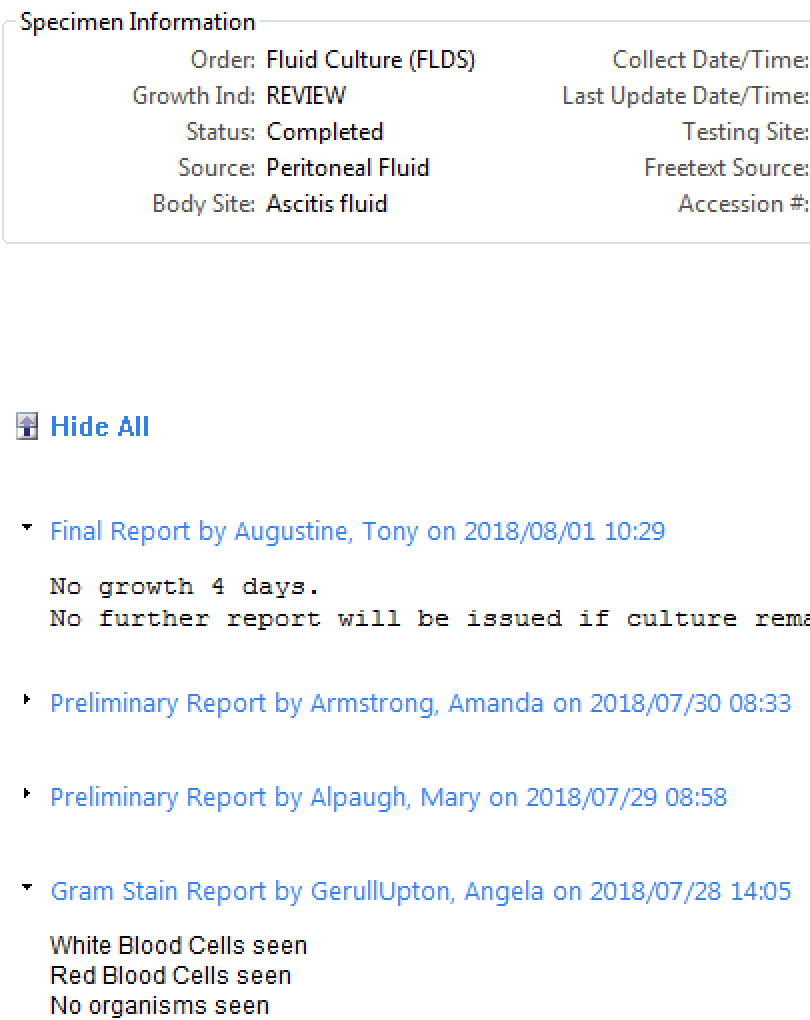
SBP
- Patients with ascitic fluid PMN counts >=250 cells/ml should receive empiric antibiotic therapy, e.g., IV third-generation cephalosporin(Class I, Level A)
- Patients with ascitic fluid PMN <250 cells/mm3 but signs/symptoms of infection (febrile or abdo pain) should receive empiric antibiotics while waiting for cultures. (Class I, Level B)
- If nosocomial SBP or atypical clinical response to treatment, follow-up paracentesis after 48 hrs of treatment to assess the response in PMN
count and culture. (Class IIa, Level C)
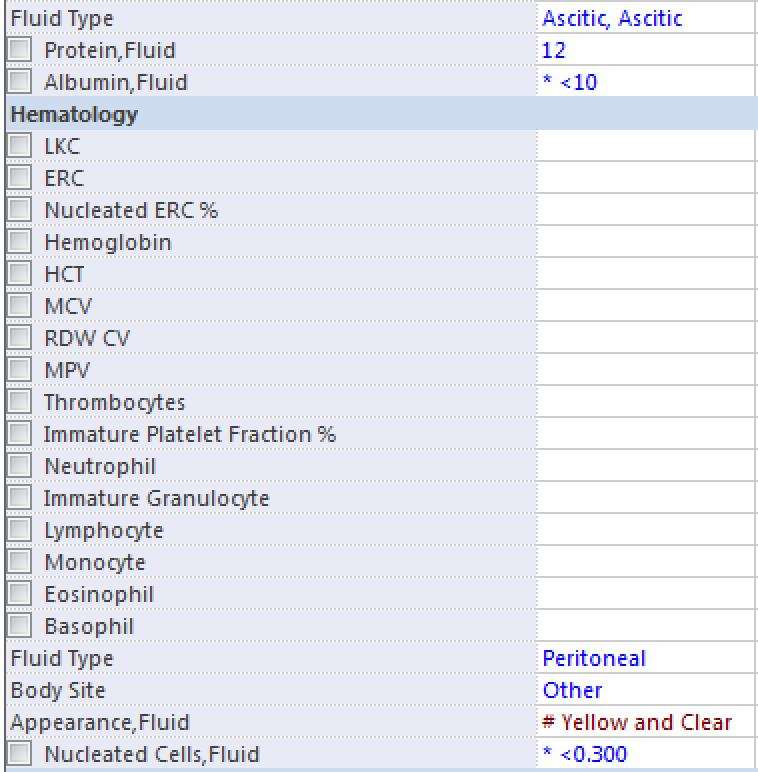
Text
Bonus points: His albumin is 23, portal hypertension present?
3 Indications for SBP Prophylaxis?
SBP Prophylaxis
- History of SBP
- GI Bleed + Cirrhosis
- Fluid Albumin <15 + CKD/Bad Cirrhosis
Norfox or Cipro or Septra
https://www.aasld.org/sites/default/files/guideline_documents/adultascitesenhanced.pdf
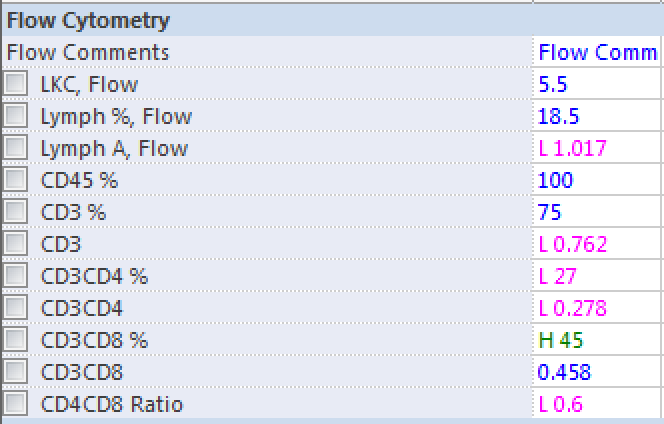
42F history of HIV, leaving AMA. CD4? What is she at risk for? What prophylaxis?
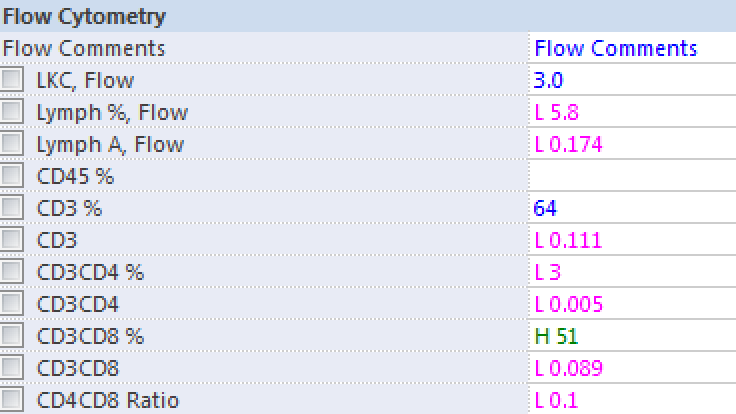
Primary Prophylaxis
- CD4< 200: PJP (Septra 1DS Daily)
- CD4<150: Histoplasma occupational exposure or endemic area for (Itraconzole 200mg Daily)
- CD4<100: If Toxoplasma IgG+ (Septra 1DS Daily)
- CD4<50: MAC (Azithromycin 1200mg PO Weekly)
https://aidsinfo.nih.gov/guidelines/html/4/adult-and-adolescent-opportunistic-infection/354/primary-prophylaxis
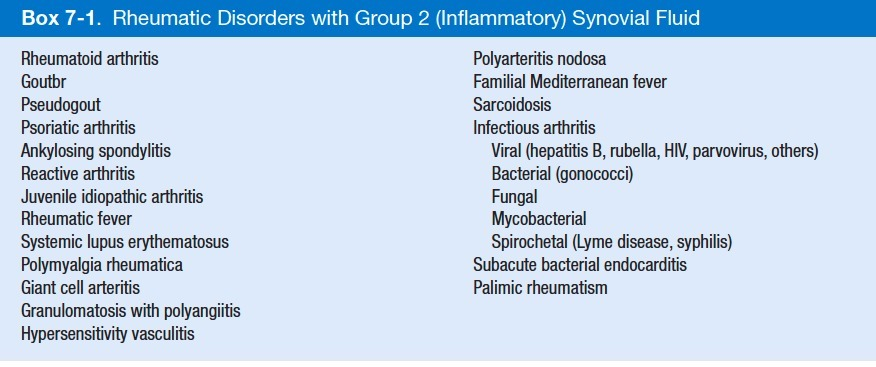
45M with hx of gout and multiple previous ACL repair, knee red/warm/swollen.
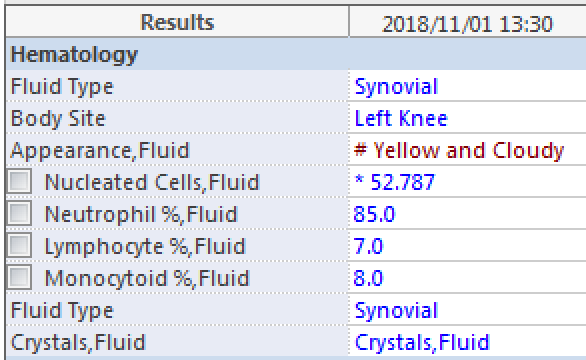
Normal? Inflamm? Septic? Dx/Tx (watch? steroid? ABx? NSAIDS?)
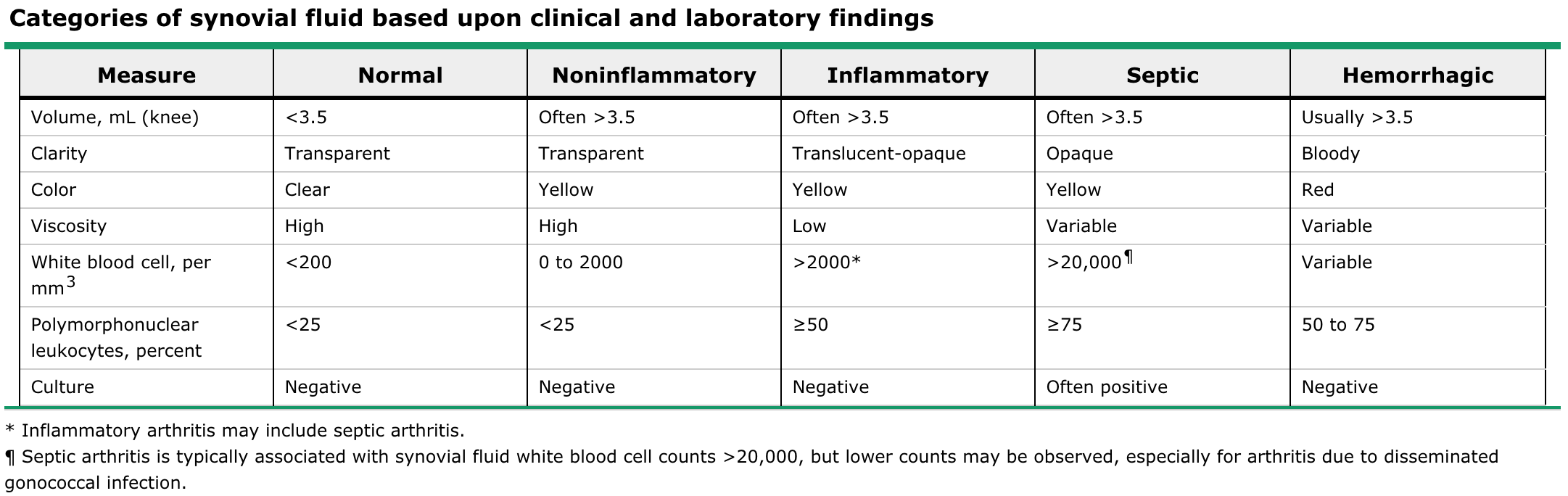
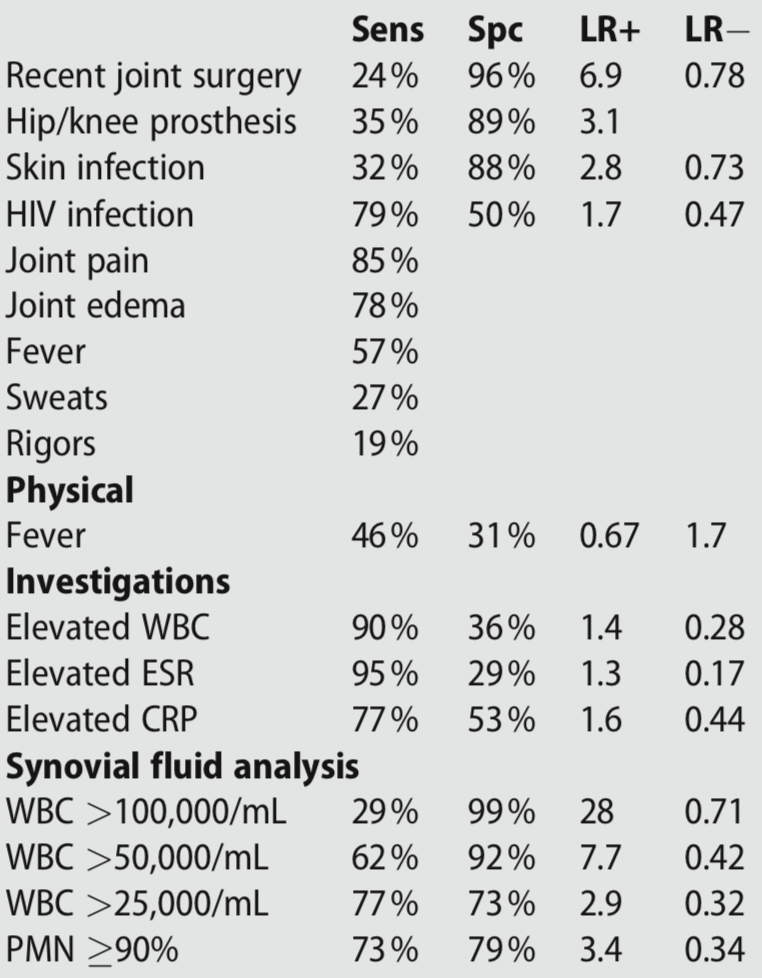
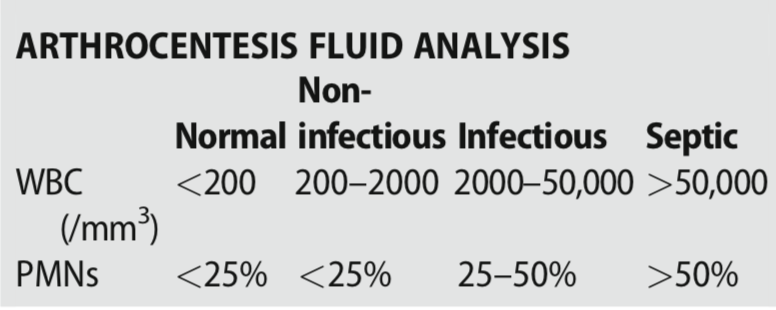
Synovial fluid is usually purulent, with typical leukocyte count of 50,000 to 150,000 cells/mm3 (most of which are neutrophils)
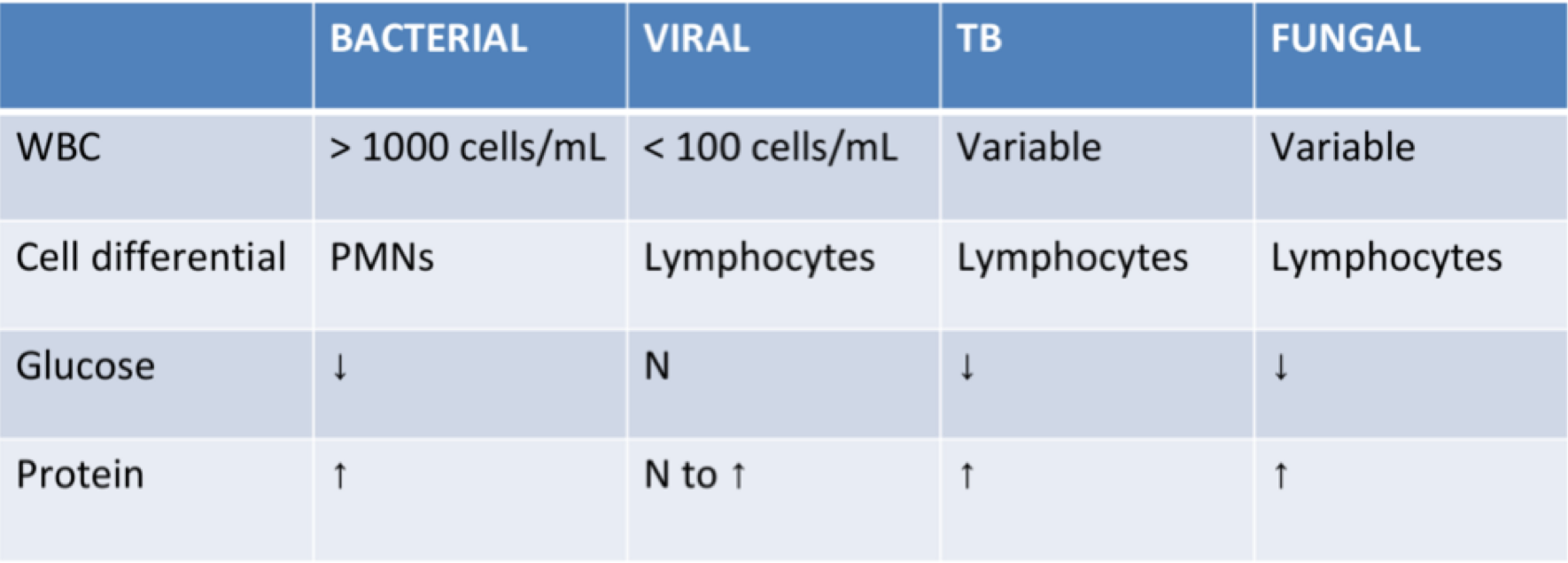
67M homeless, 2-3 week malaise/odd, now decreased LOC, fever, neck rigid, Dx and Tx?
| Tube # | 2 |
|---|---|
| Appearance | clear & colourless |
| Glucose | 1.7 (2.2-3.9) |
| Protein | 500 (200-400) |
| Tube # | 1 |
| Appearance | slight pink & clear |
| Nucleated Cells | 400 (0-5) |
| Erythrocyte | 6 |
| Tube | 4 |
| Appearance | clear & colourless |
| Nucleated Cells | 400 (0-5) |
| Erythrocytes | 1 |
| Neutrophil % | 35 |
| Lymptocyte % | 65 |
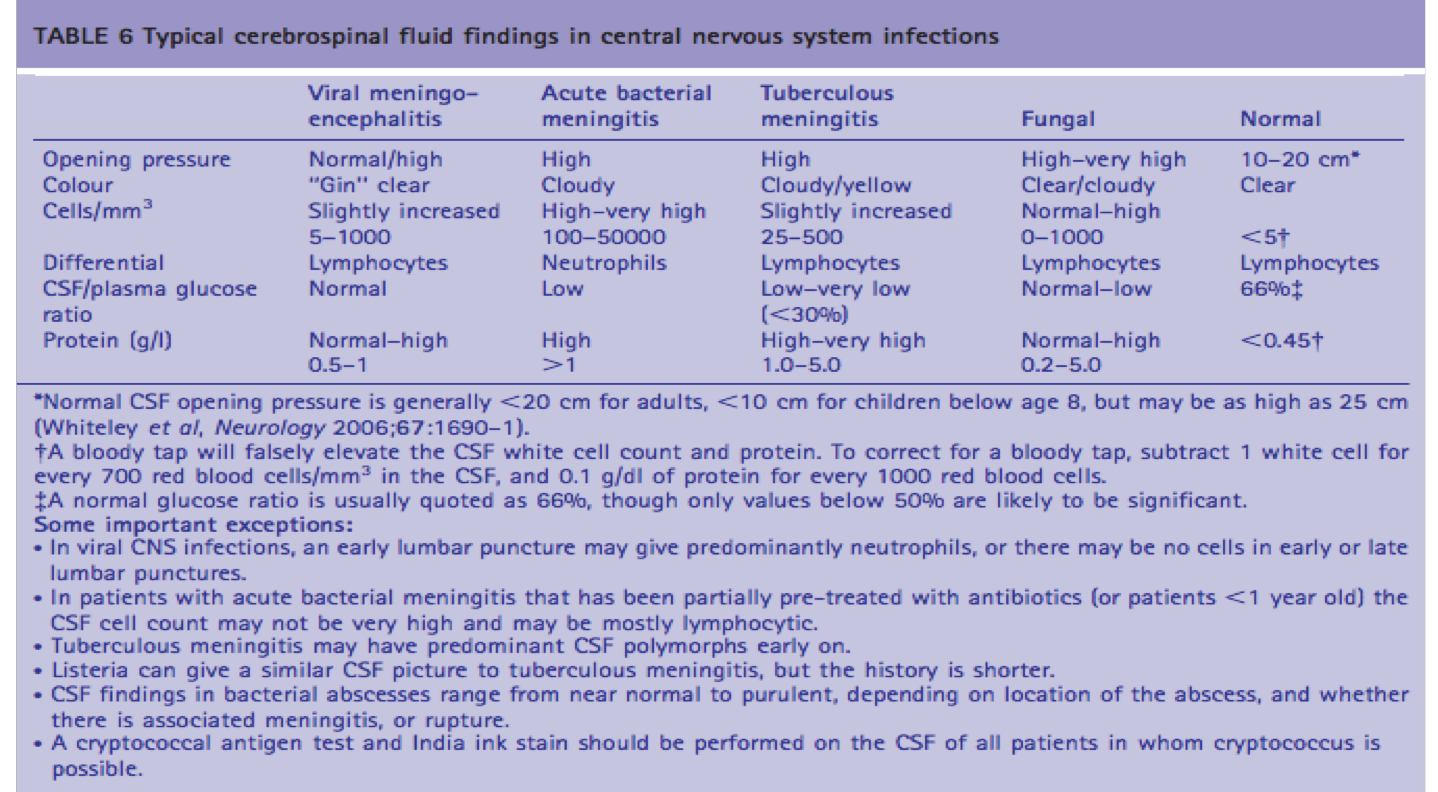
TB Meningitis
-
Patients with tuberculous meningitis are categorized by stage on presentation, based upon mental status and focal neurologic signs as follows:
•Stage I patients are lucid with no focal neurologic signs or evidence of hydrocephalus.
•Stage II patients exhibit lethargy, confusion; they may have mild focal signs, such as cranial nerve palsy or hemiparesis.
•Stage III represents advanced illness with delirium, stupor, coma, seizures, multiple cranial nerve palsies, and/or dense hemiplegia.
INH (isoniazid) + RMP (Rifampin) + PZA (Pyrazinamide) + EMB (Ethambutol)
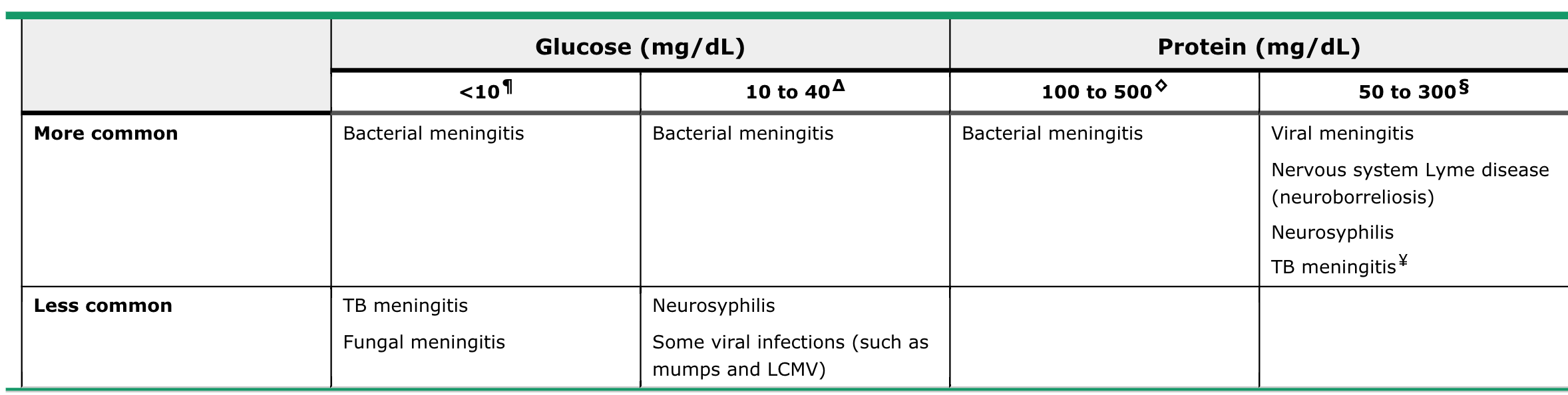
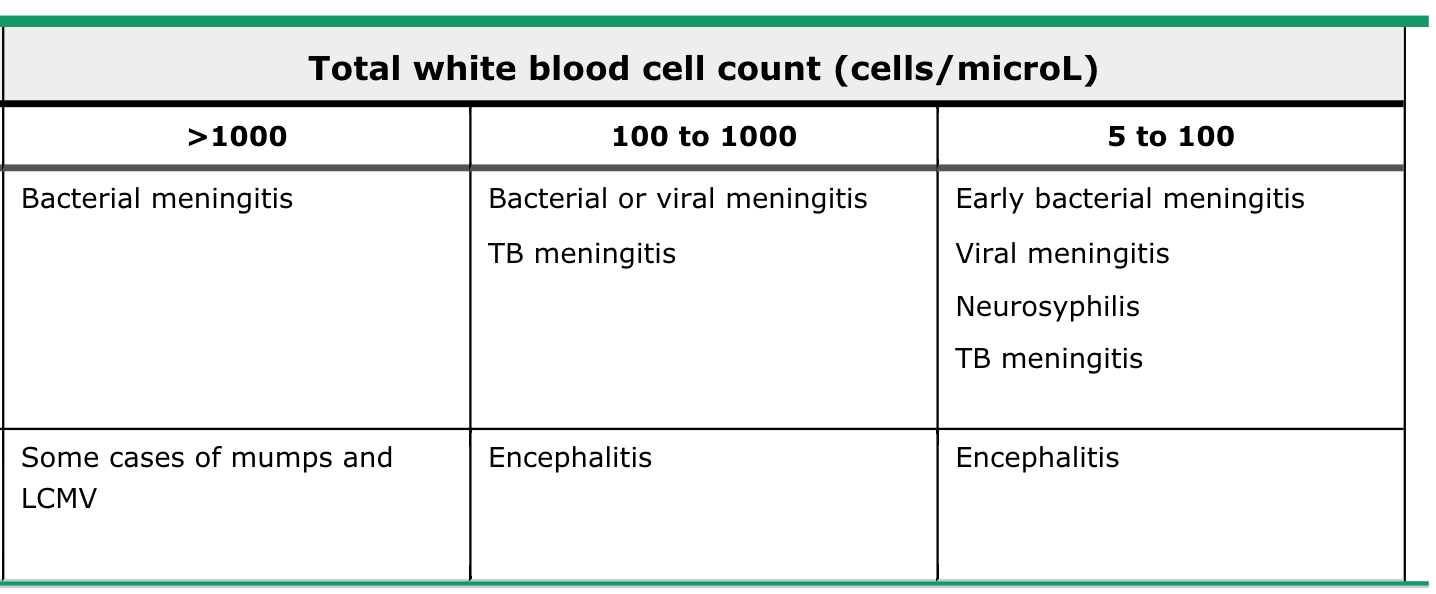
Lymphocyte
Predominant