Interpreting the evolution of
SARS-CoV-2
Jesse Bloom
Fred Hutch Cancer Research Center / HHMI
Slides at https://slides.com/jbloom/understanding-sars-cov-2-evolution
Disclosures
- I am on the scientific advisory boards of Apriori Bio and Oncorus
- I am an inventor on Fred Hutch licensed patents related to deep mutational scanning of viral proteins
- My lab has unfunded research collaborations with Vir Biotechnology
Outline
- Principles of viral antigenic evolution and emergence of Omicron
Outline
- Principles of viral antigenic evolution and emergence of Omicron
- Importance of the SARS-CoV-2 receptor-binding domain (RBD)
Outline
- Principles of viral antigenic evolution and emergence of Omicron
- Importance of the SARS-CoV-2 receptor-binding domain (RBD)
- Mapping antibody escape to interpret viral evolution
Outline
- Principles of viral antigenic evolution and emergence of Omicron
- Importance of the SARS-CoV-2 receptor-binding domain (RBD)
- Mapping antibody escape to interpret viral evolution
Only sometimes does virus evolution lead to changes in antigenic phenotype
- Measles virus: Does not evolve to escape immunity. People are infected at most once in their lives. A vaccine developed in the 1960s still works today.
- Influenza virus: Evolves to escape immunity. People are infected every ~5 years. The vaccine needs to be updated annually.

Early on, many speculated SARS-CoV-2 would not undergo antigenic evolution
We decided to look at another human coronavirus: CoV-229E causes common colds and has been circulating in humans since at least 1960s.
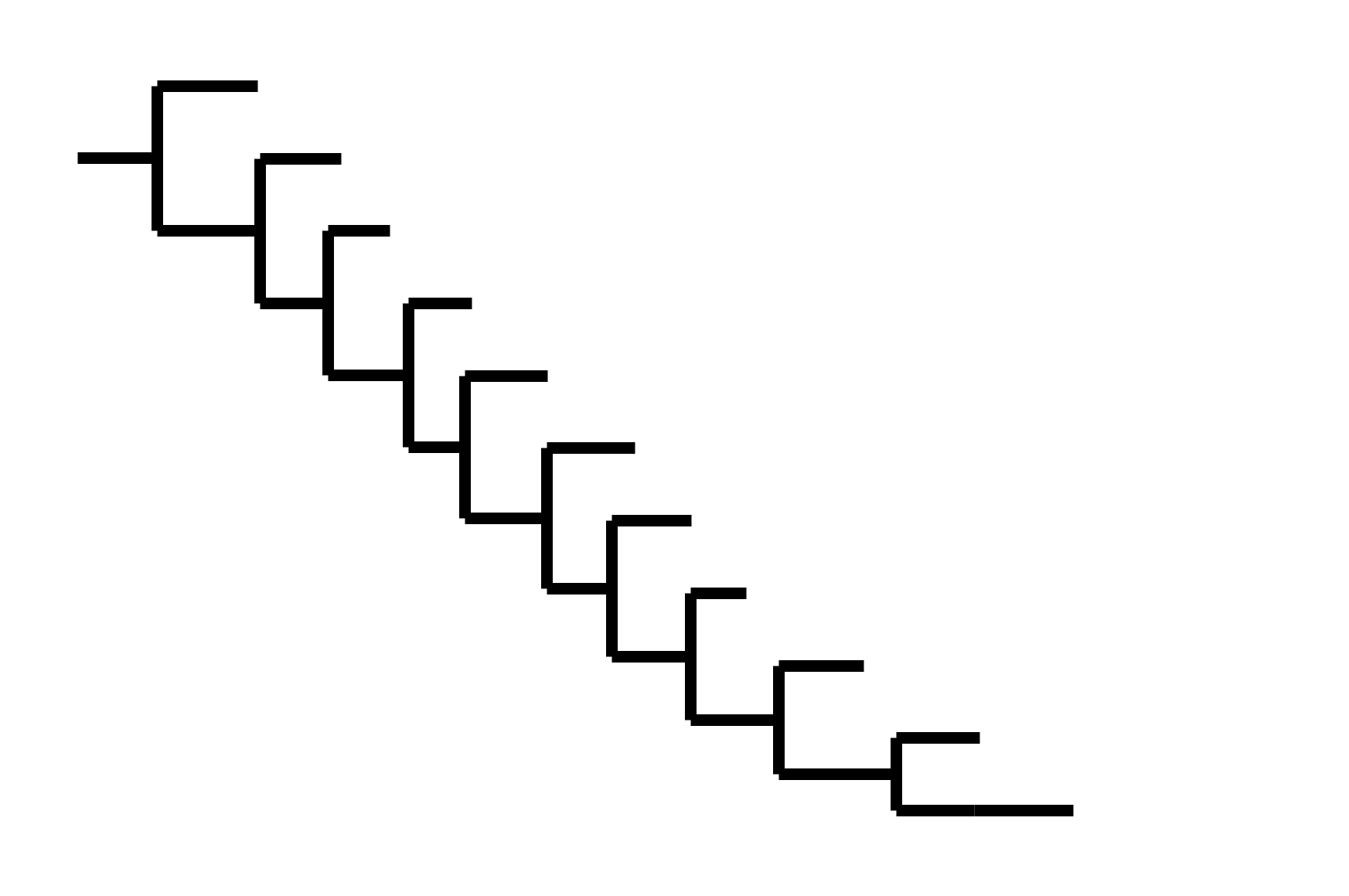
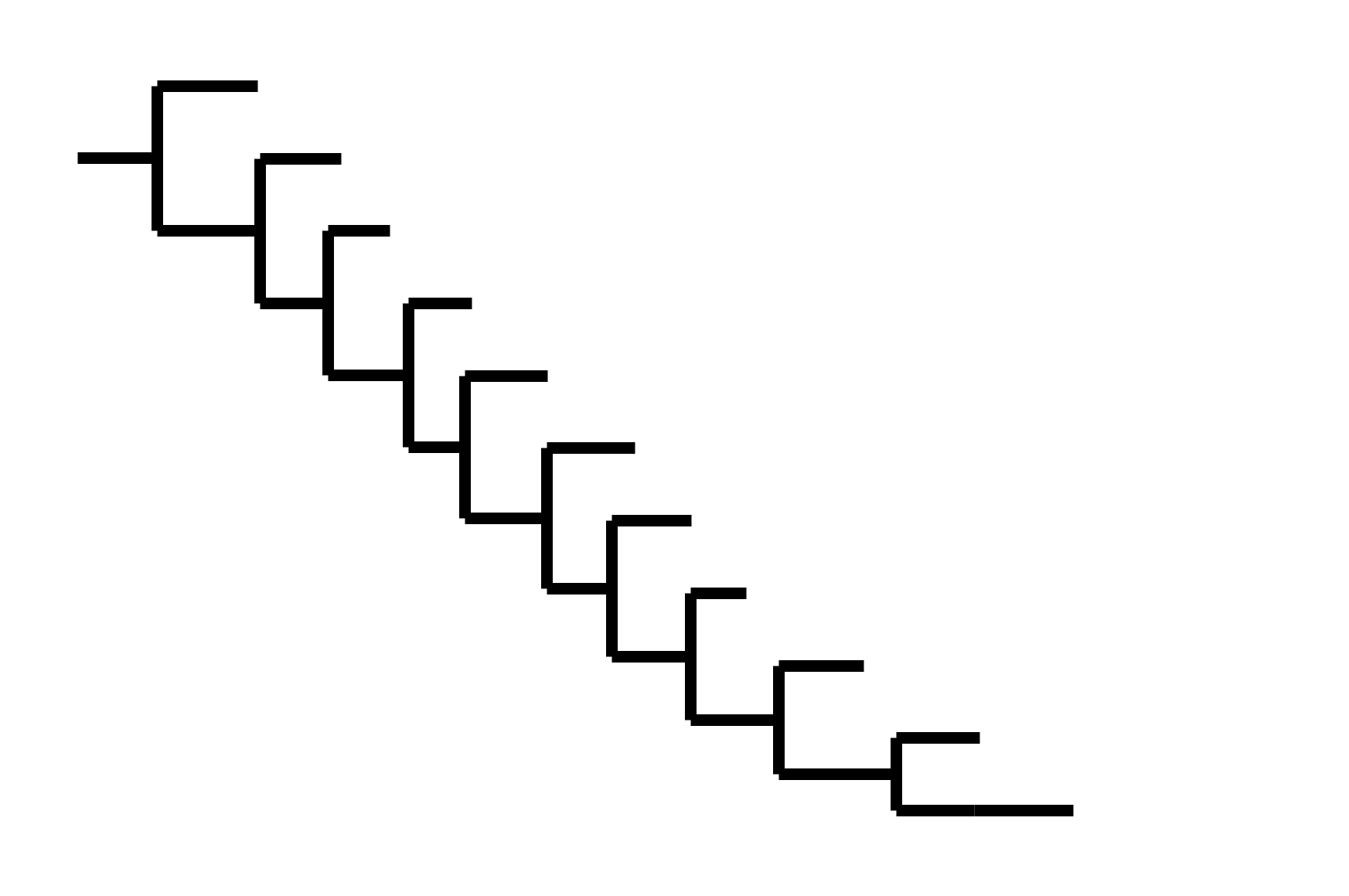
Reconstructing evolution of CoV-229E spike

We experimentally generated CoV-229E spikes at ~8 year intervals so we could study them in the lab:
- 1984
- 1992
- 2001
- 2008
- 2016
Note "ladder-like" shape of tree
Evolution of CoV-229E spike erodes neutralization by human antibody immunity
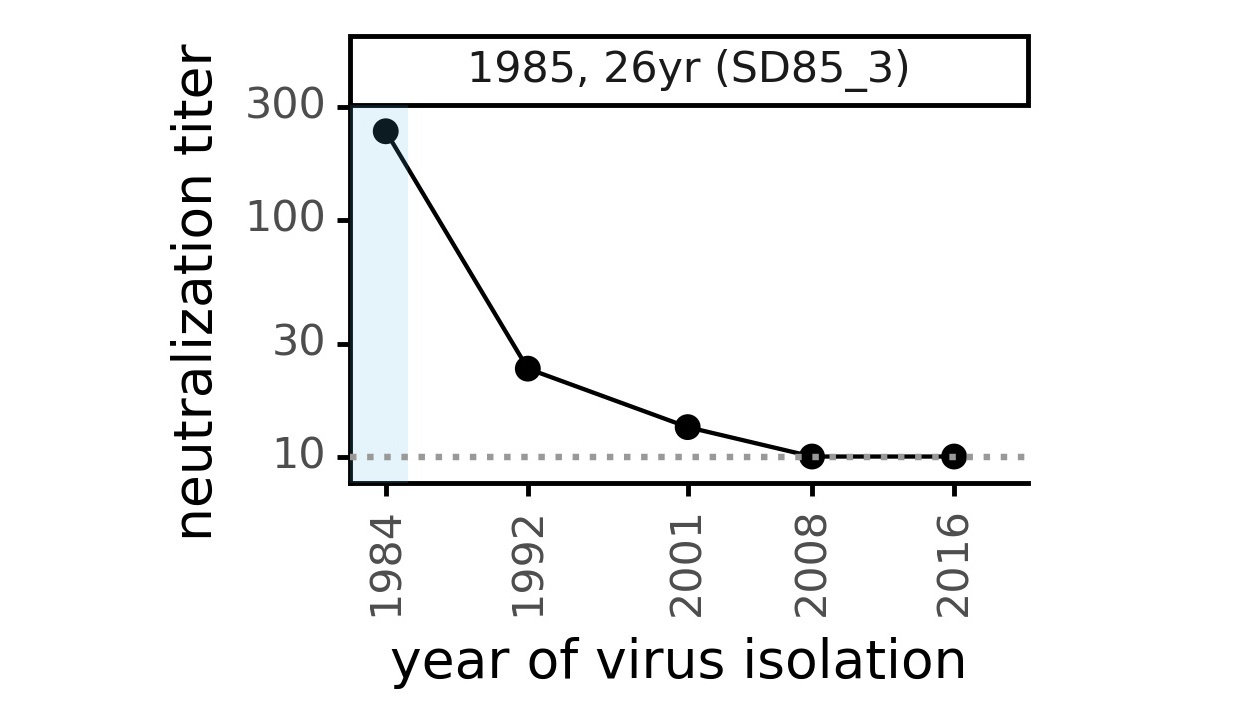
Serum collected in 1985 neutralizes virus with spike from 1984, but less effective against more recent viruses.
Viral evolution erodes antibody immunity of different people at different rates
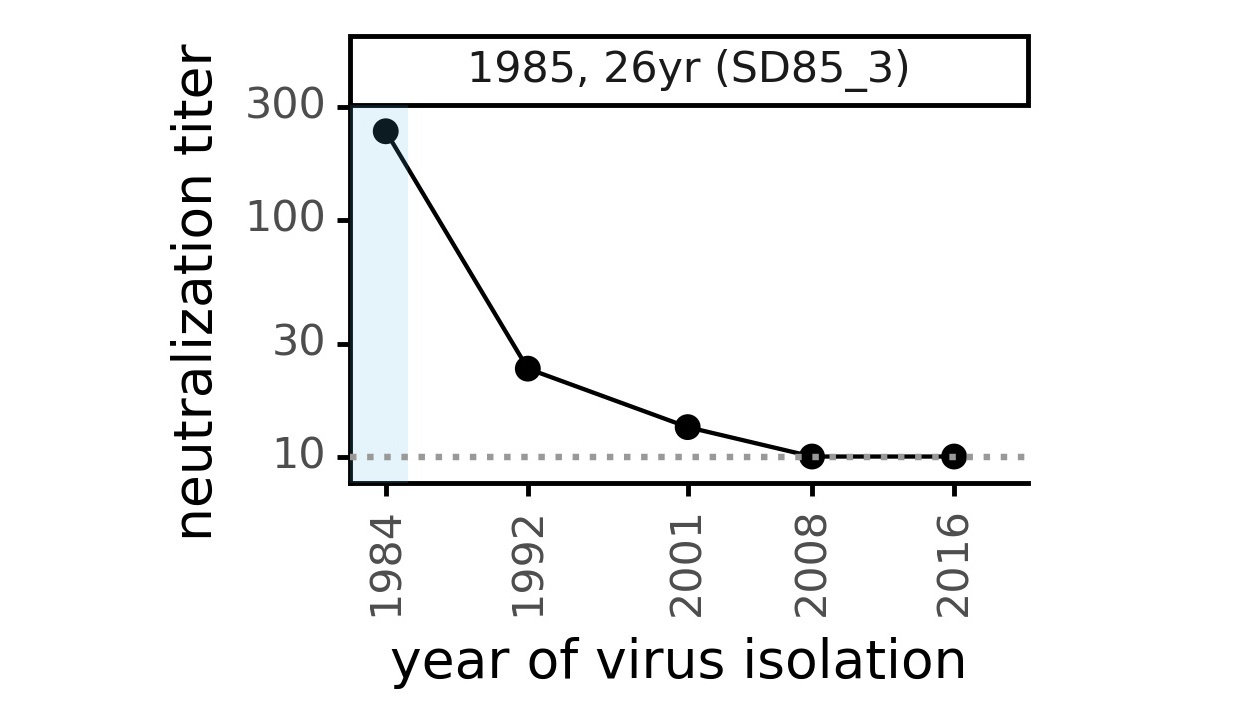
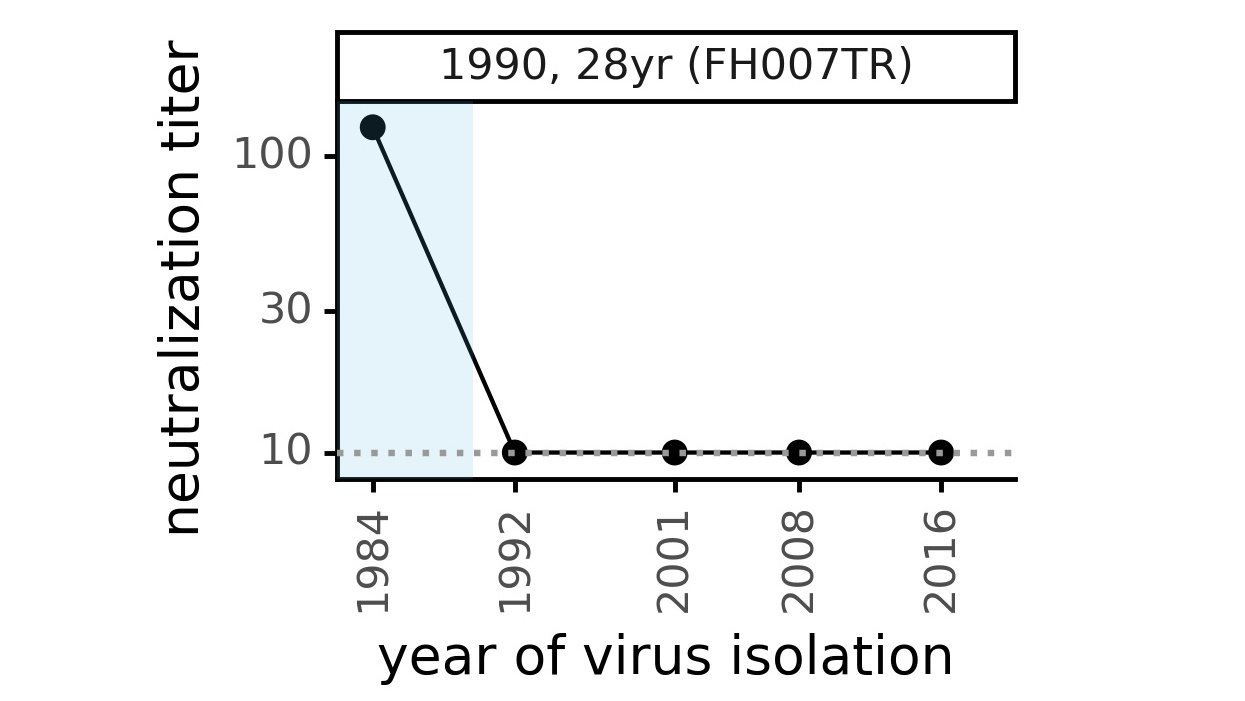
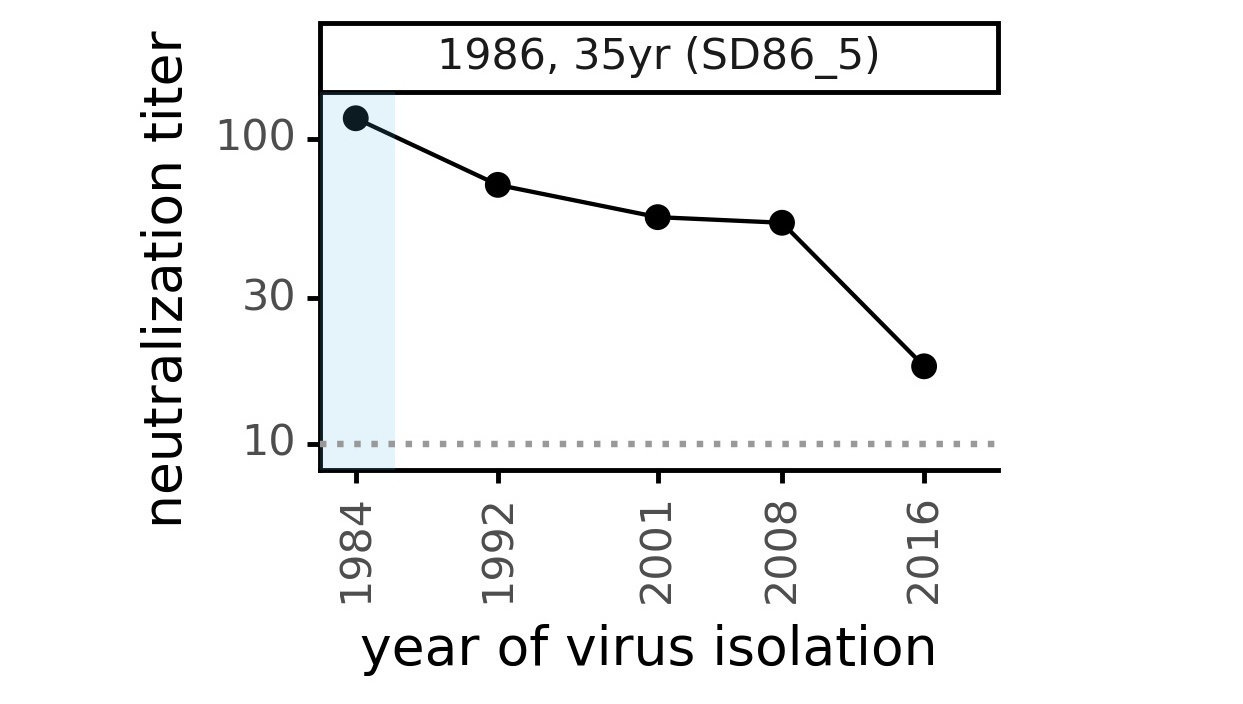
We are studying basis of these differences, as ideally vaccines would elicit more evolution-resistant sera as on the right.
Phylogenetic tree shape and vaccine strategy
CoV-229E has ladder-like tree:
- new variants displace old ones
- new variants descend from recent successful ones
Human influenza A evolves this way too. It's theoretically possible to pick single well-matched vaccine strain.
Phylogenetic tree shape and vaccine strategy
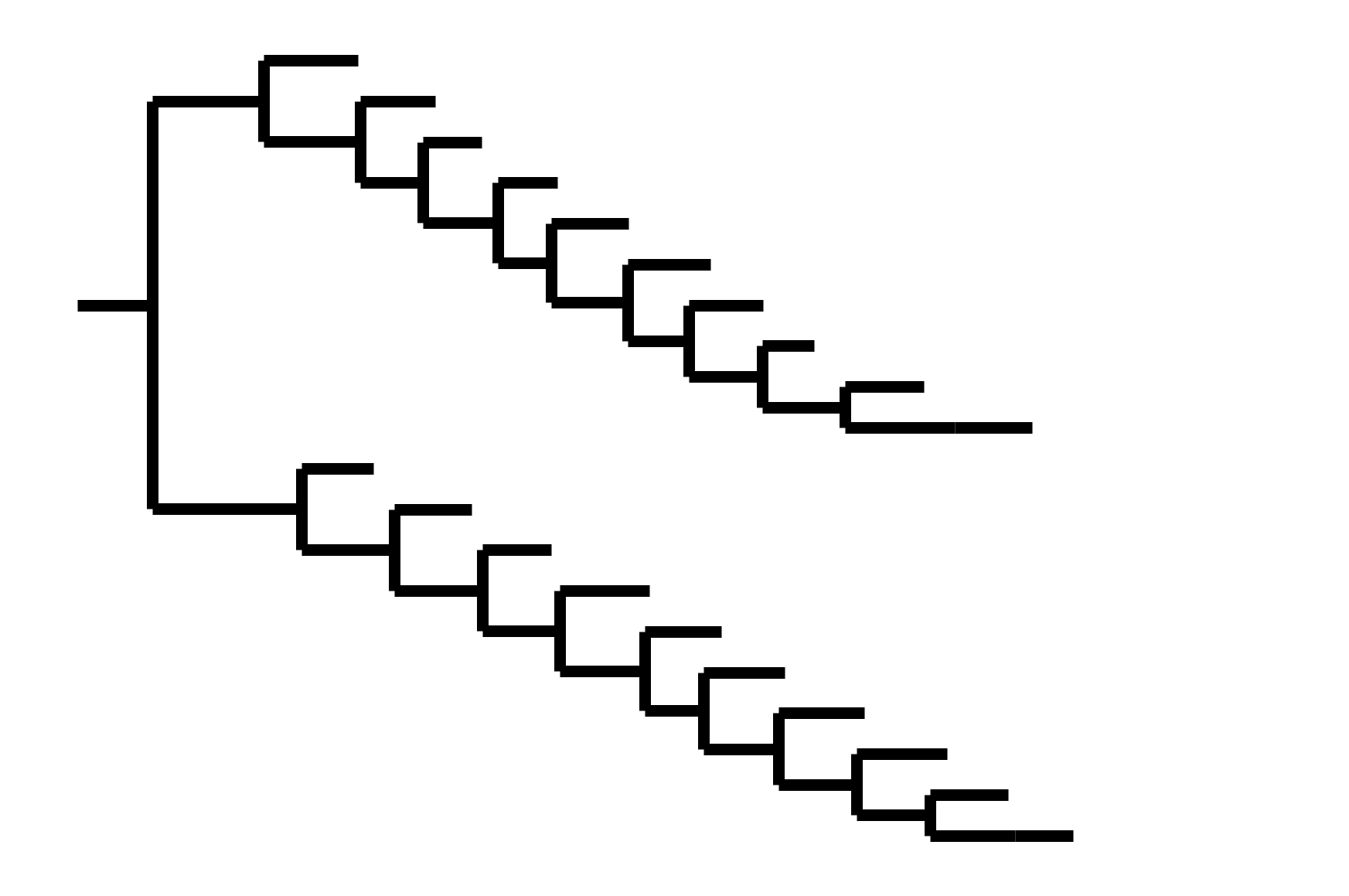
CoV-229E has ladder-like tree:
- new variants displace old ones
- new variants descend from recent successful ones
Human influenza A evolves this way too. It's theoretically possible to pick single well-matched vaccine strain.
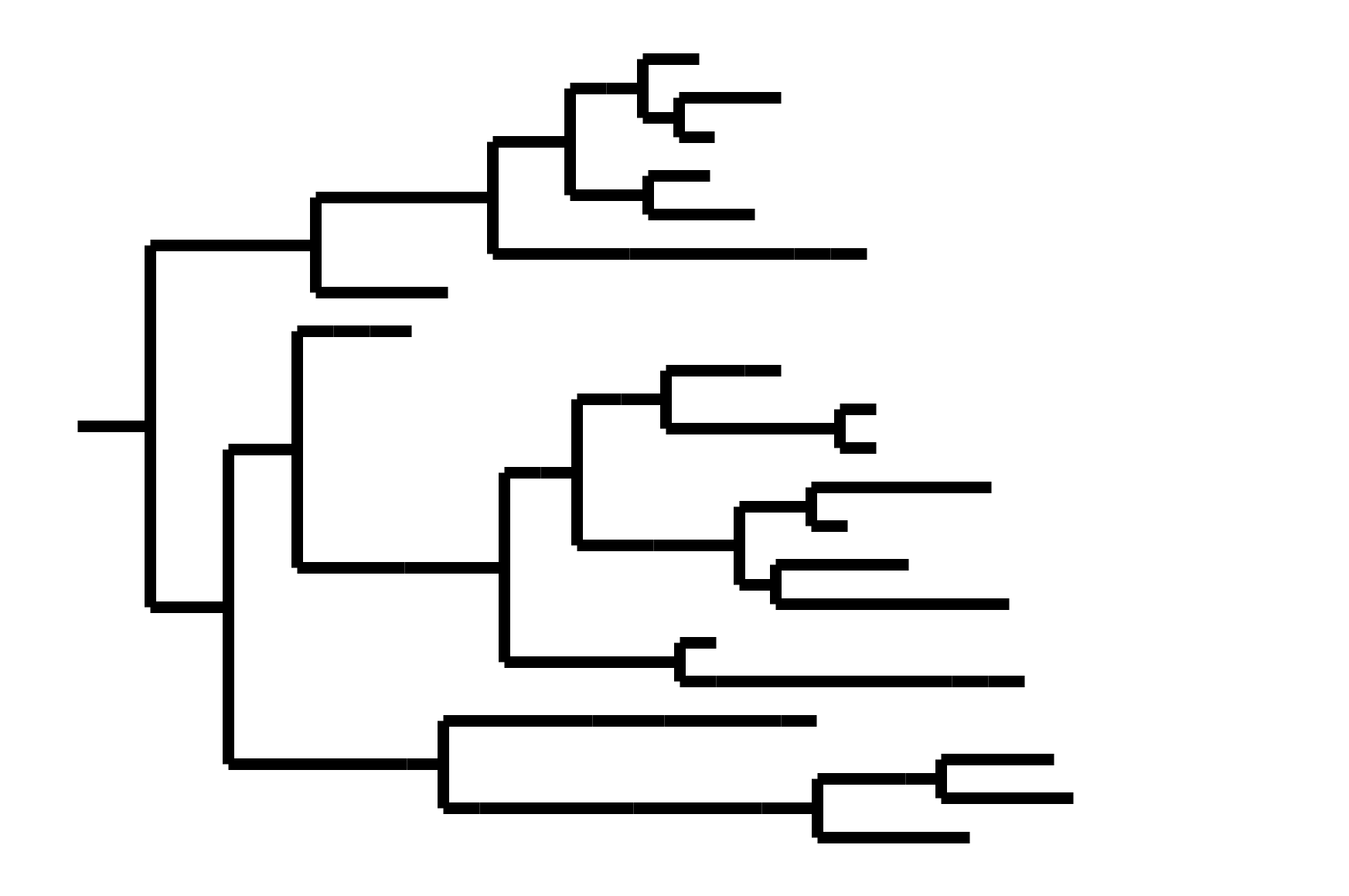
CoV-OC43 split into two ladder-like lineages. Influenza B evolves this way too. It's theoretically possible to pick well-matched bivalent vaccine.
Phylogenetic tree shape and vaccine strategy
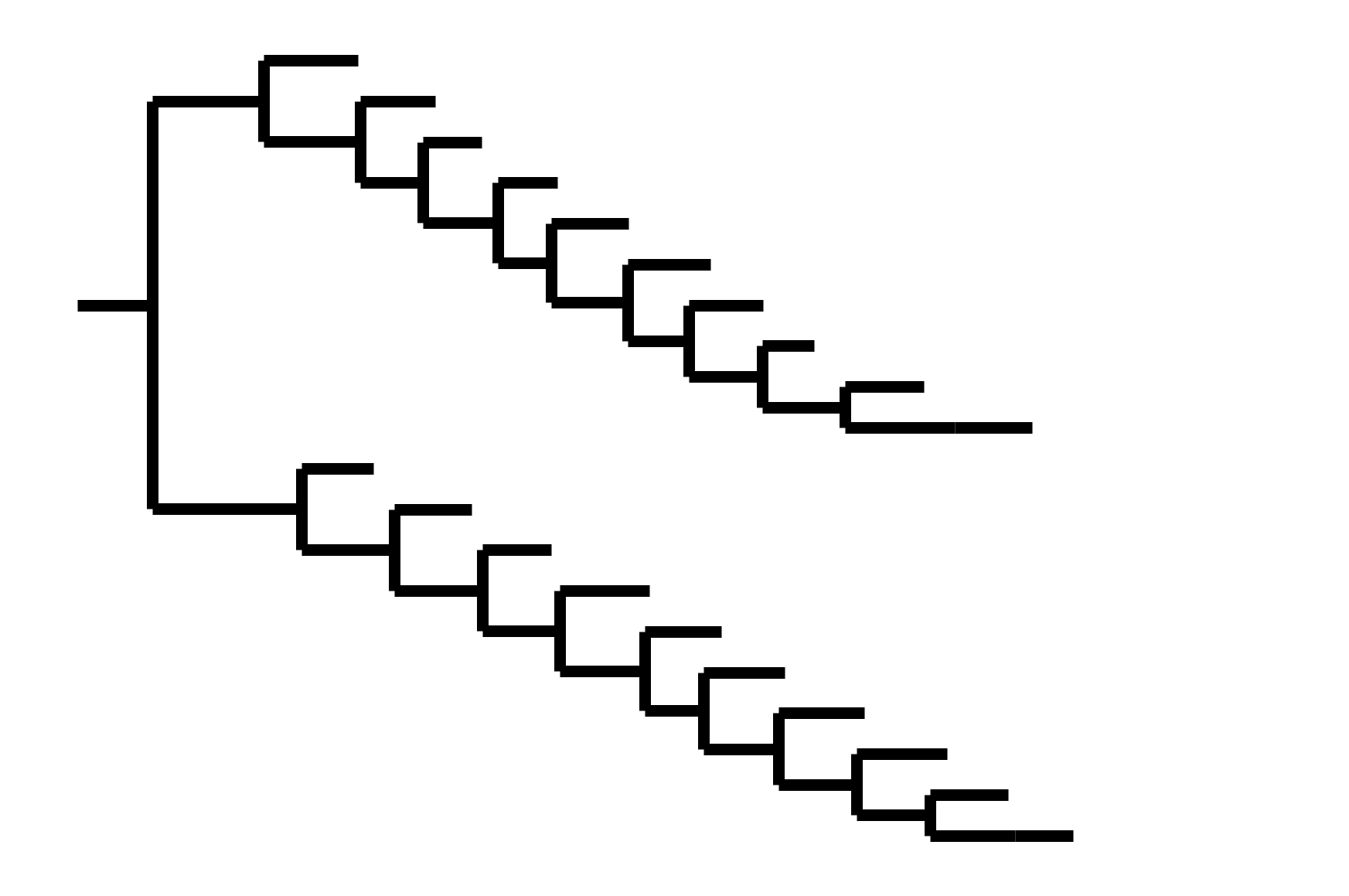
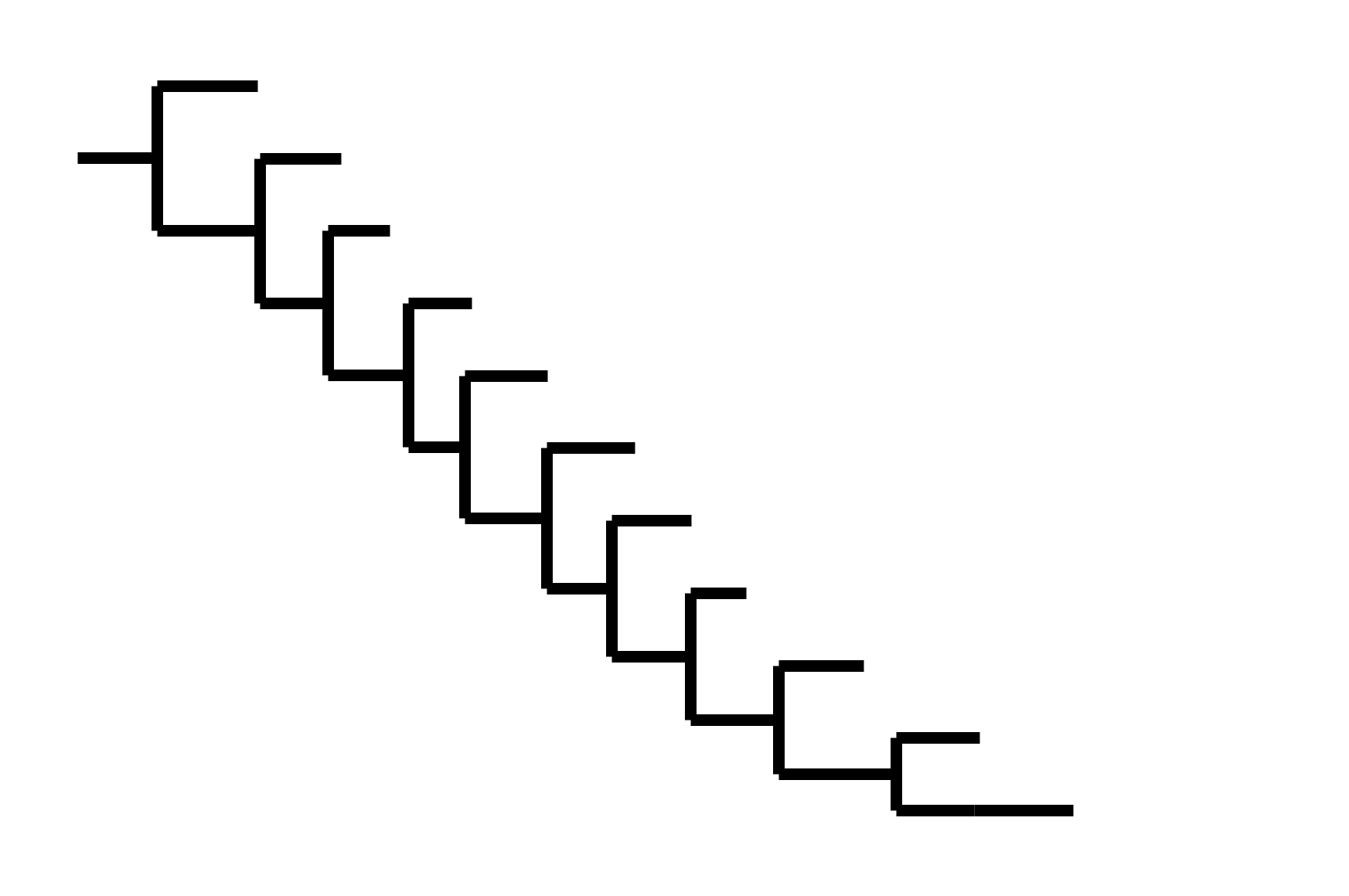
CoV-229E has ladder-like tree:
- new variants displace old ones
- new variants descend from recent successful ones
Human influenza A evolves this way too. It's theoretically possible to pick single well-matched vaccine strain.
CoV-OC43 split into two ladder-like lineages. Influenza B evolves this way too. It's theoretically possible to pick well-matched bivalent vaccine.
In non-ladder-like tree, next variant not descended from recent successful one. Makes picking vaccine strains difficult.
After early fixation of D614G, the SARS-CoV-2 tree has not been ladder-like

Take-aways on general principles
Other antigenically evolving human respiratory viruses have ladder-like phylogenetic trees, which is key to enabling vaccine updates as it provides some level of predictability (the next variant usually descended from the last one).
So far SARS-CoV-2 has defied ladder-like paradigm: Omicron not descended from Delta; Delta not descended from Alpha. However, it's still early and we are seeing combined selection for antibody escape and increased transmissibility--presumably transmissibility will eventually plateau. Despite having been wrong in thinking next variant would come from Delta, I still think evolution will be mostly ladder-like.
Outline
- Principles of viral antigenic evolution and emergence of Omicron
- Importance of the SARS-CoV-2 receptor-binding domain (RBD)
- Mapping antibody escape to interpret viral evolution
Strongest evolutionary selection is in RBD
Sites of evolutionary change in the spike of CoV-229E over the last four decades
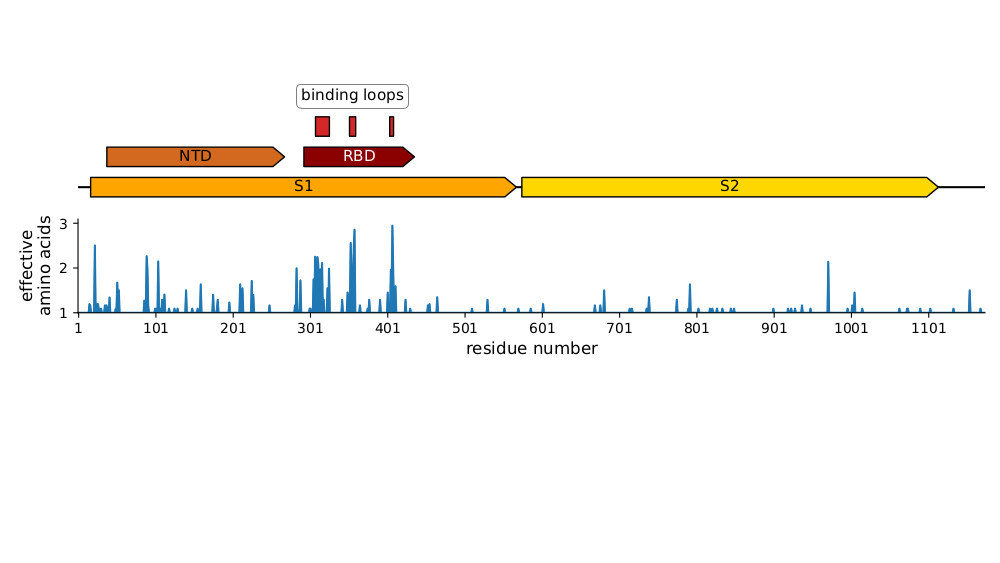
Strongest evolutionary selection is in RBD
Sites of evolutionary change in the spike of CoV-229E over the last four decades
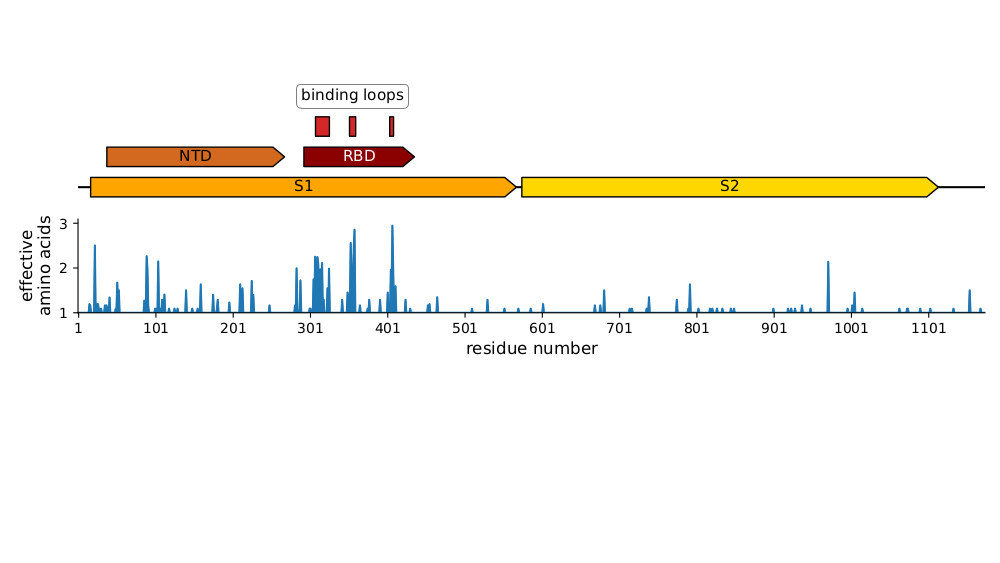
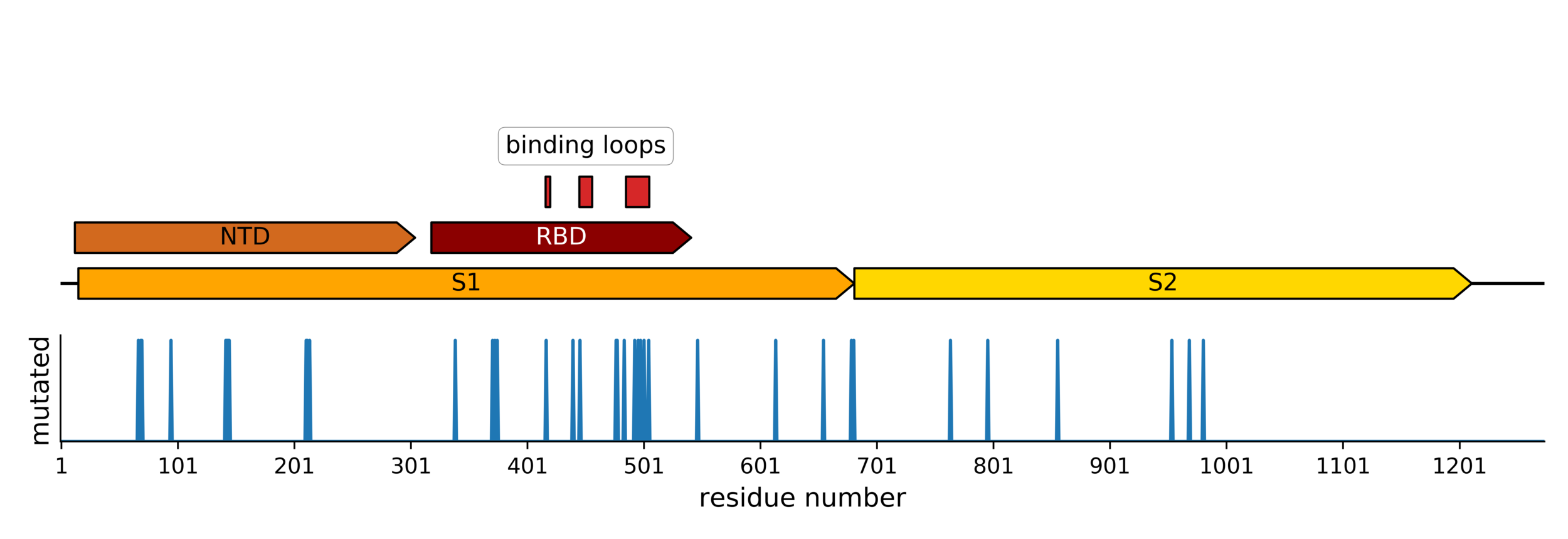
Sites of mutations in SARS-CoV-2 Omicron (BA.1) spike relative to Wuhan-Hu-1
Main difference is SARS-CoV-2 also fixing transmissibility-enhancing spike mutations that affect proteolytic processing and stabilize defects cause by furin-cleavage site
Majority of neutralizing antibody response in vaccinated/infected humans targets RBD
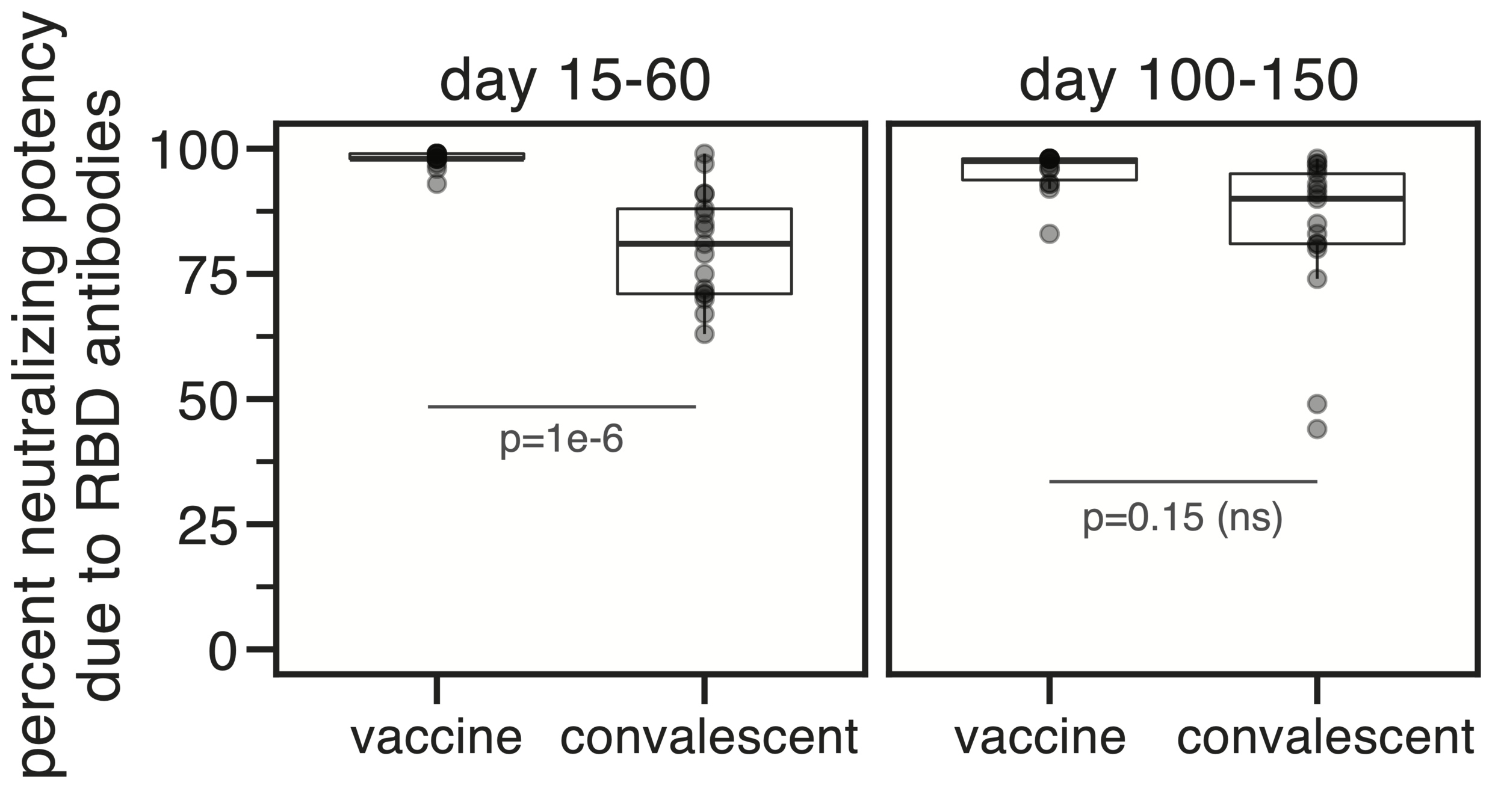
Importance of RBD
Human CoVs, which evolve to escape transmission-blocking immunity, show strongest selection in RBD. So virus is telling us RBD antibodies matter most for blocking transmission. But non-RBD antibodies and T-cells still matter, especially for reducing disease severity while putting less selection on virus.
Most neutralizing activity from RBD antibodies (although antibodies to other domains such as NTD can also be neutralizing).
However, a minority of all anti-spike antibodies elicited by current vaccines target RBD.
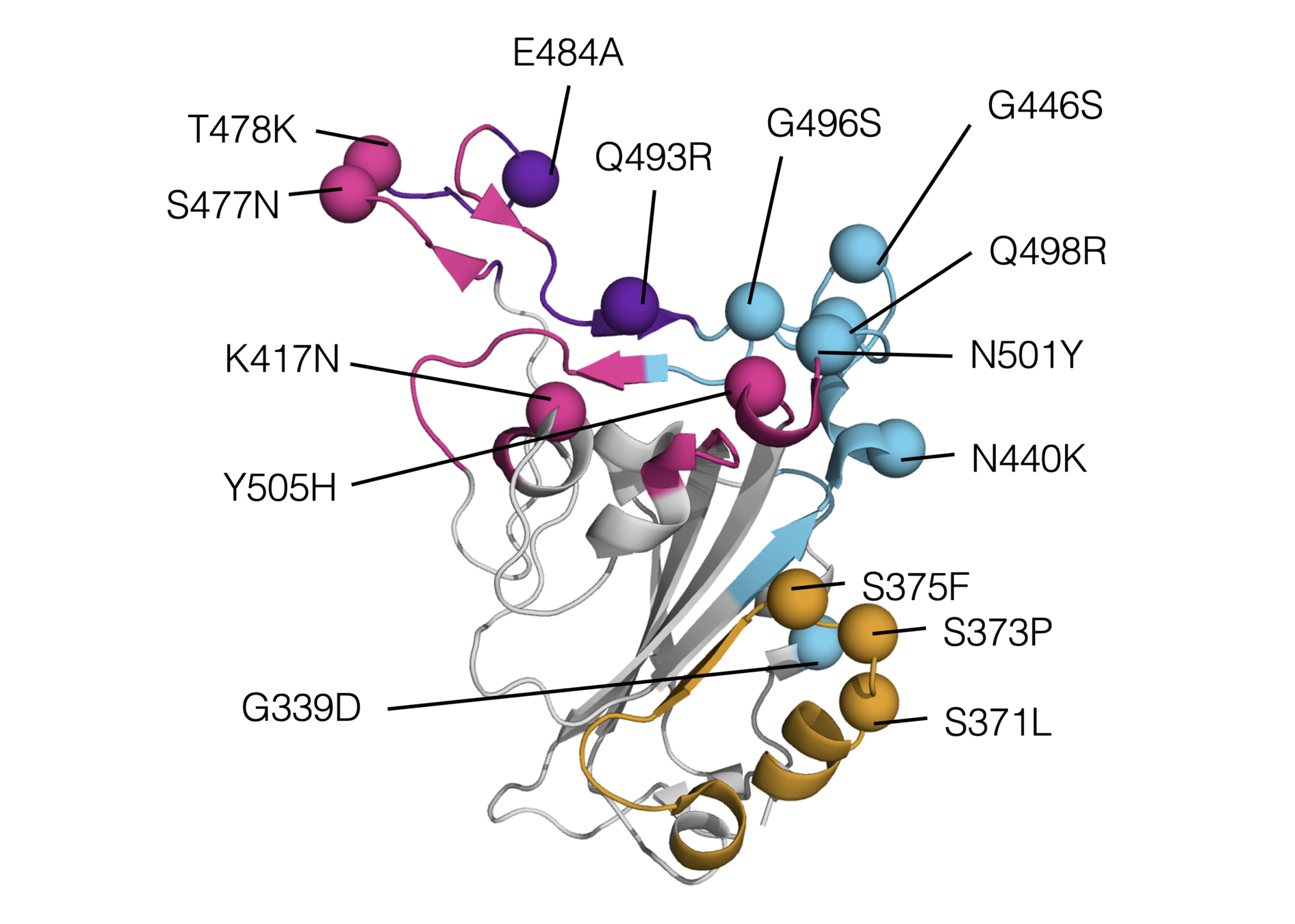
Omicron has a lot of mutations, especially in the receptor binding domain (RBD)
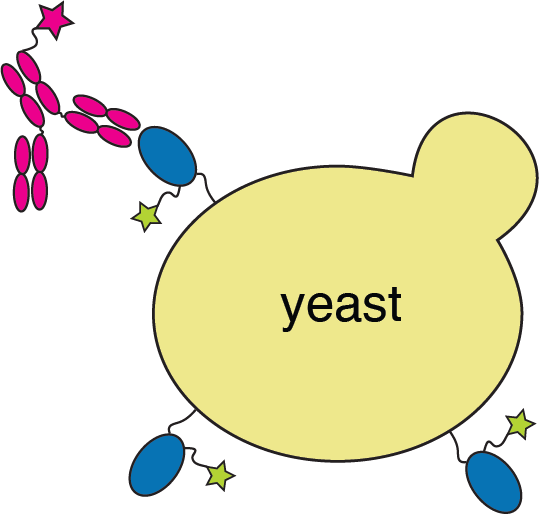
Deep mutational scanning measures how all mutations affect ACE2 affinity
RBD
fluorescent ACE2
yeast
fluorescent tag on RBD
Importantly, we use ACE2 titrations to measure true affinities, not just relative FACS binding signal; see here for details.
Deep mutational scanning measures how all mutations affect ACE2 affinity

Library of yeast each expressing a different RBD mutant. Click here for details on how library is made.
Deep mutational scanning measures how all mutations affect ACE2 affinity
Experimentally measured maps of how all mutations affect ACE2 affinity:
https://jbloomlab.github.io/SARS-CoV-2-RBD_DMS_variants/RBD-heatmaps/
How does Omicron bind ACE2 with so many mutations?
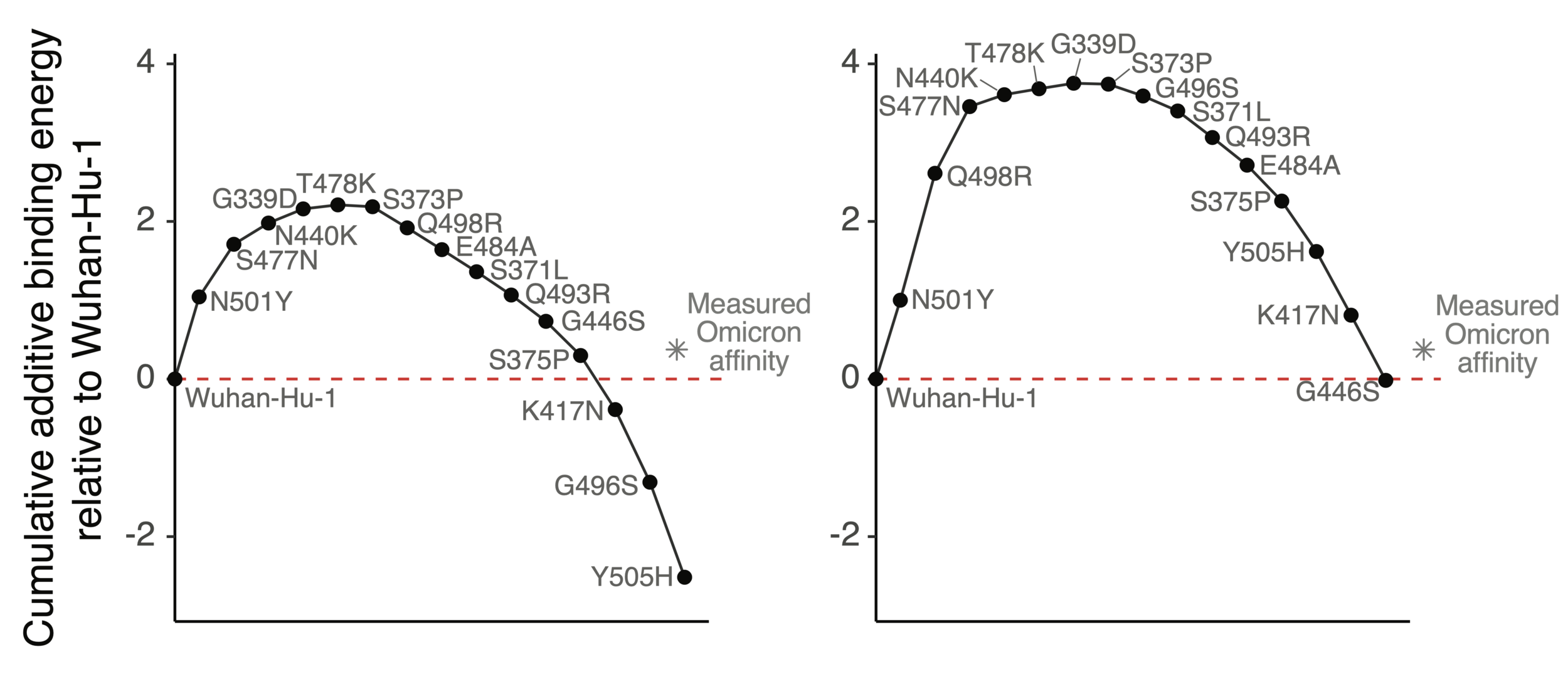
Mutations in Omicron have net negative effect on ACE2 binding if summed as single mutants
How does Omicron bind ACE2 with so many mutations?
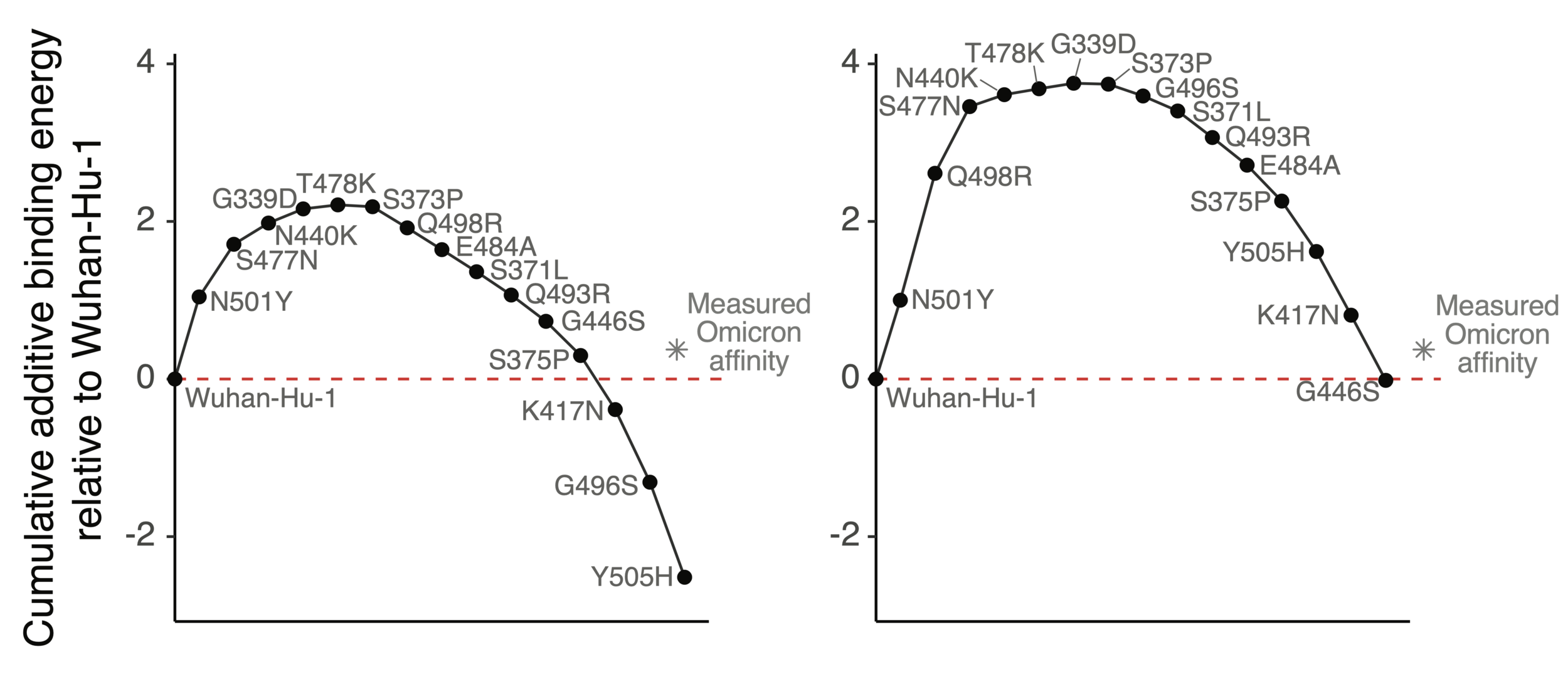
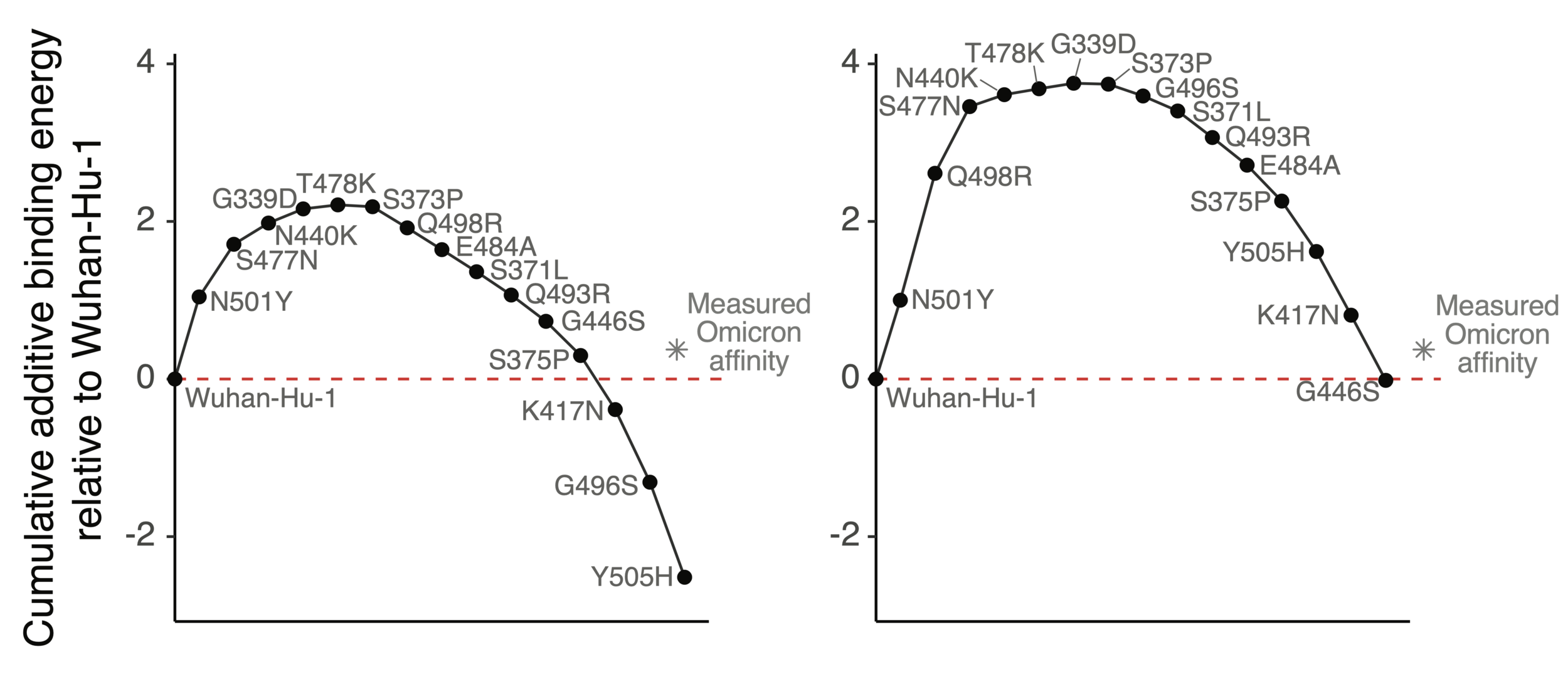
Mutations in Omicron have net negative effect on ACE2 binding if summed as single mutants
However, two mutations (Q498R & N501Y) work together so net effect ~zero when both present
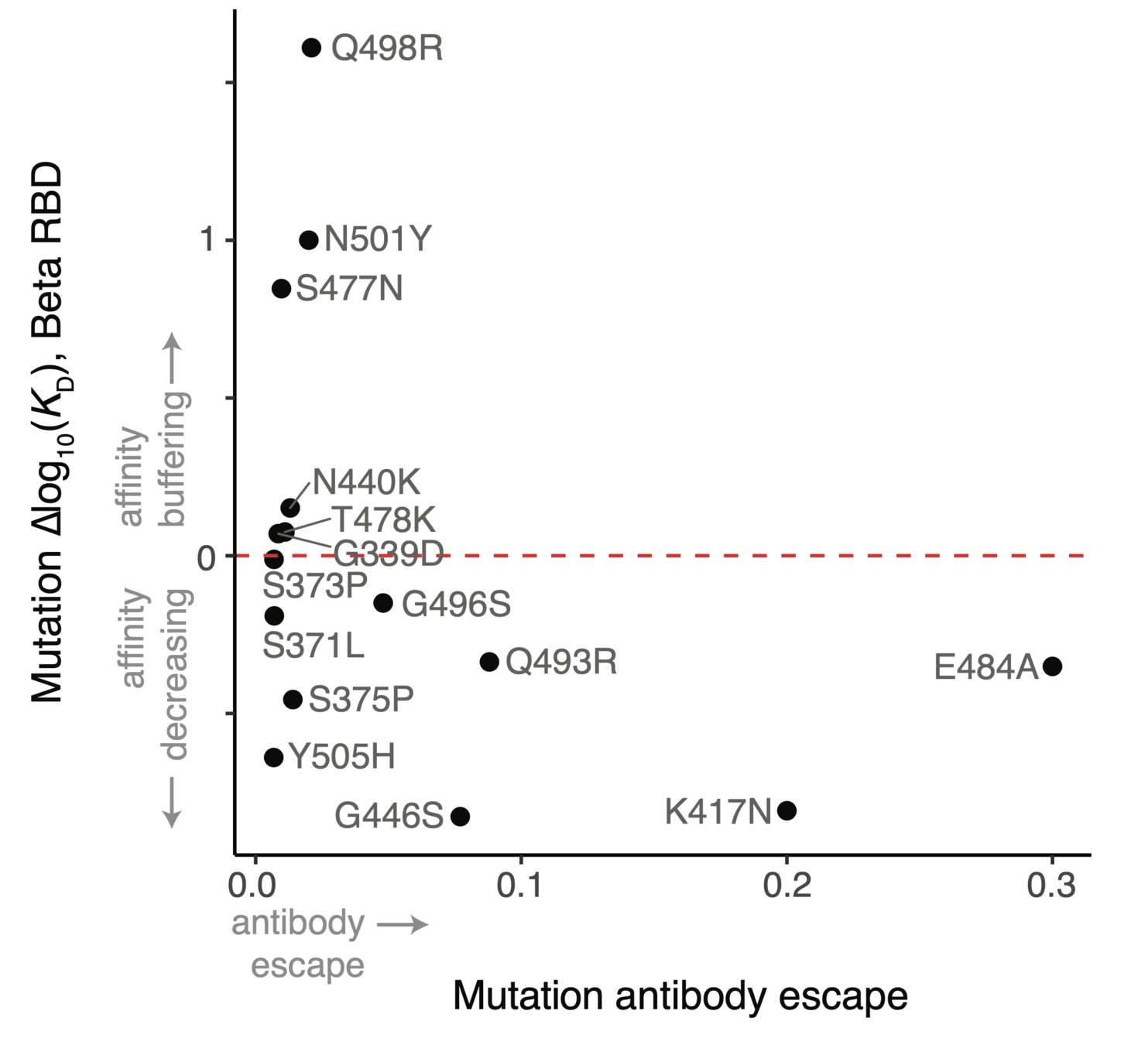
ACE2 affinity-enhancing mutations buffer antibody-escape mutations
RBD will not run out of evolutionary space
25 of 31 residues in CoV-229E RBD that contact receptor varied during virus's evolution in humans over last ~50 years (Li et al, eLife, 2019)
There are lots of mutations to SARS-CoV-2 RBD that retain (and sometimes even enhance) ACE2 affinity (Starr et al, 2020)
Outline
- Principles of viral antigenic evolution and emergence of Omicron
- Importance of the SARS-CoV-2 receptor-binding domain (RBD)
- Mapping antibody escape to interpret viral evolution
We map escape mutations by sorting for RBD variants that don't bind antibody
RBD
fluorescently labeled antibody
yeast
fluorescent tag on RBD
Escape map from a single antibody
Escape maps from lots of antibodies
Infection / vaccination elicit polyclonal antibodies that can bind many epitopes
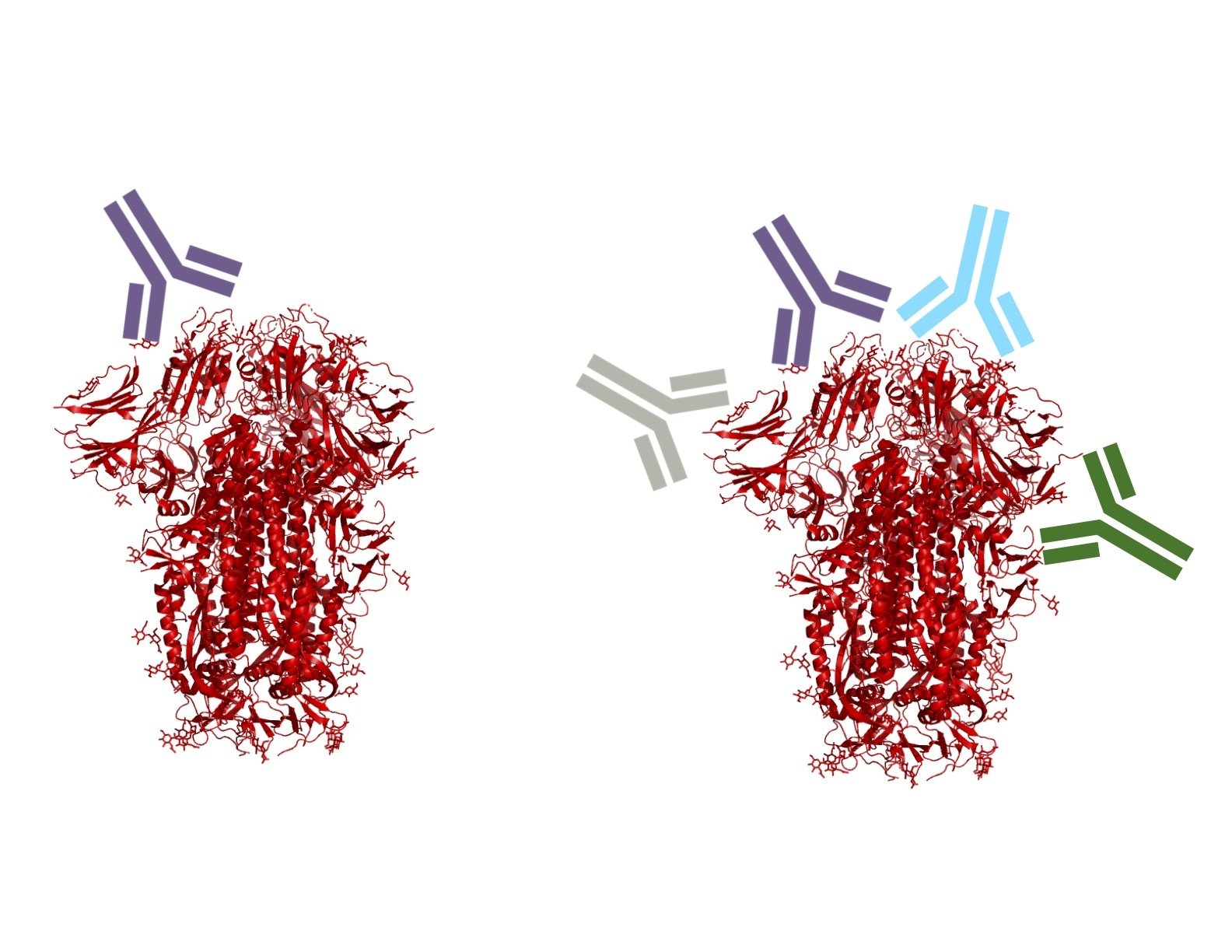
Monoclonal antibodies bind one epitope, so can usually be escaped by single mutation
Polyclonal antibodies can bind many epitopes, so often more resistant to escape
If polyclonal antibodies bind multiple epitopes, escape needs multiple mutations
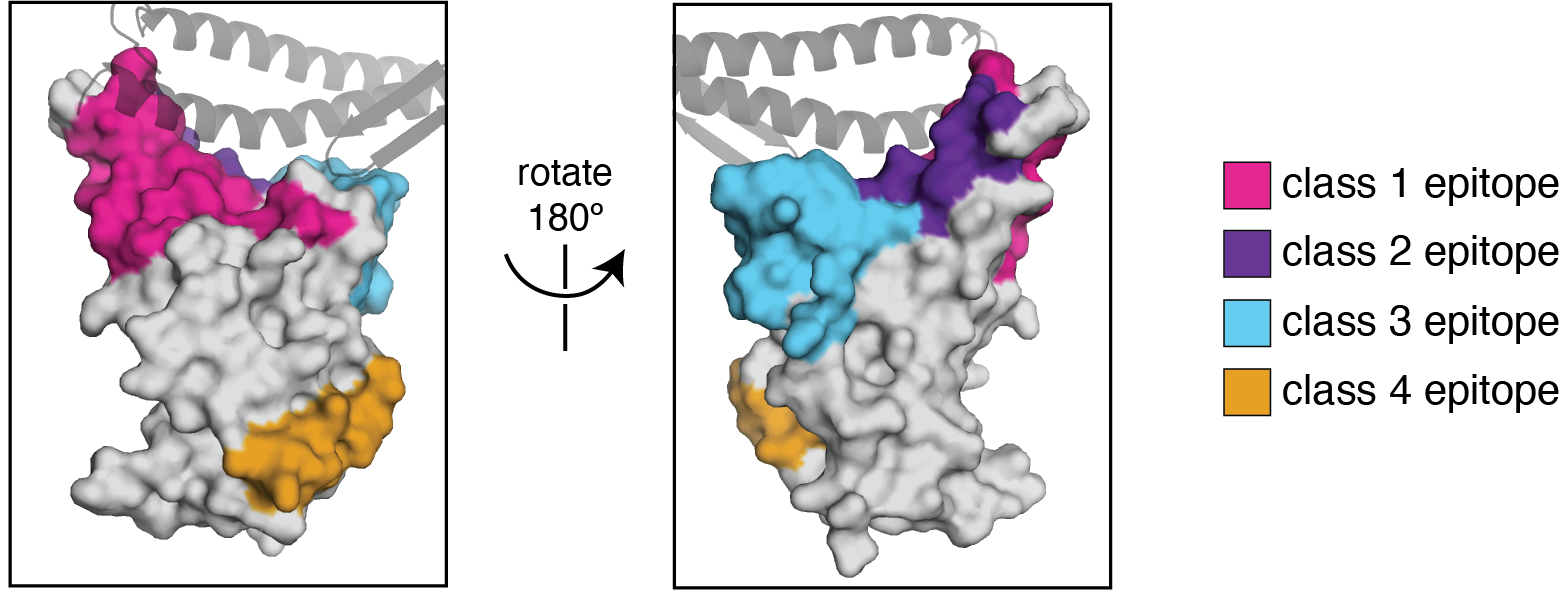
We use the antibody classification scheme from Barnes et al Nature (2020). The extension of these antibody classes to escape mapping is in Greaney et al (2021), and escape maps are available here. Class 1, 2, and 3 antibodies are often potently neutralizing, while class 4 antibodies are less neutralizing (see: Piccoli et al (2020), Dejnirattisai et al (2021), Liu et al (2020), Zost, et al (2020)).
We know where in RBD antibodies elicited by current Wuhan-Hu-1-like vaccines bind
Plot from escape calculator described in Greaney et al (2022)


Delta only has modest mutations at antigenically important RBD sites
Plot from escape calculator described in Greaney et al (2022)

Omicron (BA.1) is extensively mutated at important RBD antigenic sites
Plot from escape calculator described in Greaney et al (2022)

Omicron (BA.2) shares most but not all key RBD antigenic mutations with BA.1
Plot from escape calculator described in Greaney et al (2022)
We expect future evolution to involve mutations that escape antibodies from current vaccines that still neutralize Omicron
Sites of escape from pre-Omicron antibodies that still neutralize Omicron
Plot from escape calculator described in Greaney et al (2022)
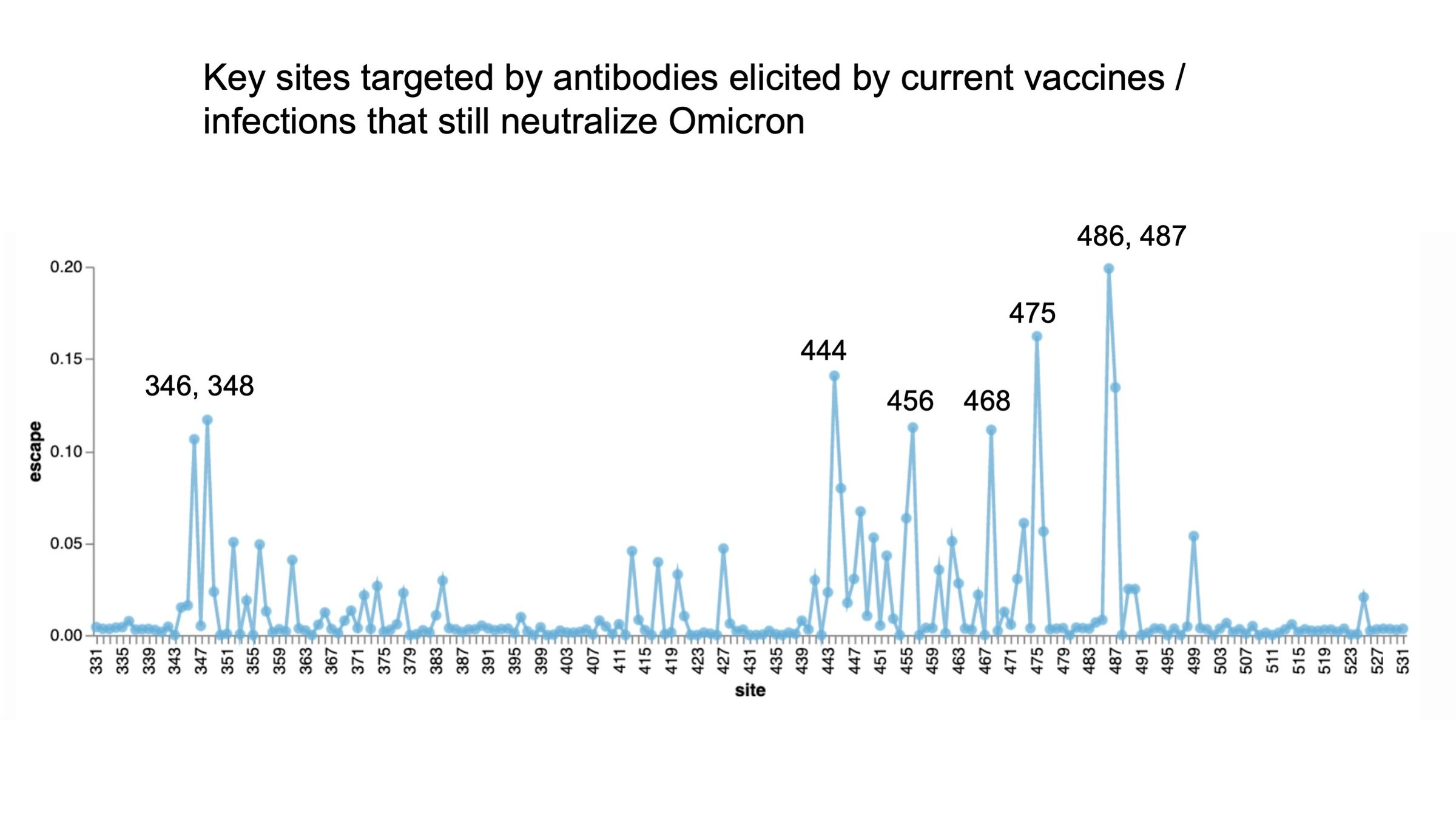
Sites of escape from pre-Omicron antibodies that still neutralize Omicron
Plot from escape calculator described in Greaney et al (2022)
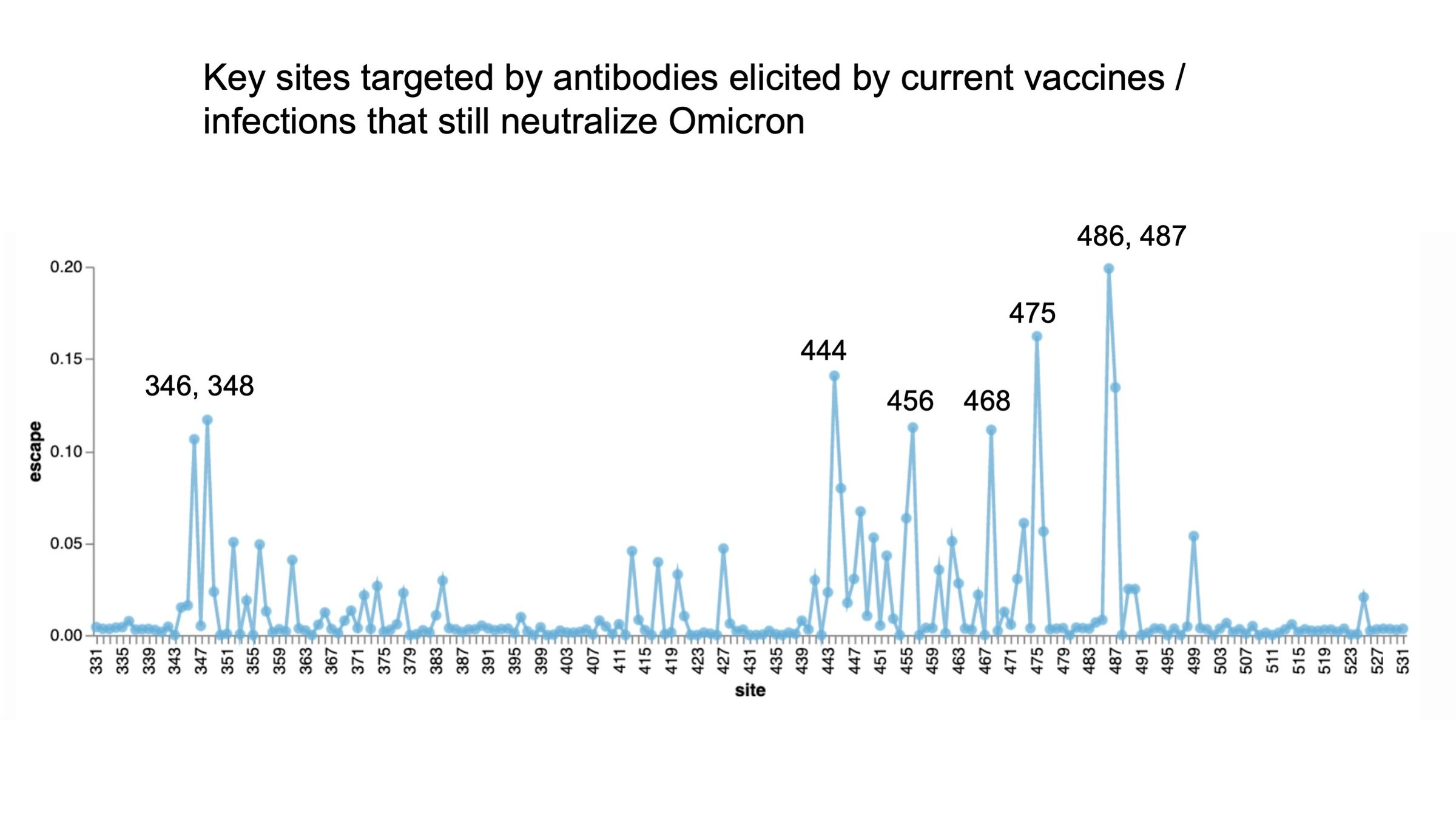
346 and 486 already mutated in Omicron variants
Conclusions...
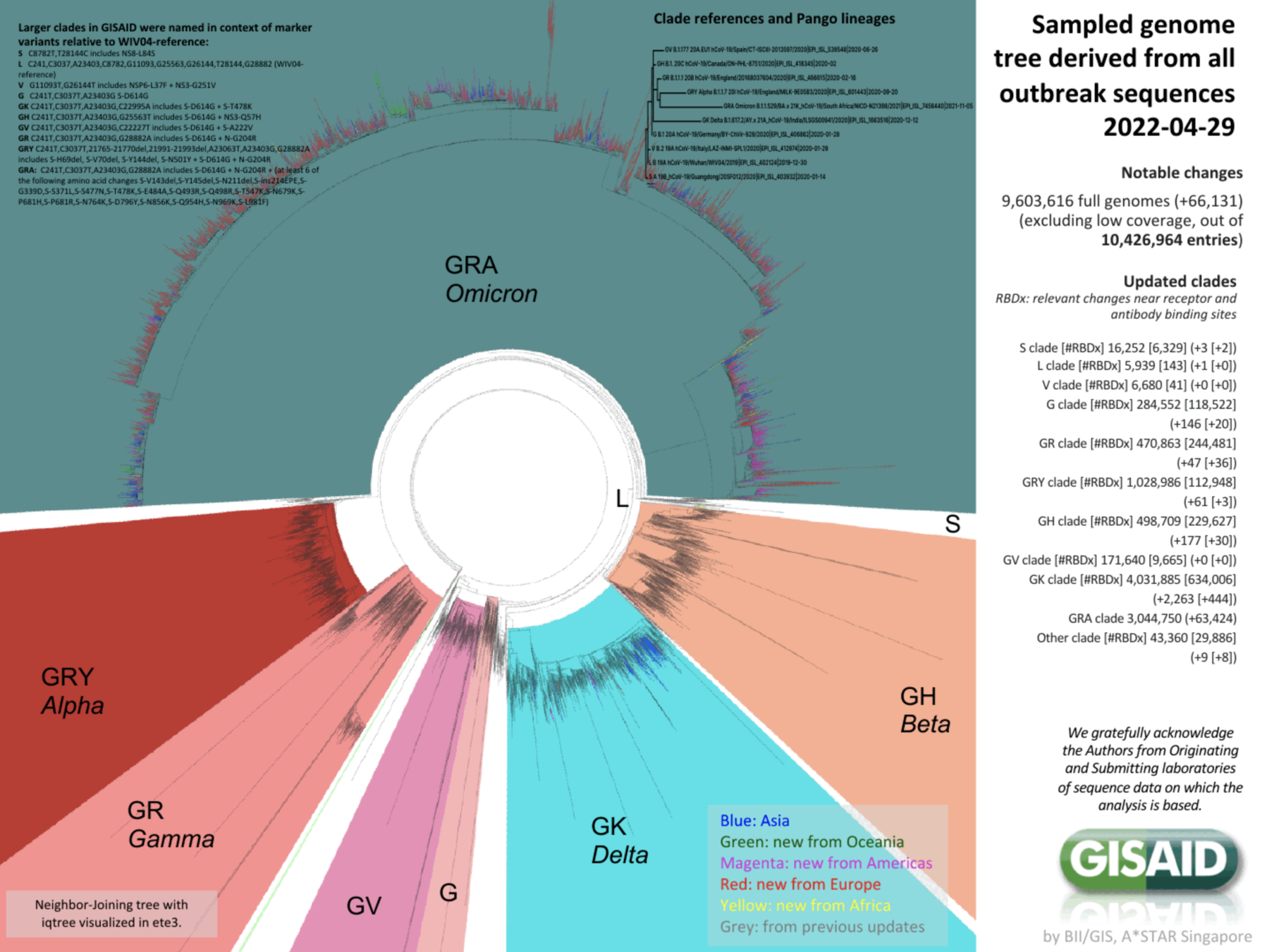
We can now monitor viral evolution at sequence level in great detail
nearly 10-million SARS-CoV-2 sequences!
Challenge is now to interpret antigenic and functional consequences of all those mutations... I've described a start.

Crowe lab (Vanderbilt)
Chu lab (Univ Wash)
Veesler lab (Univ Wash)
King lab (Univ Wash)
Li lab (Brigham & Women's)
Boeckh lab (Fred Hutch)
Alex Greninger (Univ Wash)
Nussenzweig lab (Rockefeller)
Bjorkman lab (Caltech)






Tyler Starr
Allie Greaney
Rachel Eguia
Bloom lab (Fred Hutch)

Sarah Hilton
Kate Crawford


Andrea Loes