BOOM BOOM
FoRT Trial: 4 Gy vs 24 Gy Radiotherapy for Follicular and Marginal Zone Lymphoma
Hoskin et al., Lancet Oncology 2021
Introduction & Methods
- Background: Low-dose radiotherapy (4 Gy) has shown efficacy in small studies
- Objective: Compare 4 Gy vs 24 Gy radiotherapy for follicular and marginal zone lymphoma
- Study design: Multicenter, randomized, phase 3, non-inferiority trial
- Key eligibility: Histologically confirmed follicular or marginal zone lymphoma requiring radical or palliative radiotherapy
- Randomization: 1:1 ratio, stratified by histology and treatment intent
- Primary endpoint: Time to local progression
Introduction & Methods
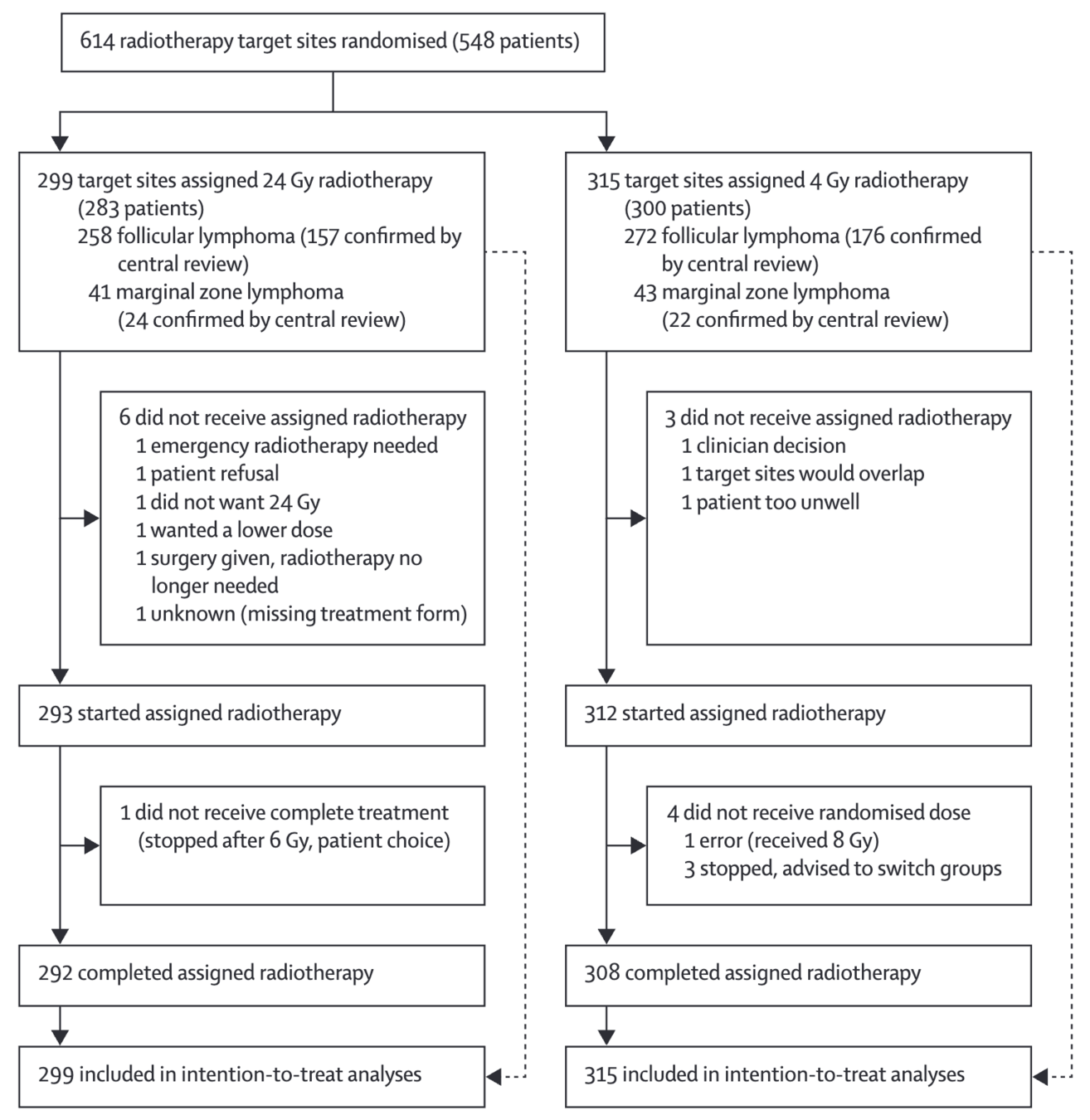
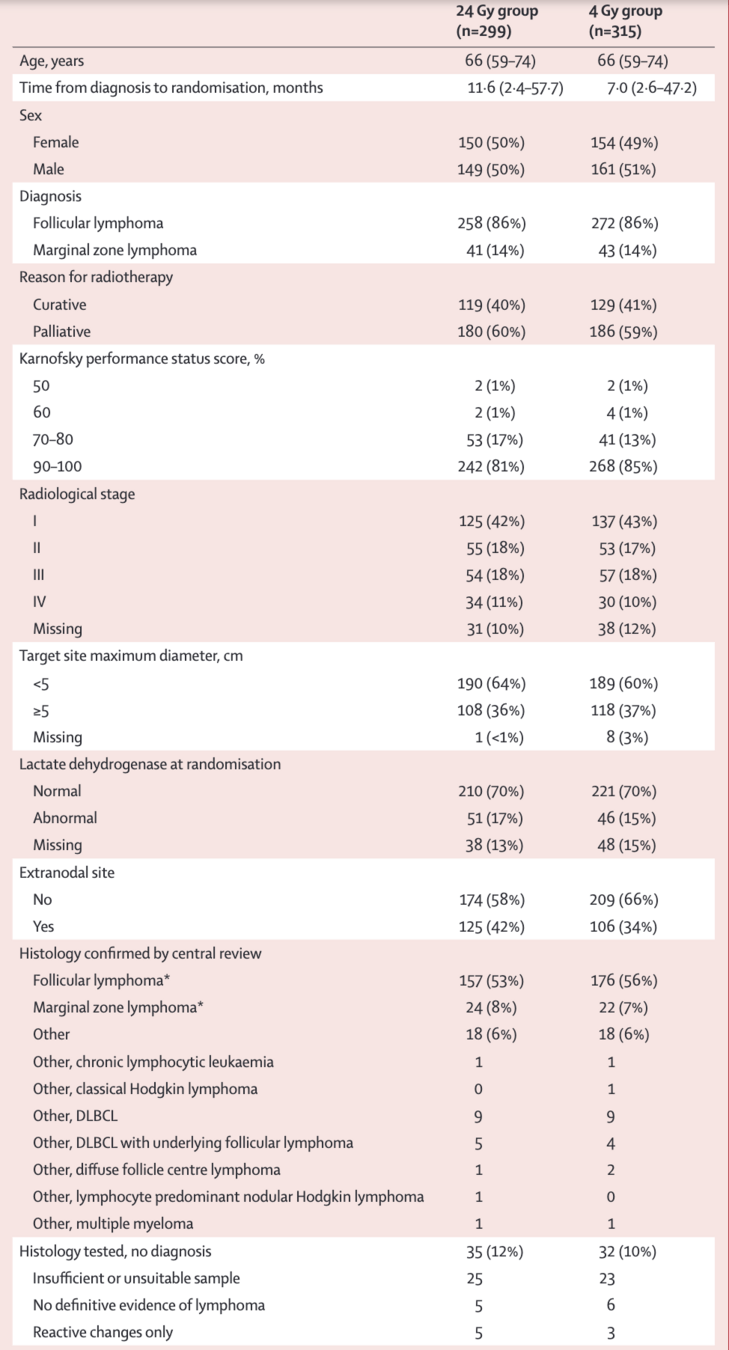
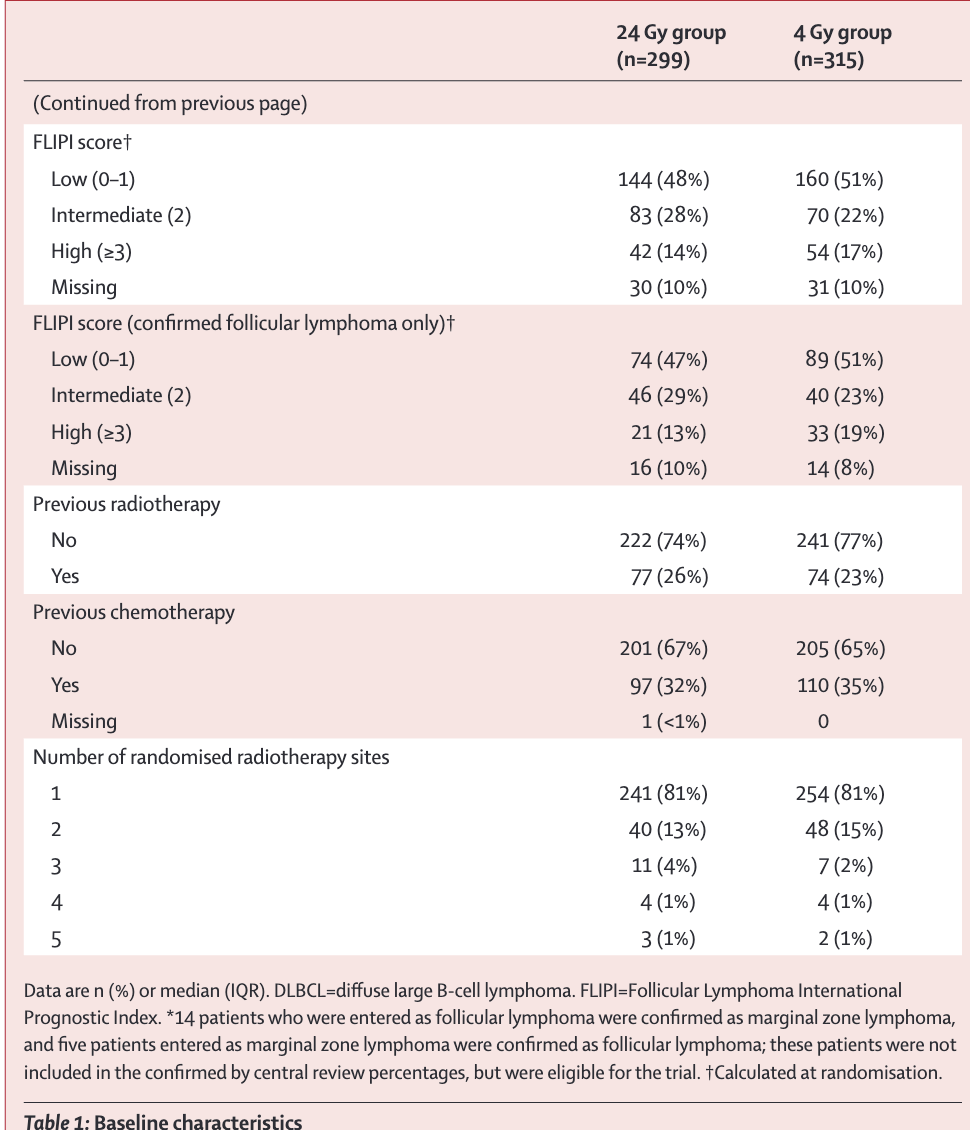
Patient Population
| Characteristic | 24 Gy (n=299) | 4 Gy (n=315) |
|---|---|---|
| Median age (years) | 66 | 66 |
| Follicular lymphoma | 258 (86%) | 272 (86%) |
| Marginal zone lymphoma | 41 (14%) | 43 (14%) |
| Curative intent | 119 (40%) | 129 (41%) |
| Palliative intent | 180 (60%) | 186 (59%) |
Patient Population
Interventions
- 24 Gy arm: 12 fractions of 2 Gy, treating daily Monday to Friday
- 4 Gy arm: 2 fractions of 2 Gy on consecutive days
- Involved-field radiotherapy based on tumor mass
- Quality assurance program included
- Central histological review performed
Primary Outcome: Local Progression-Free Interval
- Median follow-up: 73.8 months
- 2-year local progression-free rate:
24 Gy: 94.1% (95% CI 90.6–96.4)
4 Gy: 79.8% (74.8–83.9) - 5-year local progression-free rate:
24 Gy: 89.9% (85.5–93.1)
4 Gy: 70.4% (64.7–75.4) - Hazard ratio: 3.46 (95% CI 2.25–5.33; p<0.0001)
- Non-inferiority not achieved: difference at 2 years -13.0% (95% CI -21.7 to -6.9)
Figure: Local Progression-Free Interval
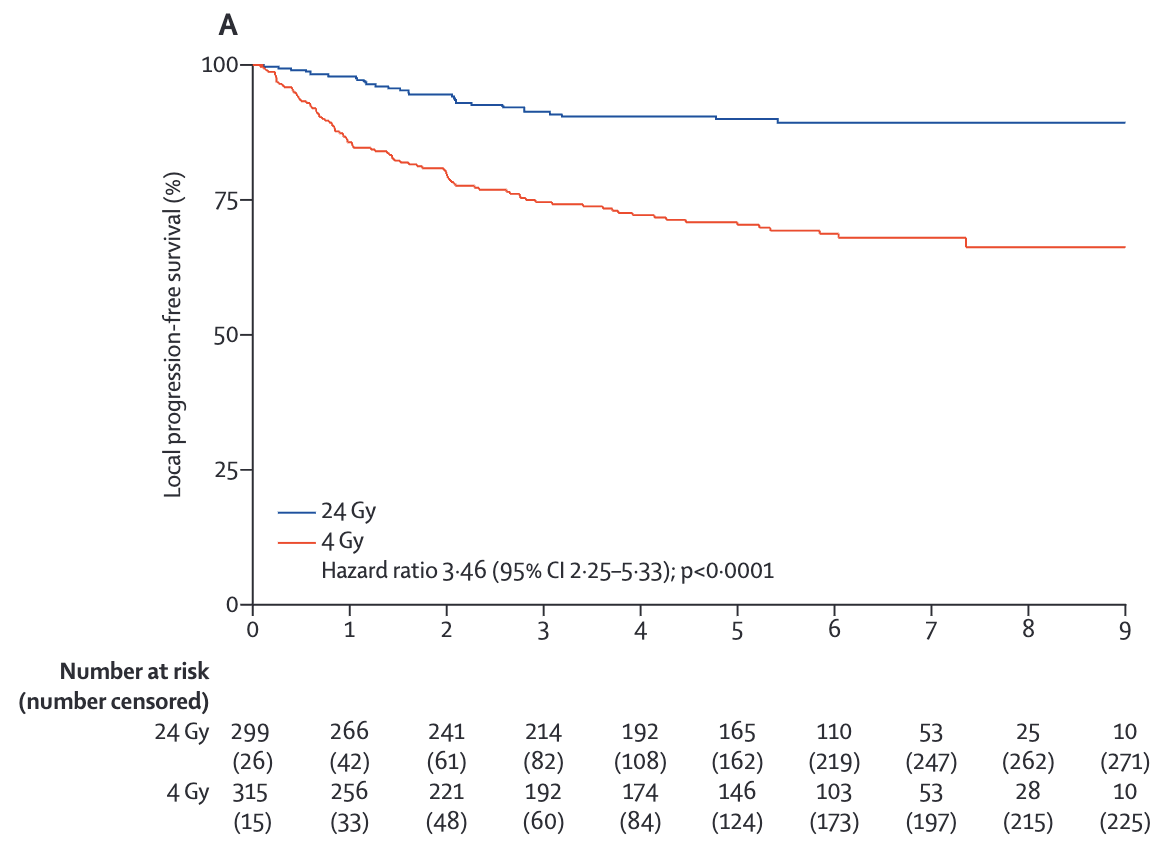
Figure: Local Progression-Free Interval
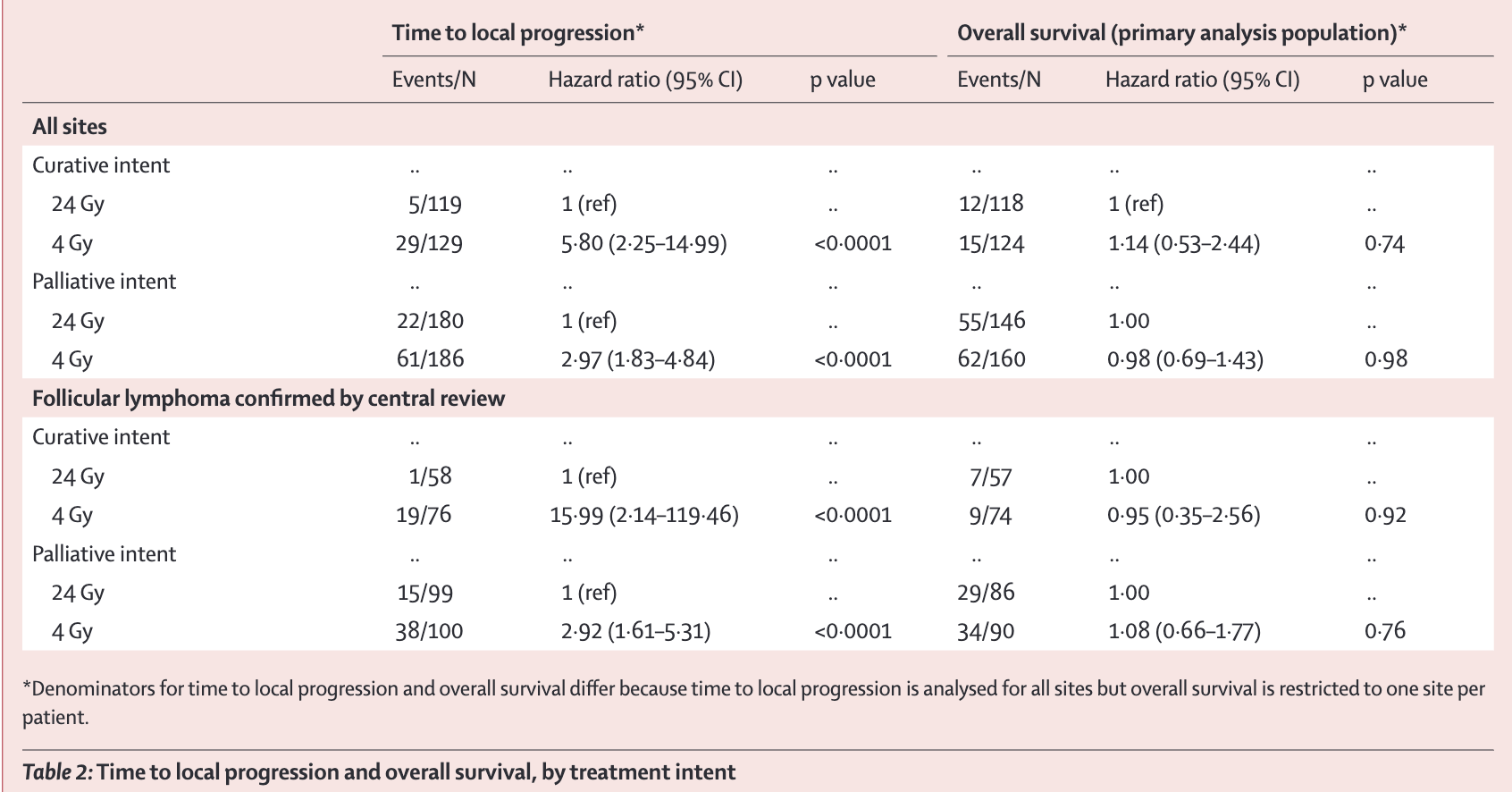
Secondary Outcomes
- Overall survival: No significant difference
HR 1.03 (95% CI 0.74–1.43; p=0.86) - Toxicity at 12 weeks:
24 Gy: 29 (10%) grade 2 or above events
4 Gy: 11 (4%) grade 2 or above events
p=0.0029 - Most common events at 12 weeks: alopecia, dry mouth, fatigue, mucositis, and pain
- No treatment-related deaths reported
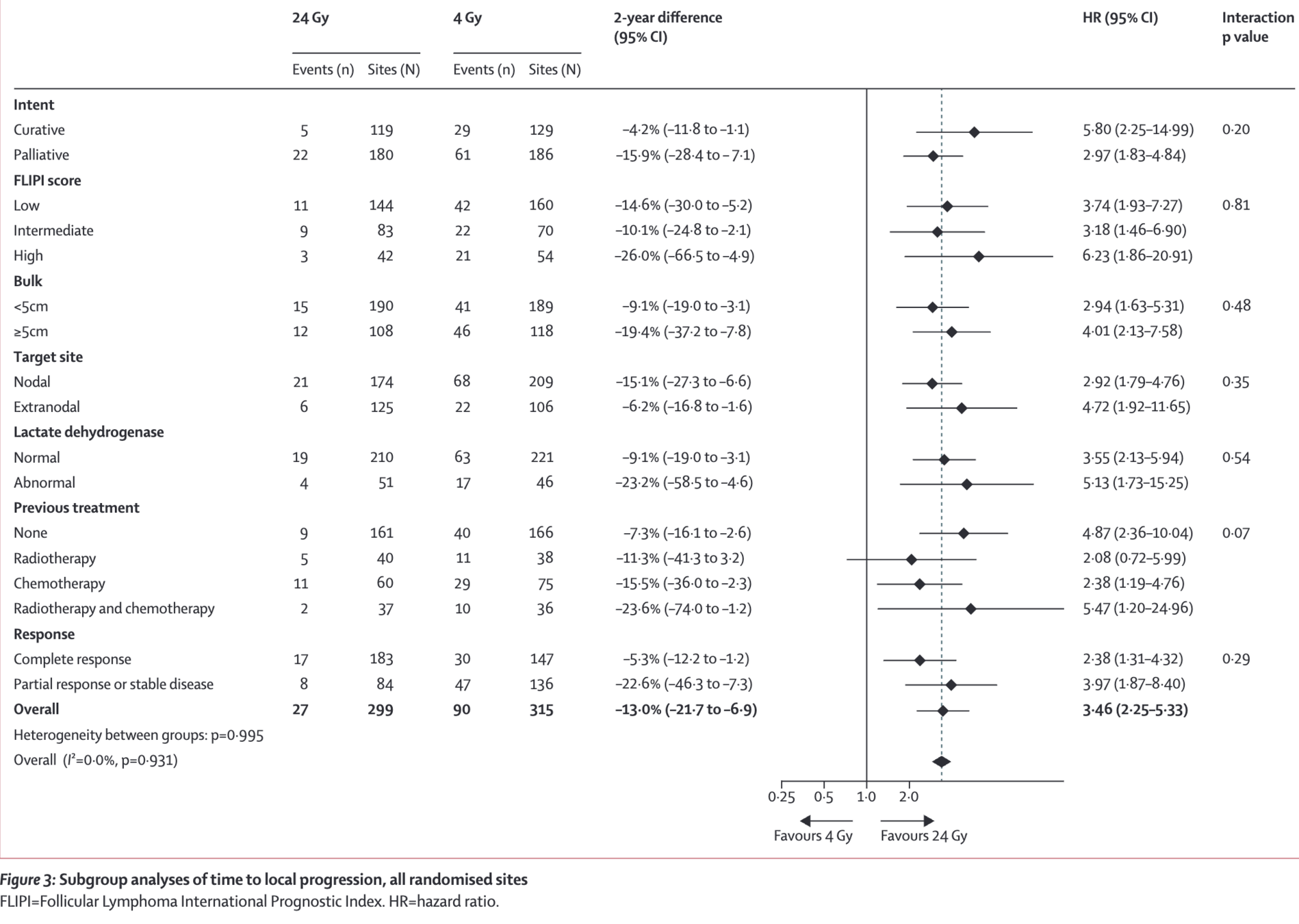
Subgroup Analyses
- Curative vs. palliative intent: Both showed significant benefit with 24 Gy
- Follicular vs. marginal zone lymphoma: Similar results in both histologies
- Orbital lymphoma: No progressions in 20 sites treated with 24 Gy, 2 progressions in 13 sites treated with 4 Gy
- No significant interactions found between treatment effect and subgroups
Figure: Subgroup Analyses
Conclusions
- 24 Gy remains the standard of care for durable local control in follicular and marginal zone lymphoma
- 4 Gy is inferior to 24 Gy in terms of local progression-free interval
- No difference in overall survival between the two arms
- 4 Gy may be considered in palliative settings where durable control is not paramount
- Similar results observed in follicular and marginal zone lymphoma subgroups
Strengths and Limitations
- Strengths:
- Large, multicenter, randomized trial
- Long-term follow-up (median 73.8 months)
- Inclusion of both follicular and marginal zone lymphoma
- Limitations:
- Premature closure (614 of 650 planned sites)
- Multiple randomizations allowed per patient
- Central histological confirmation in only 62% of cases
Implications for Practice
- 24 Gy in 12 fractions should remain the standard dose for durable local control
-
4 Gy in 2 fractions may be considered in palliative settings:
- When durable control is not the primary aim
- For patients with limited life expectancy
- In conjunction with systemic treatments
- Treatment decision should balance efficacy, toxicity, and patient factors
- Further research needed on optimal dose for specific subgroups (e.g., orbital lymphoma)
Discussion Points
-
How might these results impact current clinical practice?
-
Are there specific patient populations where 4 Gy might still be preferred?
-
What are the potential benefits and drawbacks of using 4 Gy in a palliative setting?
-
How do these findings compare to other studies on low-dose radiotherapy in indolent lymphomas?
-
What future research questions arise from this study?