Modern Linear Accelerator–Based Radiotherapy Is Safe and Effective in the Treatment of
Secretory and Nonsecretory Pituitary Adenomas
Janopaul-Naylor JR, Rupji M, Zhong J, Eaton BR, Ali N, Ioachimescu AG, Oyesiku NM, Shu HKG
World Neurosurg. 2022;160:e33-e39
Background
- Pituitary adenomas (PAs) can cause symptoms from:
- Compression of adjacent structures (optic apparatus, cranial nerves)
- Hypersecretion syndromes (hormonal excess)
- Previous studies mostly on Gamma Knife radiosurgery (GKRS)
- Limited modern data on LINAC-based approaches:
- LINAC fractionated RT
- LINAC stereotactic radiosurgery (SRS)
- Prior reports suggested functional tumors had worse local control
- Study aimed to report long-term outcomes with modern LINAC RT
Methods
- Single institution retrospective review (2003-2017)
- Inclusion: LINAC-based RT for histologically/clinically confirmed PA
- Minimum 3 years of MRI follow-up required
- Endpoints:
- Local control (LC): RECIST criteria on surveillance MRI
- Hormonal control: biochemical remission without medications
- Progression-free survival (PFS): time alive with LC without hormonal recurrence
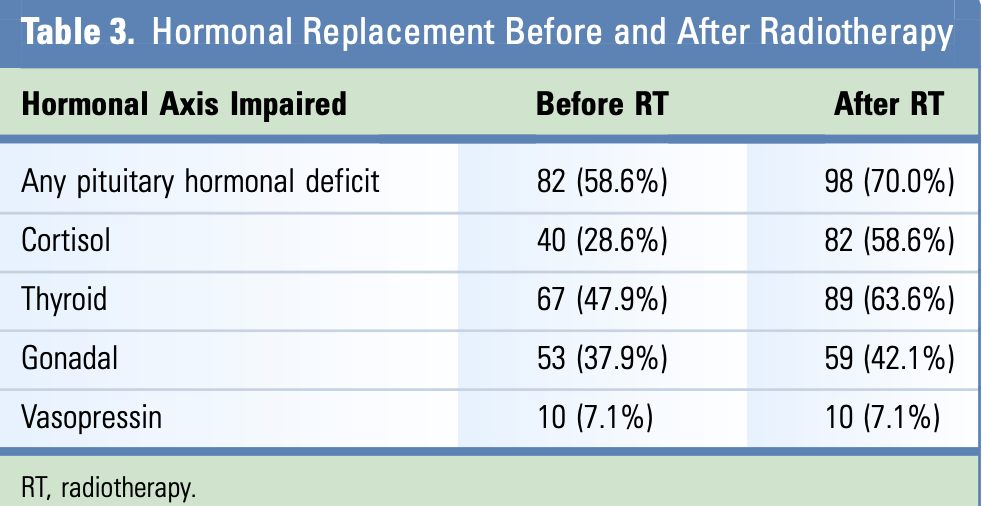
- Pituitary hormone deficiencies before and after RT
- Statistical analysis:
- Kaplan-Meier method for PFS and LC
- Cox proportional hazards models for associations with outcomes
Patient Population
- 140 patients with pituitary adenomas:
- 94 nonsecretory (67.1%)
- 46 secretory (32.9%): 23 GH-secreting, 13 ACTH-secreting, 9 prolactin-secreting, 1 TSH-secreting
- Median age: 46.5 years
- Gender: 51.4% female, 48.6% male
- Most had prior surgery (135/140 patients)
- Median number of surgeries: 1.4
- Surgical details:
- Transsphenoidal approach: 94.8%
- Gross total resection: 17.9%
- Subtotal resection: 77.9%
- Median follow-up: 5.35 years (IQR 4.0-8.5 years)
Radiation Treatment Details
- RT technique:
- Fixed gantry intensity-modulated RT: 51.4%
- Dynamic conformal arcs: 9.3%
- Volumetric modulated arc therapy: 39.3%
- Type of radiotherapy:
- Fractionated RT: 75.0% (105 patients)
- SRS: 25.0% (35 patients)
- Target delineation:
- Co-registration of planning CT with diagnostic MRI
- SRS offered if minimum distance from tumor to optic apparatus >4mm
- PTV margins: 1-3mm for fractionated RT, 0-1mm for SRS
- Dose specifications:
- Nonsecretory tumors: median 50.4 Gy fractionated / 15 Gy SRS
- Secretory tumors: median 50.4-54 Gy fractionated / 15.5 Gy SRS
- Daily image guidance for setup accuracy
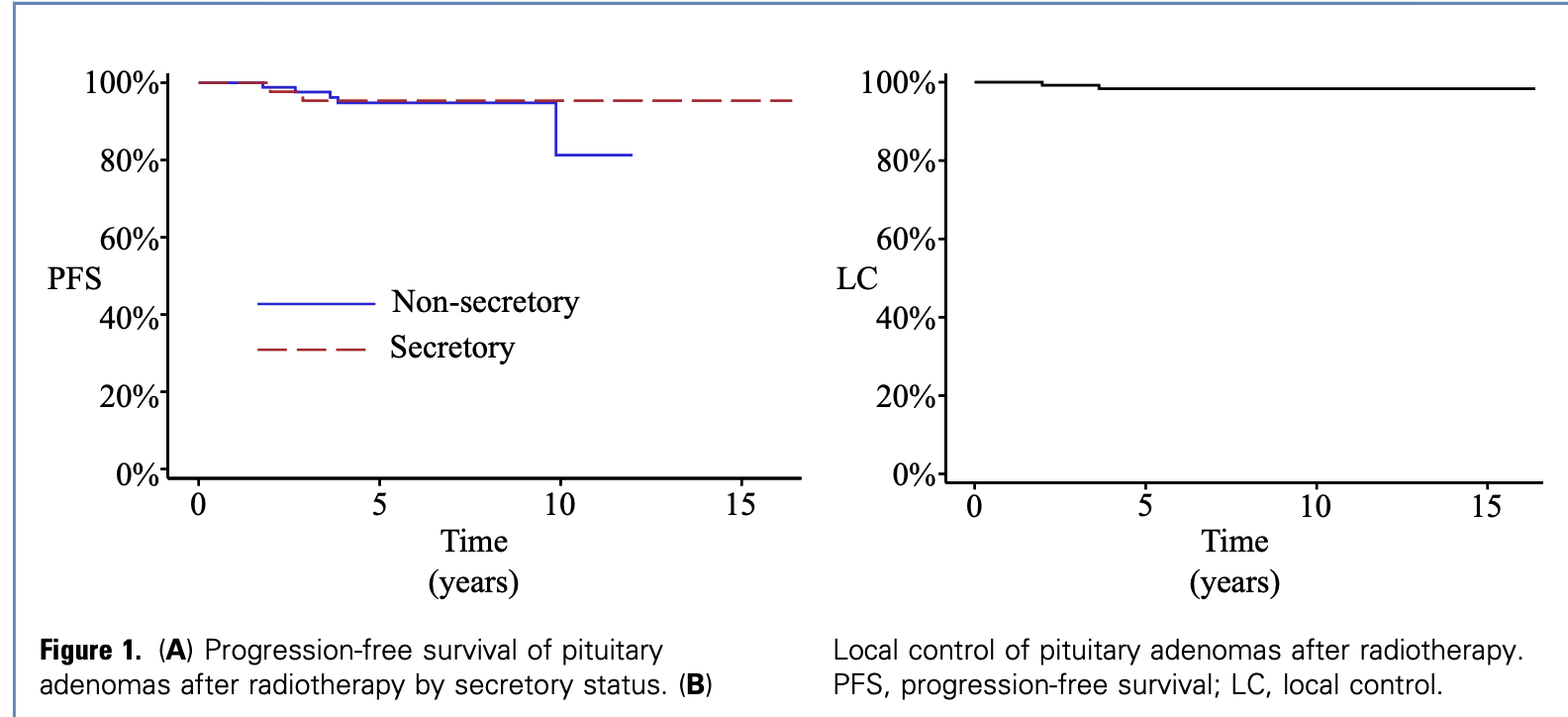
Progression-Free Survival
- No difference in PFS between secretory and nonsecretory groups (log rank p=0.70)
- 5-year PFS rates:
- Secretory tumors: 95.3%
- Nonsecretory tumors: 94.8%
- 10-year PFS rates:
- Secretory tumors: 95.3%
- Nonsecretory tumors: 81.3%
- On multivariable analysis, only larger PTV was associated with worse PFS (HR 2.60, 95% CI 1.08-6.28, p=0.03)
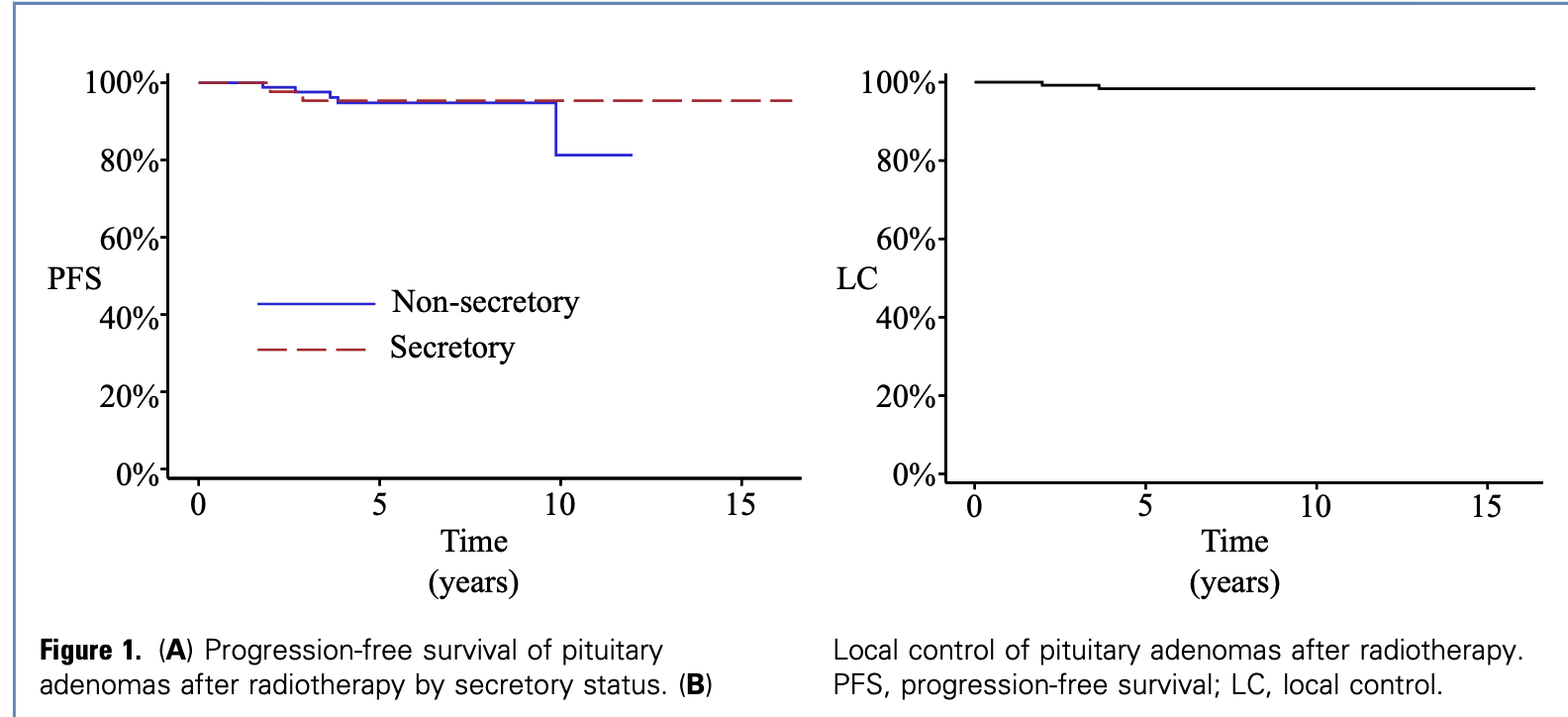
Local Control
- Only 3 local failures identified during follow-up
- 10-year actuarial LC rate: 98.3%
- No significant differences between secretory and nonsecretory tumors
- No association with type of radiotherapy (SRS vs fractionated)
- Equivalent high rates of LC with both modalities
Secondary outcome: Factors associated with PFS
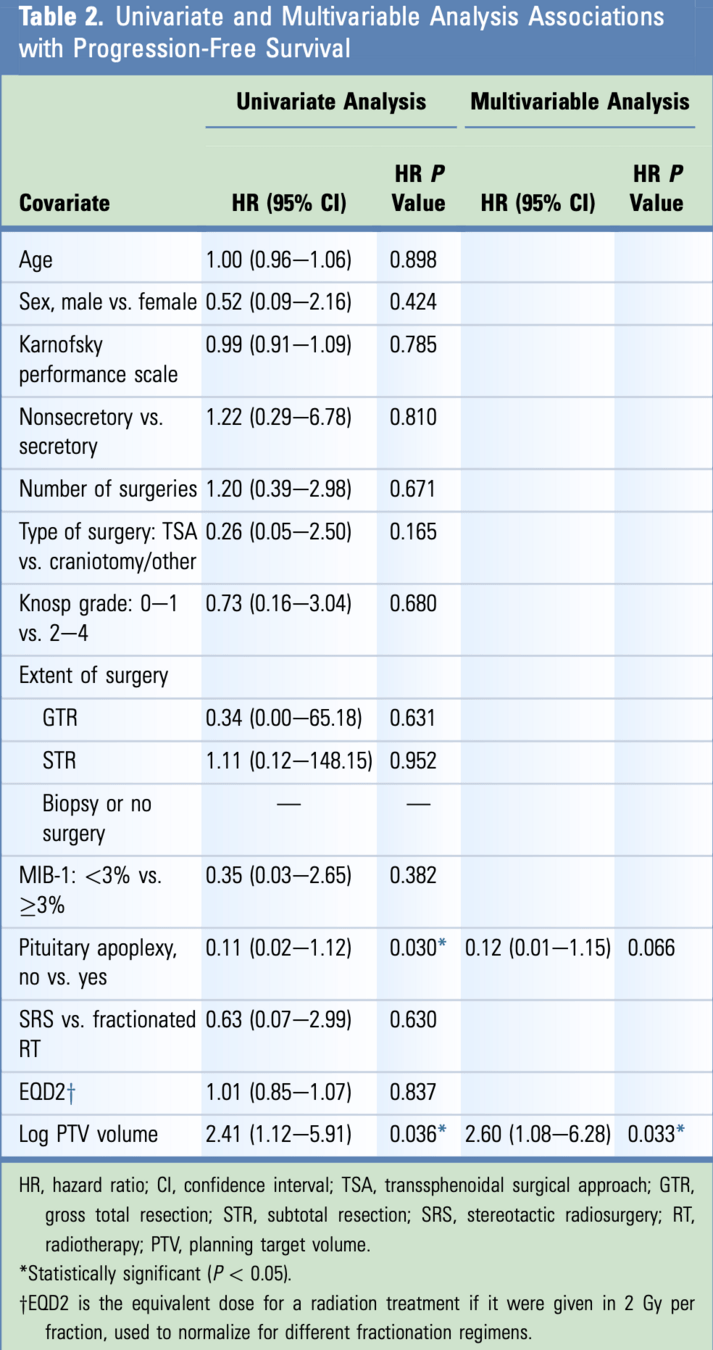
- Factors associated with worse PFS on univariate analysis:
- Larger planning target volume (HR 2.41, p=0.036)
- Pituitary apoplexy (HR 0.11, p=0.03)
- On multivariable analysis, only larger PTV remained significant:
- HR 2.60, 95% CI 1.08-6.28, p=0.033
- Factors associated with better hormonal control:
- Higher dose to tumor (HR 1.05, 95% CI 1.02-1.09, p=0.005)
- More surgeries (HR 1.74, 95% CI 1.05-2.89, p=0.032)
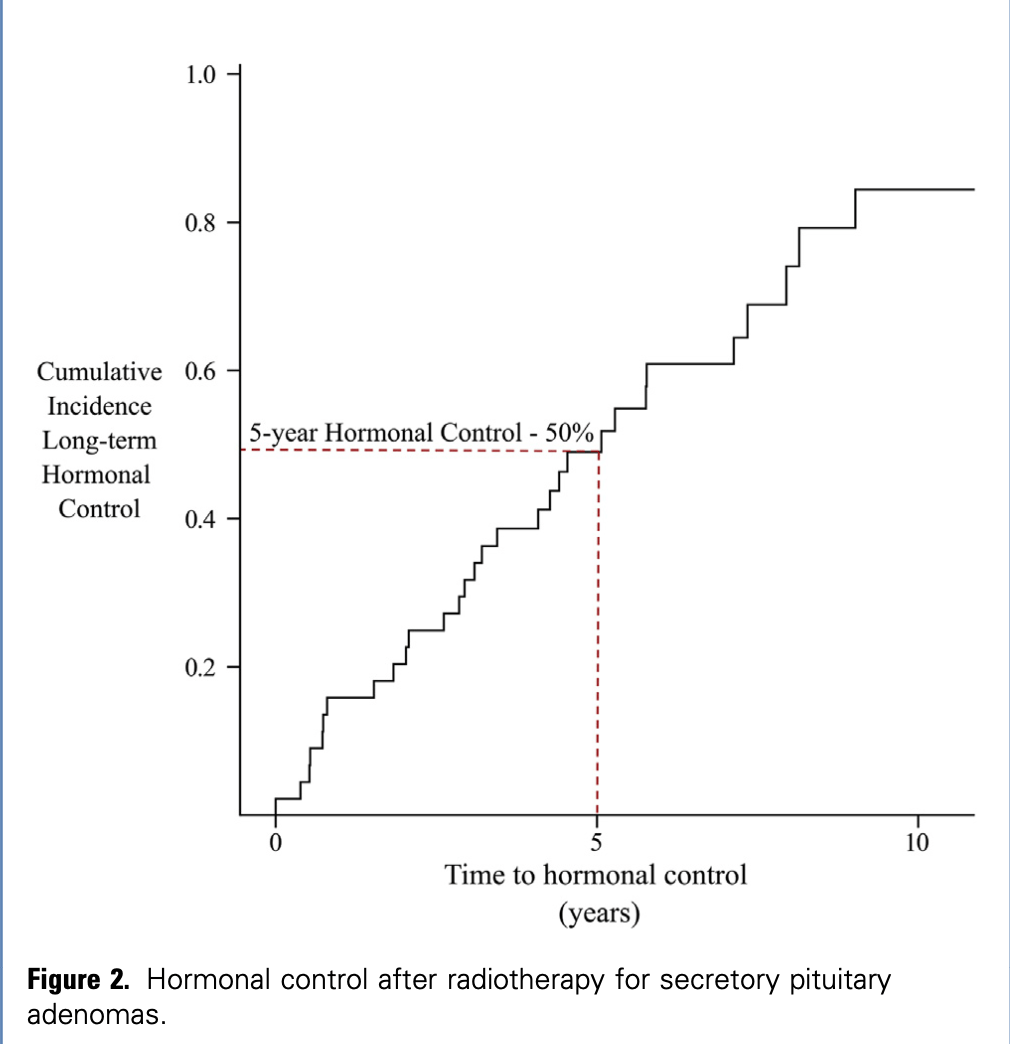
Hormonal Control
- For secretory tumors, hormonal control at 5 years: 50.0%
- Factors associated with improved hormonal control:
- Higher 2-Gy equivalent dose to tumor (HR 1.05, 95% CI 1.02-1.09, p<0.01)
- Number of surgeries (HR 1.74, 95% CI 1.05-2.89, p=0.03)
- No association with:
- Age, sex, gross tumor volume
- MIB-1 index, Knosp grade
- Use of SRS vs fractionated RT
- Similar time to hormonal control with SRS (mean 3.23 years) vs fractionated RT (mean 3.82 years, p=0.55)
Secondary outcome: Toxicity and side effects
Factors associated with increased hormonal deficiency:
- Increasing number of surgeries (HR 0.41, 95% CI 0.13-0.69, P < 0.01)
- No significant association with:
- Secretory status of tumor
- Size of planning target volume
- Age at diagnosis
Other Toxicities
- Low rates of non-endocrine toxicities:
- Transient diabetes insipidus: 16 patients (postoperative)
- Unilateral muffled hearing: 3 patients (lasting 2-5 months)
- No reported cases of:
- Radiation necrosis
- Optic neuropathy
- Other significant neurological complications
- No reported grade 3-4 acute toxicities
Conclusions
- Modern LINAC-based RT provided excellent long-term outcomes:
- 5-year local control: >94% for both secretory and nonsecretory tumors
- No significant difference in LC between functional and nonfunctional tumors
- 50% hormonal control at 5 years for secretory tumors
- Contrary to prior reports, no difference in LC between secretory and nonsecretory tumors
- Likely due to:
- Higher total doses
- More conformal radiation (IMRT, VMAT)
- Daily image guidance
- Primary toxicity was hypopituitarism, but many deficits present before RT
Strengths
- Large single-institution cohort (140 patients)
- Long follow-up (median 5.35 years)
- Includes modern RT techniques:
- Intensity-modulated RT (51.4%)
- Volumetric modulated arc therapy (39.3%)
- Dynamic conformal arcs (9.3%)
- Both secretory and nonsecretory tumors included
- Consistent use of daily image guidance
- Detailed assessment of both local control and hormonal control
- Analysis of hypopituitarism before and after RT
Limitations
- Retrospective study design
- Heterogeneous patient population
- Selection bias for treatment modality (not randomized)
- Limited number of progression events (only 3 local failures)
- MIB-1 proliferation index not available for many patients (65%)
- No standardized protocols for::
- Timing of surgery and radiation
- Type of RT (SRS vs fractionated)
- Medical management of secretory tumors
- No data on newer hypofractionated approaches (e.g., 5 fraction SRS)