Radiation Therapy for Localized MALT Lymphoma: Long-Term Outcomes
Fang et al. International Journal of Radiation Oncology • Biology • Physics, 2021
Introduction
- MALT lymphoma: indolent neoplasm, 7-8% of B-cell non-Hodgkin lymphomas
- Early-stage disease has favorable prognosis
- Radiation therapy (RT) can achieve long-term disease control
- Limited prospective data on long-term outcomes and toxicities
- Study objective: determine efficacy, safety, and salvage outcomes of RT alone for localized MALT lymphoma
Methods
- Single-center, prospective trial
- Eligibility: stage I, II, or IV (due to bilateral involvement) MALT lymphoma
- Treatment: involved field RT, 24-39.6 Gy
- Primary endpoint: relapse-free survival (RFS)
- Secondary endpoints: progression-free survival (PFS), overall survival (OS), toxicity
- Preplanned subgroup analyses by site of involvement
Patient Population
- 75 patients accrued (2000-2012),
- 73 received protocol-specified RT
- Median age: 57 years (range 25-84)
- Stage: I (84%), II (13%), IV (3%)
- Sites: gastric (47%), orbit (23%), head and neck non-orbit (18%), skin (5%), other (7%)
- 13/34 gastric MALT patients H. pylori positive at diagnosis
- Median follow-up: 9.8 years
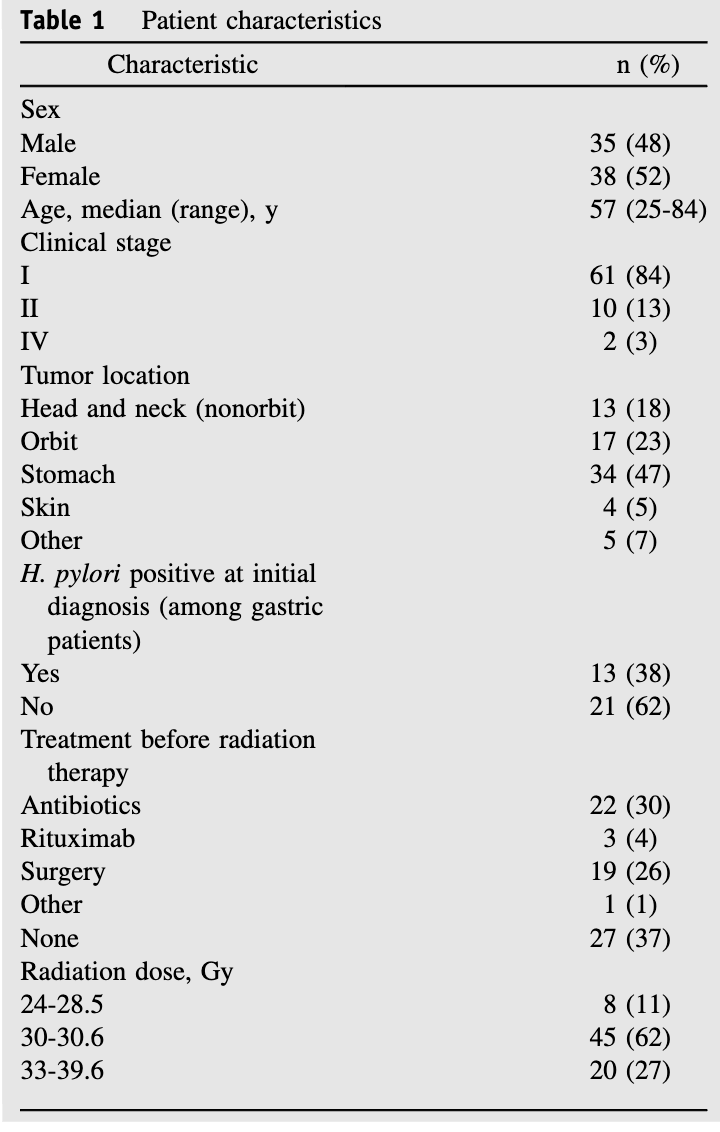
Radiation Protocol
- Involved field RT: 24-30.6 Gy in 1.8-2 Gy per fraction
- Boost to tumors >5 cm allowed up to 39.6 Gy
- CT-based planning required (except cutaneous MALT)
- Gastric MALT: empty stomach, entire stomach treated with 2 cm margin
- Dose distribution:
- 24-28.5 Gy (11%)
- 30-30.6 Gy (62%)
- 33-39.6 Gy (27%)
- All treatment plans peer-reviewed before start of RT
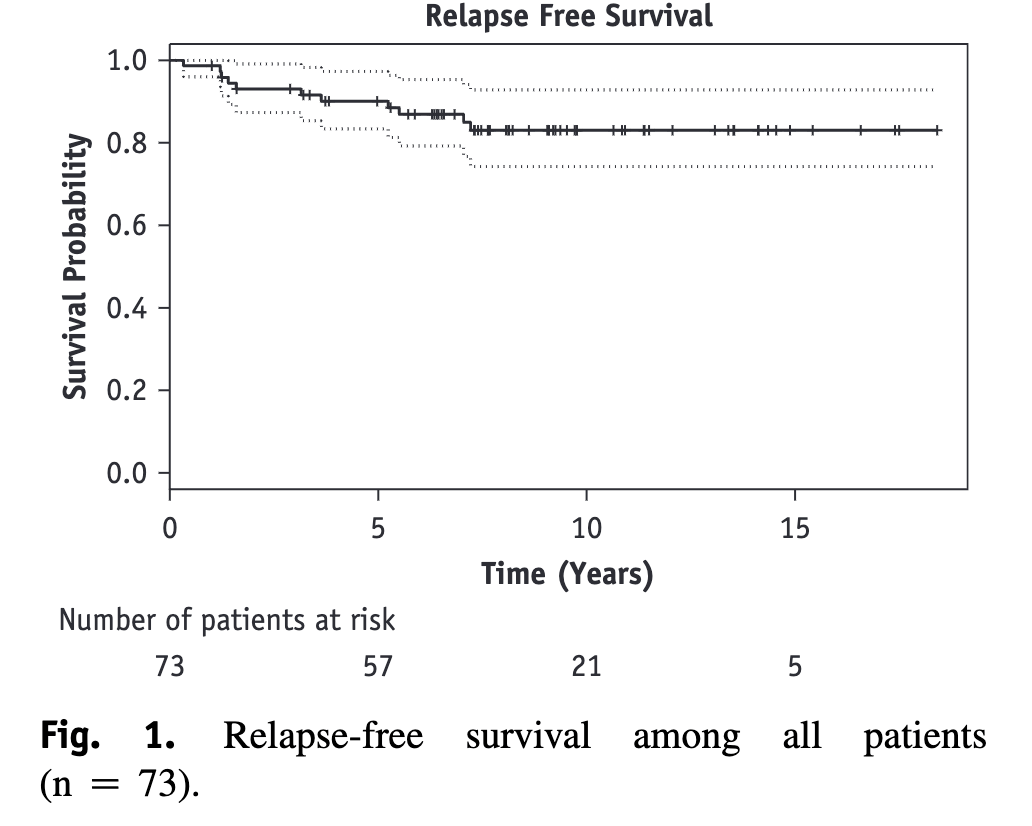
Primary Outcome
- All patients achieved complete response (median time: 3 months)
- 11 patients (15%) relapsed (median time to progression: 38.3 months)
- 10-year relapse-free survival: 83% (95% CI: 74%-93%)
- Median RFS: not reached
- No significant difference in RFS by disease site (p=0.17)
Primary Outcome
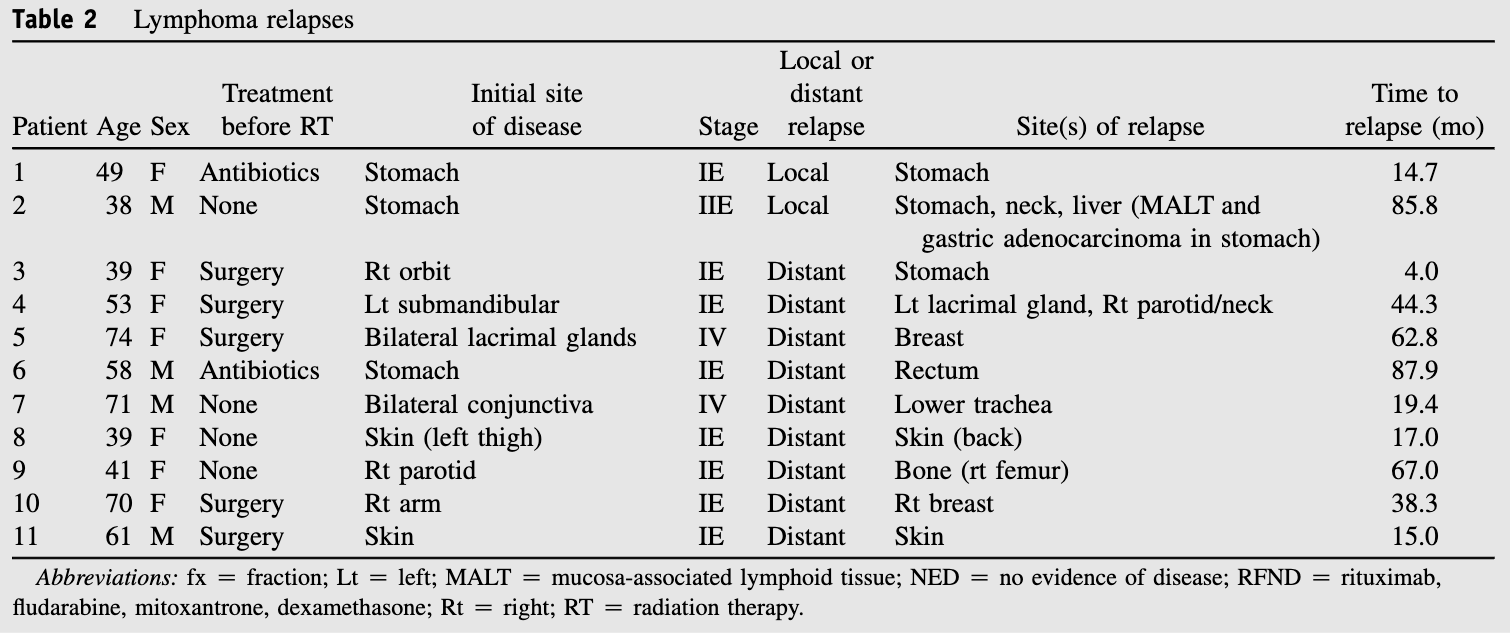
Secondary Outcomes
- Median PFS: 17.5 years (95% CI: 11.5 years to N/A)
- 10-year PFS: 71% (95% CI: 60%-84%)
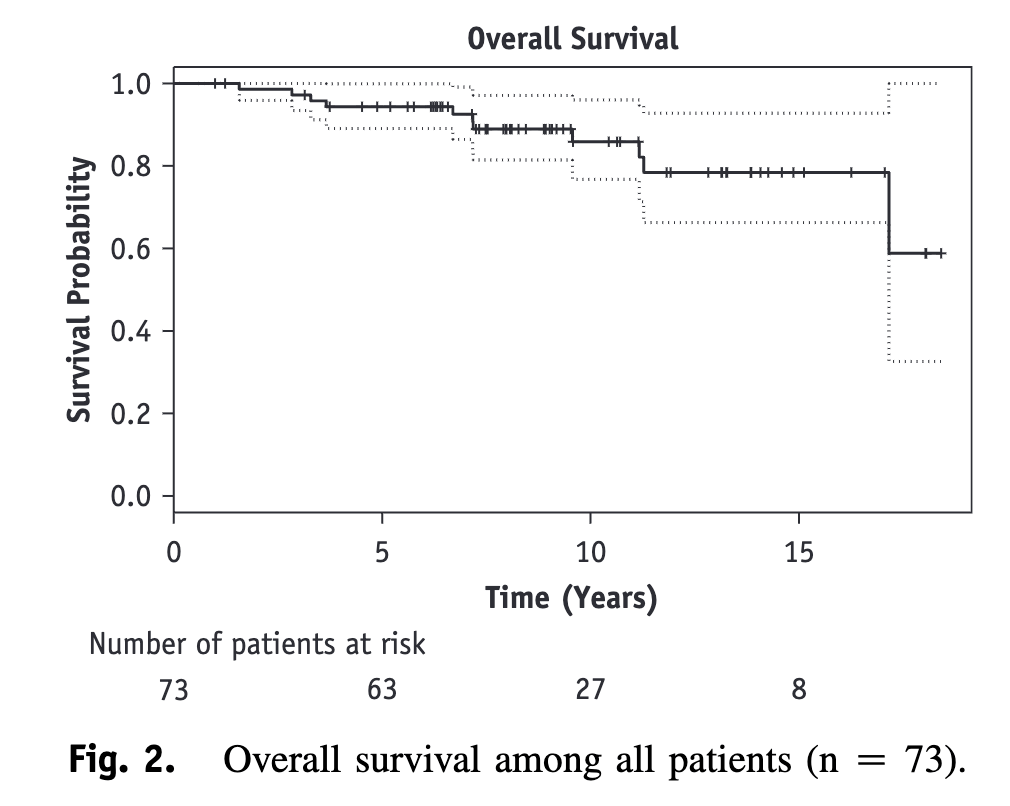
- 10-year OS: 86% (95% CI: 77%-96%)
- No significant difference in PFS or OS by disease site
- All relapses successfully salvaged
- No disease transformation to aggressive lymphoma
- One patient (1%) developed secondary malignancy (gastric adenocarcinoma)
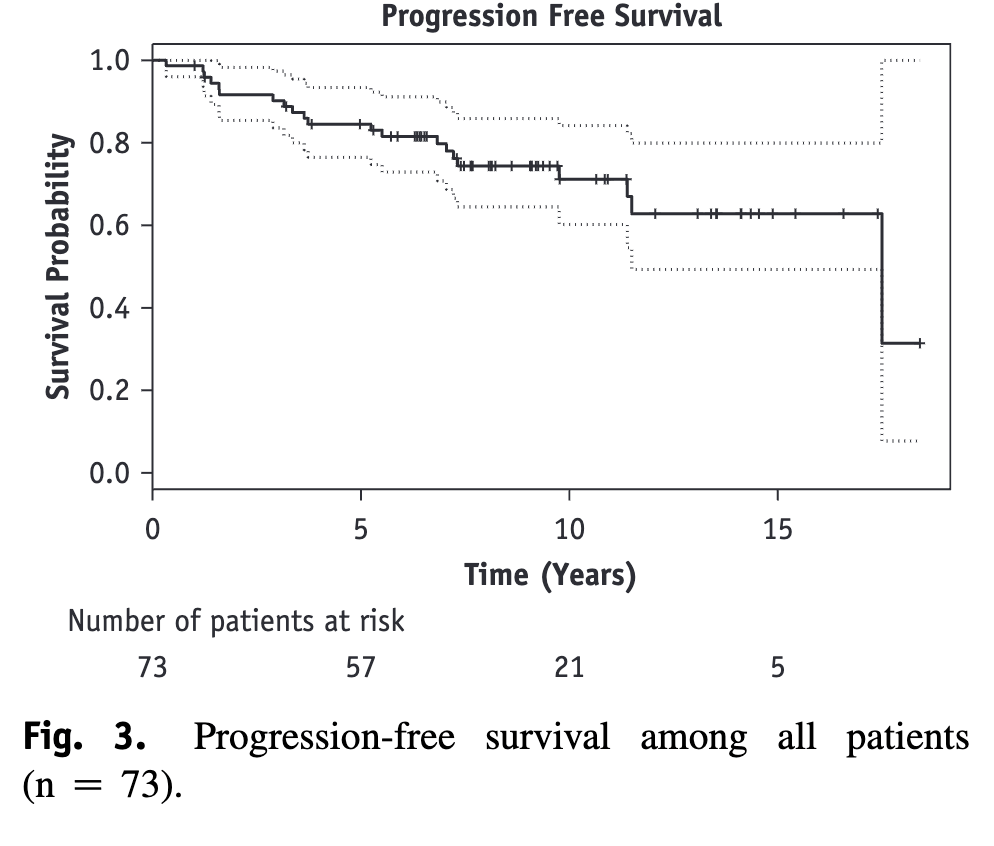
Secondary Outcomes
- Median PFS: 17.5 years (95% CI: 11.5 years to N/A)
- 10-year PFS: 71% (95% CI: 60%-84%)
- 10-year OS: 86% (95% CI: 77%-96%)
- No significant difference in PFS or OS by disease site
- All relapses successfully salvaged
- No disease transformation to aggressive lymphoma
- One patient (1%) developed secondary malignancy (gastric adenocarcinoma)
Toxicity
- Acute toxicity: 92% of patients, mostly grade 1-2
- Most common acute toxicities: nausea (38%), dermatitis (33%), fatigue (18%), eye symptoms (18%)
- One grade 3 acute toxicity: retinal detachment
- Late toxicity: 30% of patients, mostly grade 1-2
- Most common late toxicities: cataracts (8%), dry eye (7%), xerostomia (10%)
- One grade 3 late toxicity: severe retinopathy (same patient as acute toxicity)
Conclusions
- RT for localized MALT lymphoma provides excellent long-term disease control
- High complete response rate (100%) with durable remissions
- Low rate of relapse (15%) with successful salvage treatment
- No disease-specific deaths observed
- Acceptable toxicity profile, mostly low-grade
- Results affirm the use of RT as definitive treatment in early-stage MALT lymphoma
- Further studies on dose de-escalation may help minimize toxicity
Strengths and Limitations
- Strengths:
- Prospective design
- Long-term follow-up (median 9.8 years)
- Comprehensive reporting of outcomes and toxicities - Limitations:
- Single-center study
- Higher radiation doses than current standards
- Use of involved field RT vs. current involved site RT
- Limited use of PET staging (60% of patients)
- Lack of data on t(11;18) translocation status
Discussion Points
- How might the results of this study impact current practice for early-stage MALT lymphoma?
- What are the potential benefits and risks of dose de-escalation in RT for MALT lymphoma?
- How does the toxicity profile observed in this study compare to more modern RT techniques and doses?
- What role does PET staging play in the management of MALT lymphoma, and how might it have affected the results of this study?
- How should we approach the management of relapsed MALT lymphoma after initial RT, given the excellent salvage outcomes observed in this study?