Shunt lesions
Shunt Lesions: Objectives
- Identify types of shunts
- Identify clinical features
- Diagnosis of shunts (including echo features)
- Qualification and management of shunts
- Who, when and how to treat
What is a shunt?
Right-to-Left shunts
- Blood from systemic arterial circulation mixes with venous blood
Where is the shunt
| Level of L to R shunt | Increased SaO2 (step-up) | Example |
|---|---|---|
| Screening | PA SaO2- SVC SaO2 >8% | Shunt somewhere between SVC and PA |
| Atrial | RA SaO2 - mixed venous SaO2 >7% | ASD |
| Ventricular | RV SaO2 - RA SaO2 >5% | VSD |
| Pulmonary | PA SaO2 - RV SaO2 >5% | PDA |
Laflamme, D., 2018. Cardiology: A Practical Handbook. CRC Press.
Calculating the shunt fraction
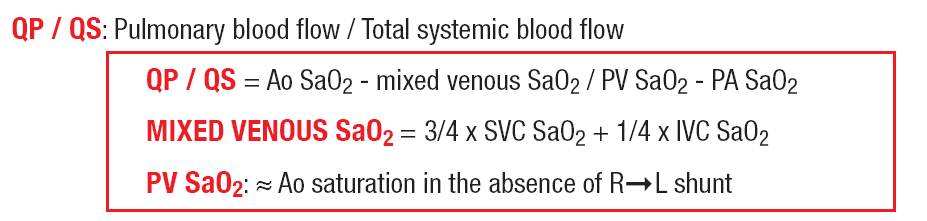
Laflamme, D., 2018. Cardiology: A Practical Handbook. CRC Press.
Is the shunt important?
| Qp/Qs < 1.5 | Qp/Qs 1.5-2 | Qp/Qs > 2 |
|---|---|---|
| Small L-to-R shunt |
Moderate L-to-R shunt |
Large L-to-R shunt |
Atrial Septal Defect
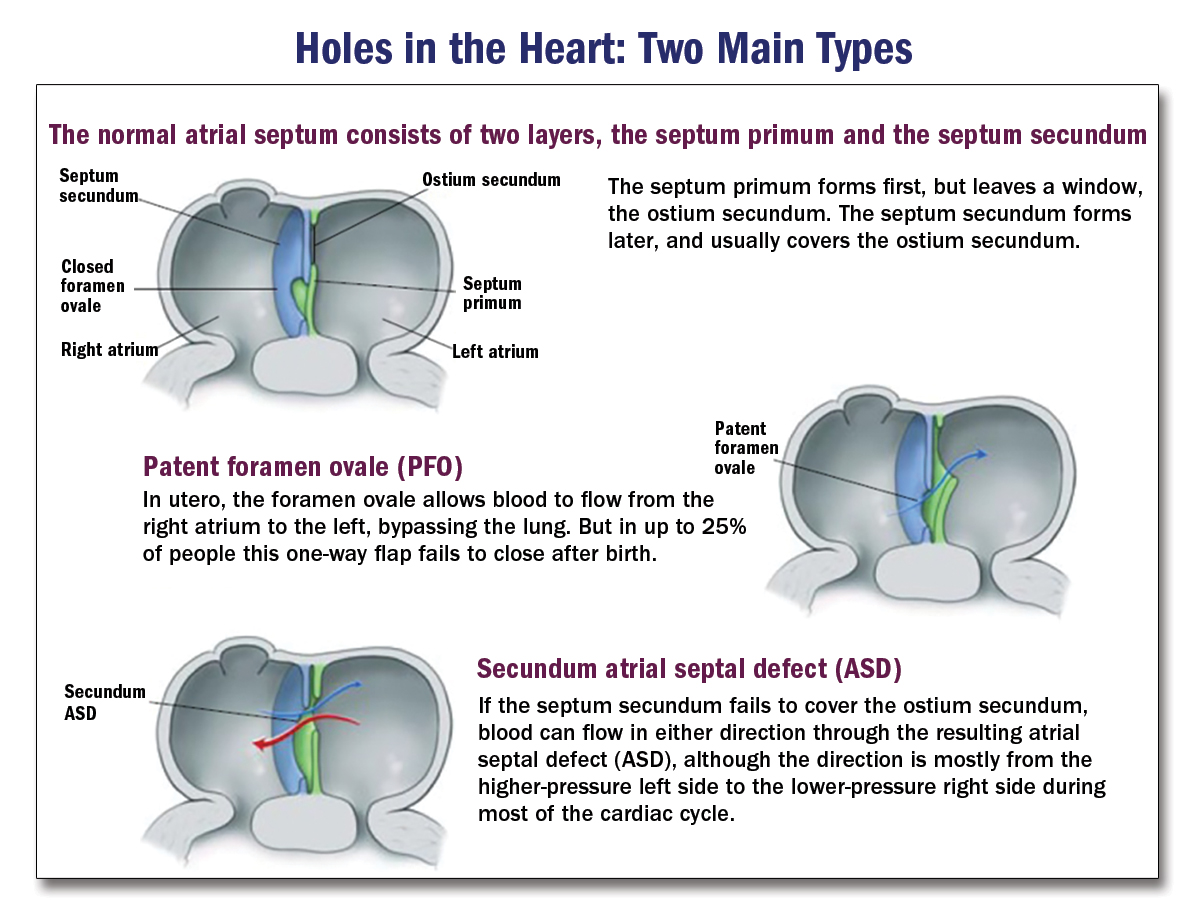
ACCSAP, Simple shunts, R. Krasuski
Types of atrial septal defects
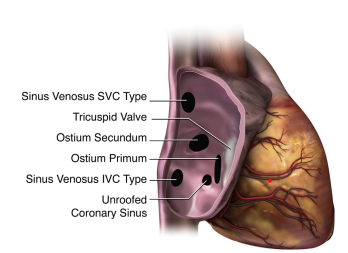
Silvestry, et al 2015. Journal of the American Society of Echocardiography, 28(8), pp.910-958.
ASD
- 15% of congenital abnormalities
- Ostium Secundum is 75% of all ASD abnormalities
- 10% of patients have >1 defect in the atrial septum
- 1/3 of patients have associated defects
- eg: partial anomalous pulmonary venous drainage, coarctation of the aorta, subaortic stenosis, VSD, pulmonary stenosis
ASD: When to suspect
- Systolic murmur at LSB with fixed S2 split,
- Unexplained RV overload
- Atrial arrhythmia
- Pulmonary HTN
ASD: Clinical features
- Adult patients often present ~40 yo
- Symptoms: fatigue, palpitations, breathlessness
- Physical: fixed split-second heart sound, pulmonic flow murmur
- +/- signs of pulmonary hypertension
- +/- signs of Eisenmenger syndrome
- ECG: RBB, R-axis deviation, abnormal p-wave axis
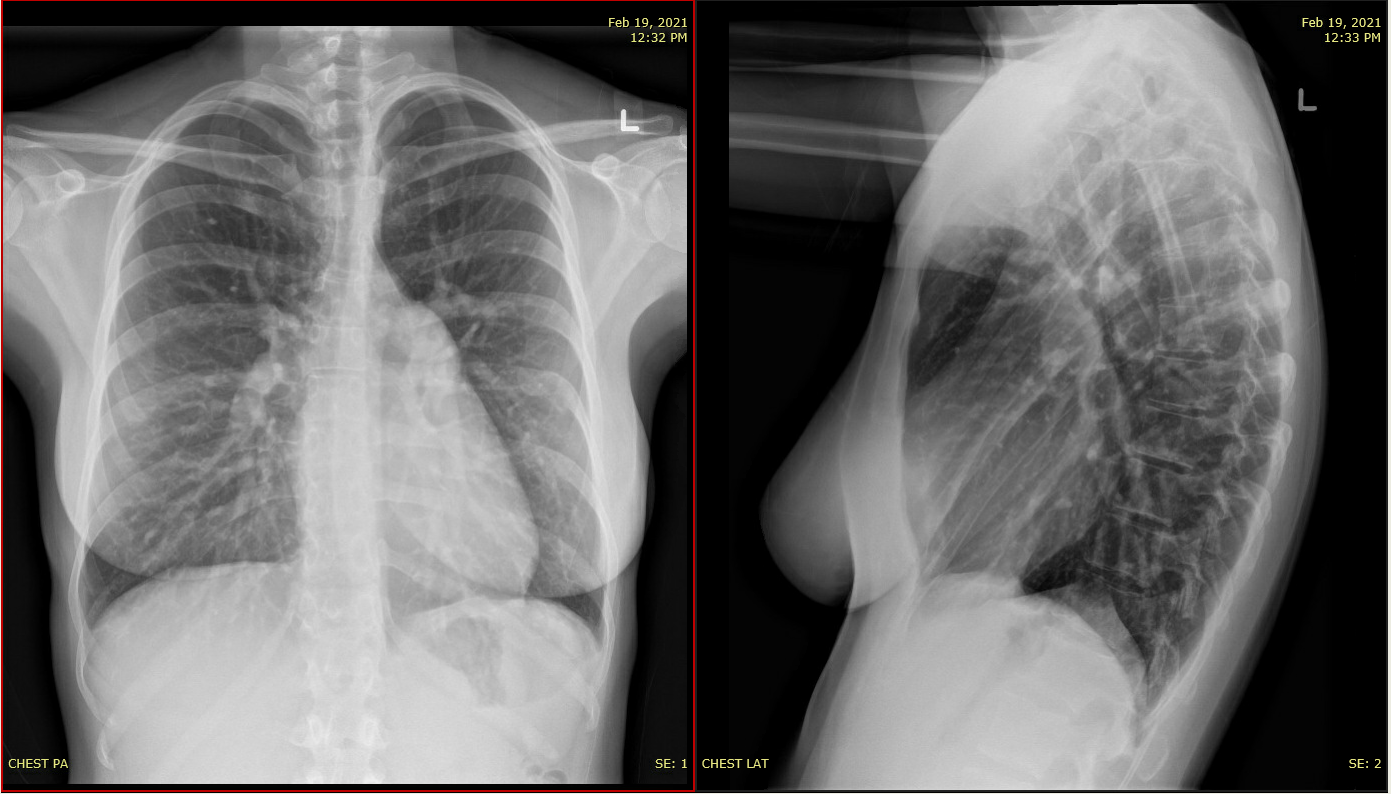
- CXR: Prominent PA, RA, RV, pulmonary plethora
ACCSAP, Simple shunts, R. Krasuski
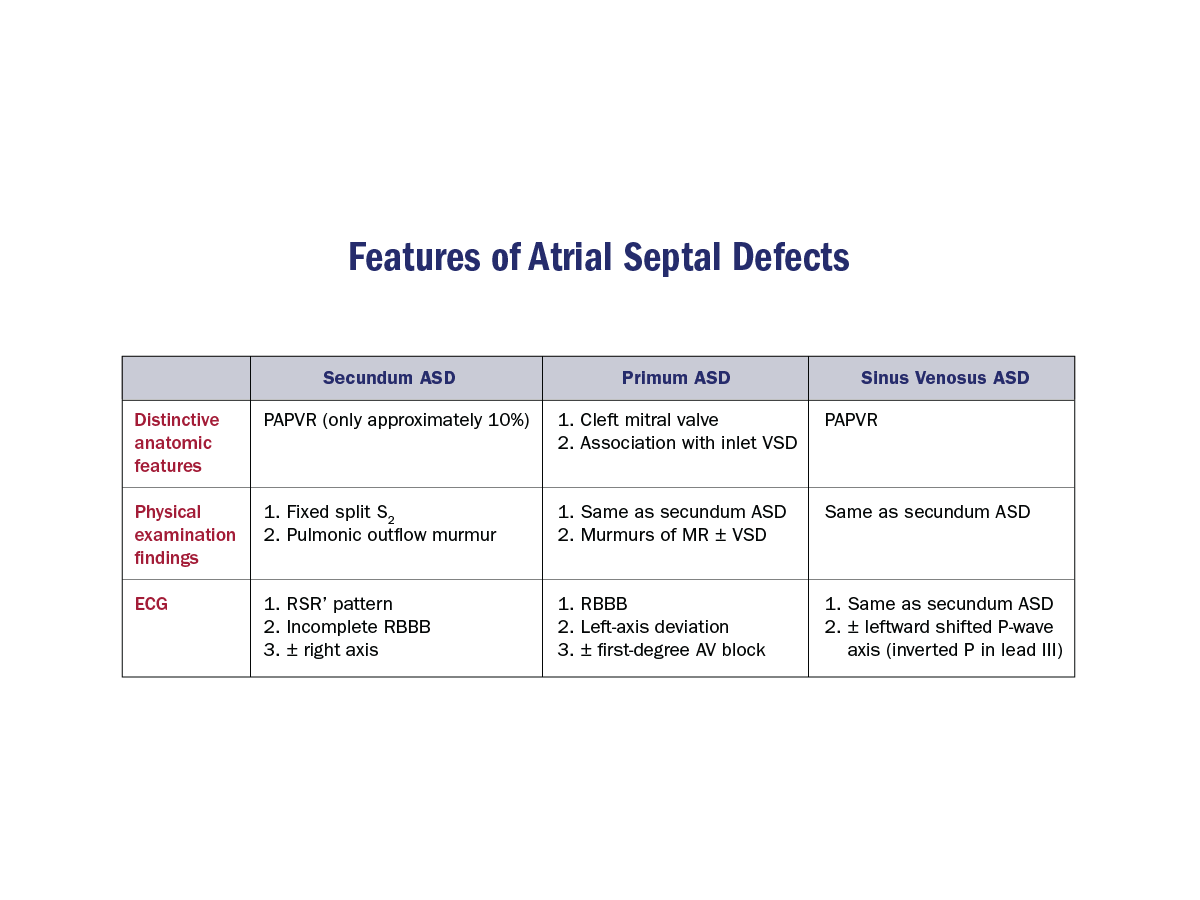
Secundum ASD
- Normal or slightly elevated JVP
- RV heave
- Ejection systolic murmur PA
- Fixed split 2nd heart sound
- Tricuspid diastolic flow rumble
Associated findings: Secundum ASD
ECG: Typical RBB

Notched R-waves in inferior leads: "Crochetage"
Incomplete RBB in V1
Associated findings: Secundum ASD
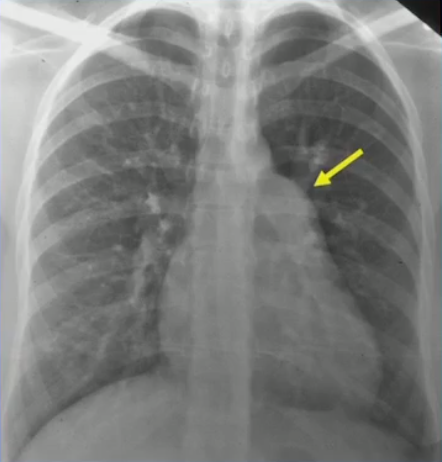
Prominant PA
Pulmonary plethora
Assessing ASD

2018 AHA/ACC ACHD Guideline
ASD: Role of echo
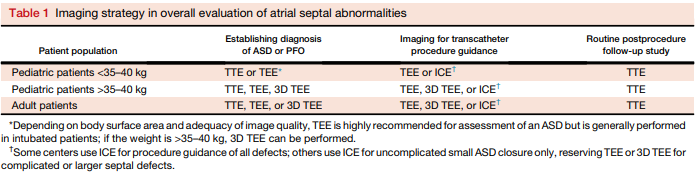
Journal of the American Society of Echocardiography Volume 28 Number 8
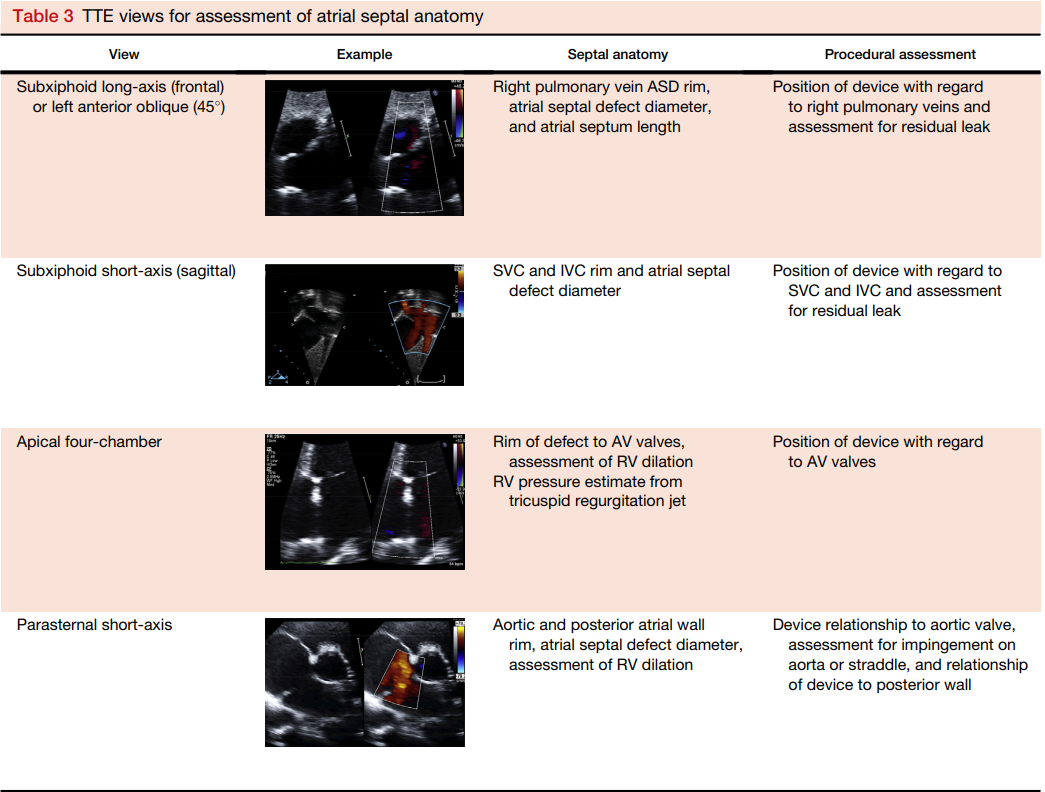
Journal of the American Society of Echocardiography (2015) Volume 28 Number 8
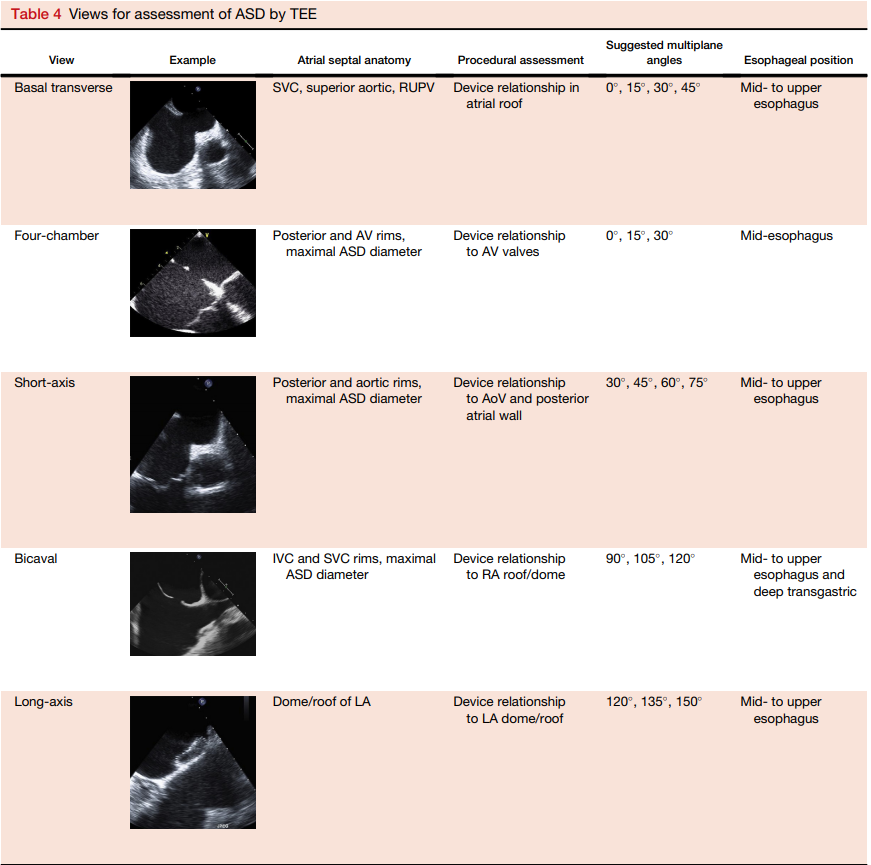
Journal of the American Society of Echocardiography (2015) Volume 28 Number 8
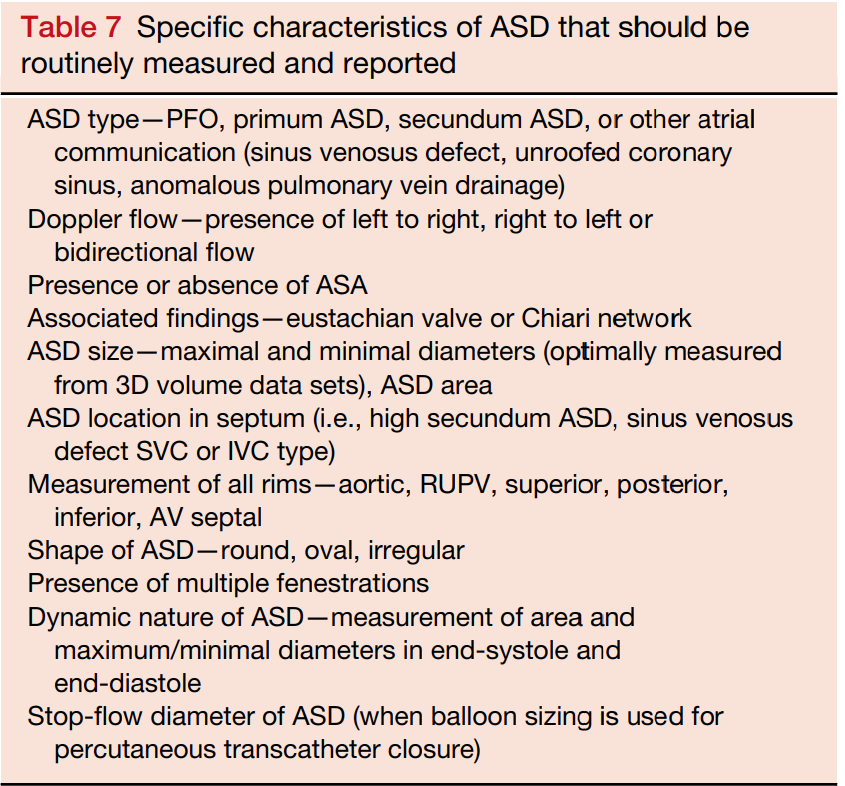
Journal of the American Society of Echocardiography (2015) Volume 28 Number 8
ASD: Cardiac imaging
- CT or MR cross-sectional imaging best for viewing pulmonary venous connections
- Especially: innominate vein or vertical vein
- CT and CMR can provide a shunt estimate
ASD: Estimation of Qp:Qs
- Can be estimated by CMR
- Limited reliability by TTE or TEE
- Cardiac cath- direct measurement
ASD: Role of cardiac catheterization
- Performed at the time of closure
- Diagnostic catheterization IF necessary to determine detailed hemodynamics (e.g. in the case of discrepant non-invasive imaging)
Calculation of Qp:Qs
- indications for cath
- Inconclusive left-to-right shunt severity by noninvasive means
- Significant pHTN is suspected
- PASP >50% systemic SAP or PVR > 1/3 of SVR and no cyanosis at rest or during exercise
- Assess LV diastolic function
- Device close of secundum ASD
- In older adults: Rule out left atrial hypertension secondary to diastolic dysfunction
- Could have a similar presentation to ASD but have poor outcomes after ASD closure
Shunt run by cath
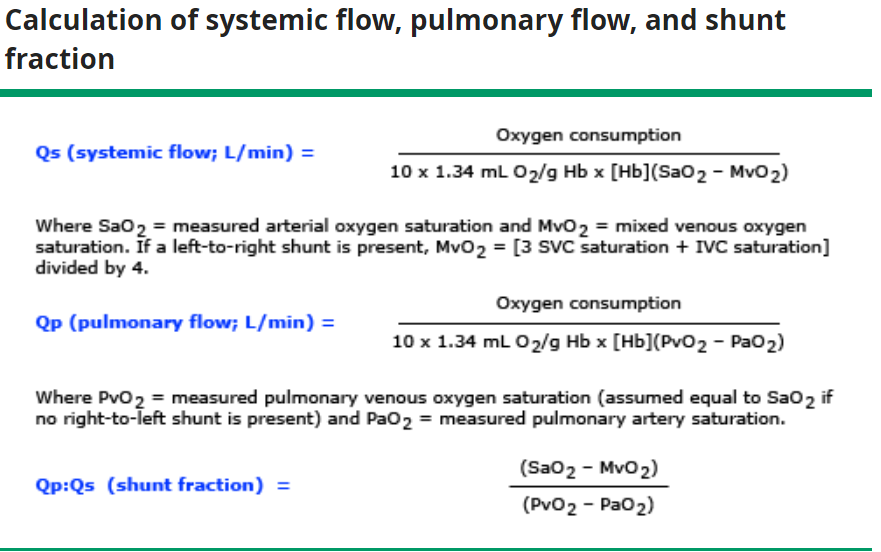
© 2021 UpToDate, Inc.
Note American values - in Canada no need to divide by 10
ASD: Should all be closed?
- In patients with normal functional capacity: closure benefits are unclear
- Patients who do not undergo closure have worse long-term outcomes:
- Atrial arrhythmias
- Reduced functional capacity
- Greater instances and degree of PAH
ASD: Who should have closure
- Patients with reduced functional capacity caused by important Secundum ASD
- moderate-large left-to-right shunt
- evidence of right heart volume overload
- in the absence of PAH
- History of paradoxical embolism
ASD: Who to close

2018 AHA/ACC ACHD Guideline
ASD - Therapy
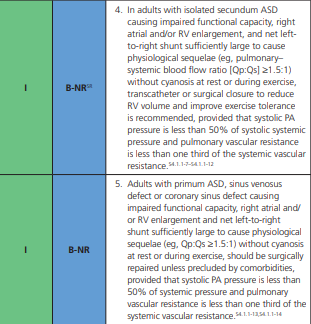
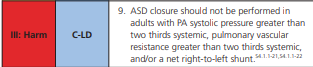
2018 AHA/ACC ACHD Guideline
ASD: Who to close
2020 ESC ACHD Guideline

Journal of the American Society of Echocardiography (2015) Volume 28 Number 8
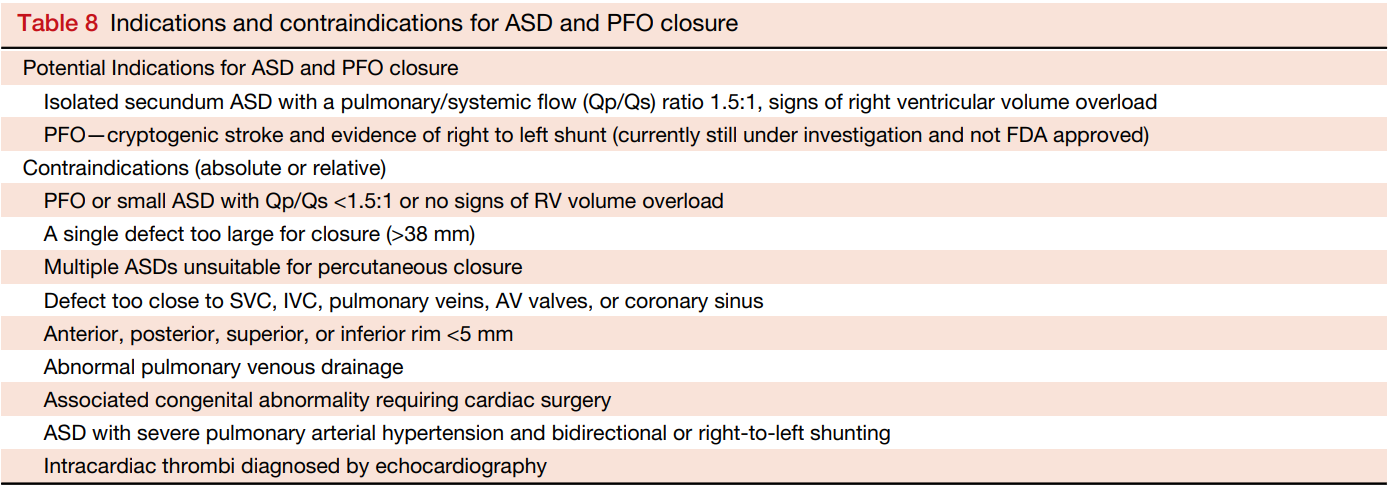
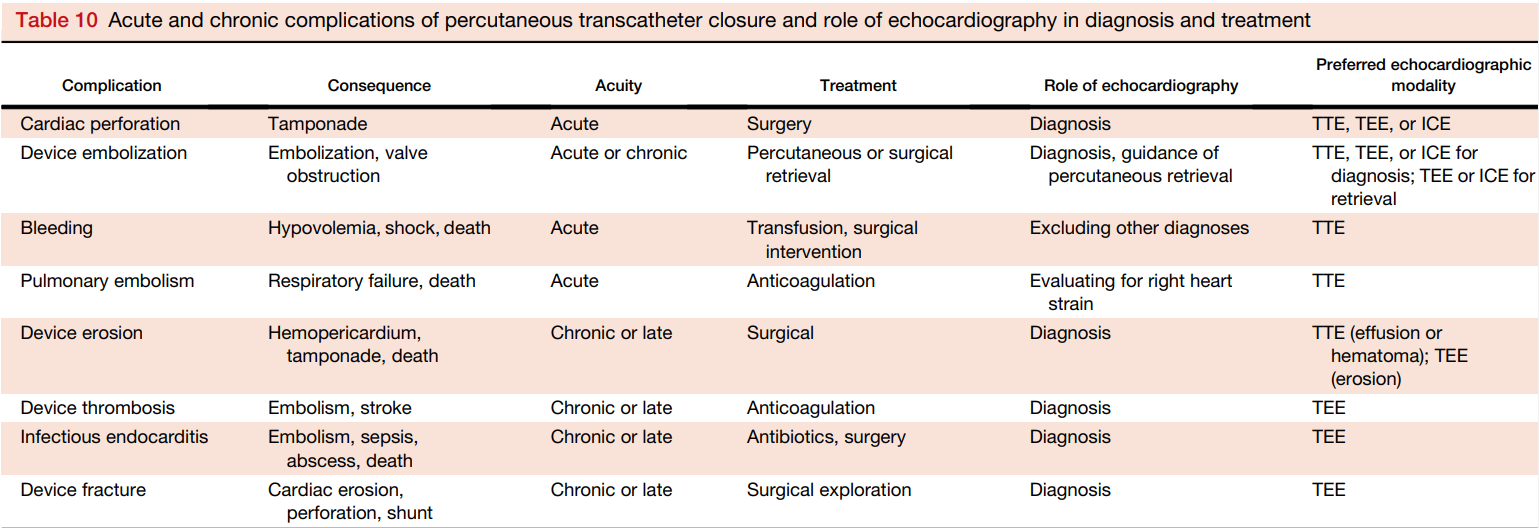
Indications and contraindications for percutaneous ASD and PFO closure
Journal of the American Society of Echocardiography (2015) Volume 28 Number 8
ASD Case
- 29 yo F with lifelong palpitations and new shortness of breath on exertion - specifically with stairs and with vigorous activity
- Physical exam: RV heave, S1, S2 split, soft murmur over left sternal border. No signs of heart failure
ASD Case
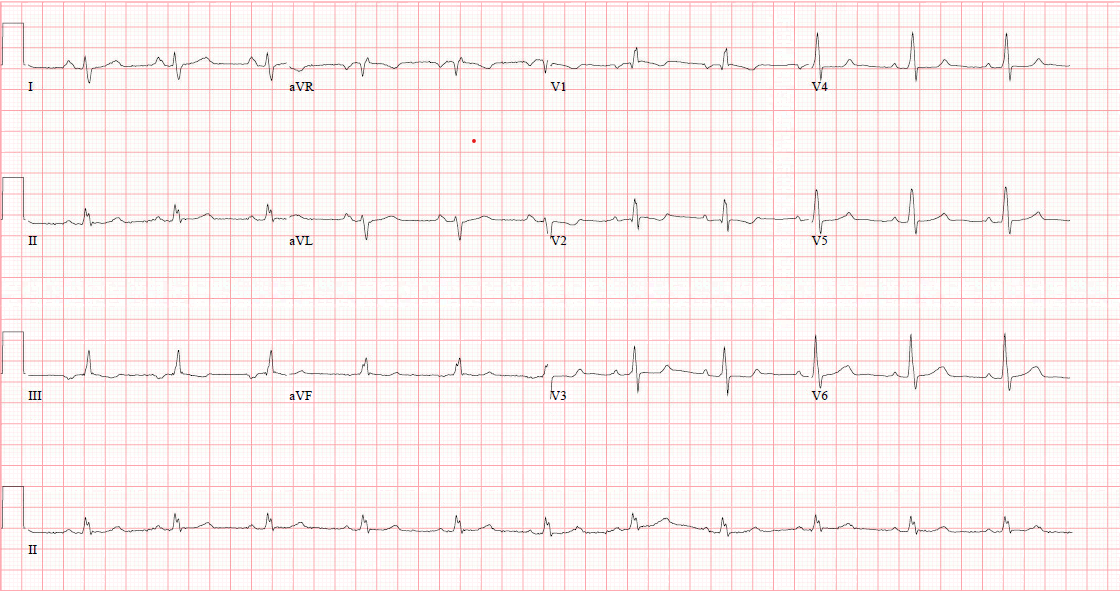
ASD Case
ASD Case
ASD Case
Hemodynamic data
(mmHg)
Oxygen saturations (%)
Right atrium 2
Right ventricle 28/3
Pulmonary artery 26/6, mean 14
Pulmonary wedge mean 4
Left atrium 4
Blood pressure (via cuff) 111/67
SVC 68.7
RA 84.7
IVC 73.4
Mixed venous 69.5
Left atrium 94.6
Pulmonary vein 93.8
Systemic 96
RV 86.9
Pulmonary artery 86.6
Hemoglobin 141 g/L
Pulmonary vascular resistance 0.6 units.
Hemodynamic data (mmHg)
Oxygen saturation
(%)
Right atrium 2
Right ventricle 28/3
Pulmonary artery 26/6, mean 14
Pulmonary wedge mean 4
Left atrium 4
Blood pressure (via cuff) 111/67
SVC 68.7
RA 84.7
IVC 73.4
Mixed venous 69.5
Left atrium 94.6
Pulmonary vein 93.8
Systemic 96
RV 86.9%
Pulmonary artery 86.6%
Hemoglobin 141 g/L
Pulmonary vascular resistance 0.6 units.
Cardiac output (Fick - systemic) 4.6 litres per minute
Cardiac output - (Fick) pulmonary 16.7 litres per minute
QP/QS 3.63:1
ASD Case
Underwent minimally invasive secundum atrial septal defect repair (4 x 3 cm autologous pericardial patch)
Ventricular Septal Defect
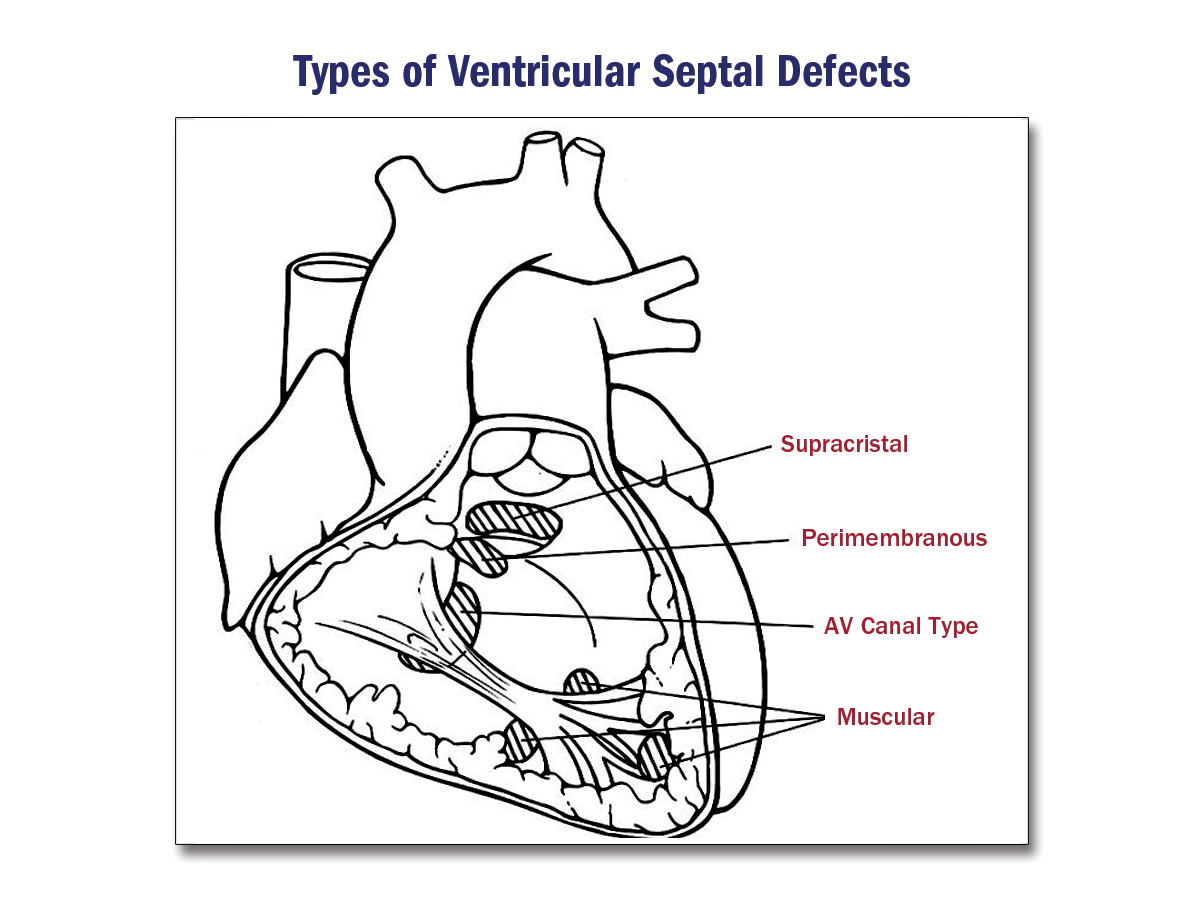
VSD
- The most common congenital defect in children
- The second most common congenital defect in adults
- Most common is perimembranous (80%) of cases
- Often isolated lesions, but can be in concert with other lesions or complexes (e.g. transposition of the great vessels, tetralogy of Fallot)
VSD: an acquired lesion
- Post MI
- Post TAVI
- Post septal myectomy
- Erosion of a strut of a bioprosthetic mitral valve
- Takuotsubo cardiomyopathy
- Trauma
ACCSAP, Simple shunts, R. Krasuski
VSD: Clinical features
- Defect size is inversely proportional to sound and severity
- Large defect (>75% of aortic annulus diameter): Eisenmenger- syndrome has no sound
- Equalization of pressure across the RV and LV
- Moderate-sized (measure 25-75% of aortic annulus diameter): mitral diastolic flow rumble
-
- Mild to moderate volume overload of pulmonary arteries, left atrium and LV
- Small restrictive defect (Qp:Qs <1.5:1): loud holosystolic along the left sternal border
- No LV volume overload or pulmonary hypertension
VSD: Prognosis
- Moderate - Large VSD: risk of progressive pulmonary vascular disease
- Further risk of pulmonary hypertension, shunt reversal and cyanosis
- HF
- Other: Arrhythmias, endocarditis, double-chambered right ventricle, thromboembolism
- Small VSD: Good prognosis, risk of endocarditis, aortic regurgiation, double chambered right ventricle
VSD investigations
- ECG - if large with pulmonary hypertension - isolated RV or biventricular hypertrophy
- CXR - if large left-to-right shunt then LA, LV enlargement and/or pulmonary edema can be noted
VSD: Echocardiographic evaluation
- Identify the location of the defect on the septum
- Establishing the number of defects
- Identifying associated features
- Assessment of size and hemodynamic significance of the defect
- Guidance treatment: interventional or surgical
Membranous VSD: Echocardiographic evaluation
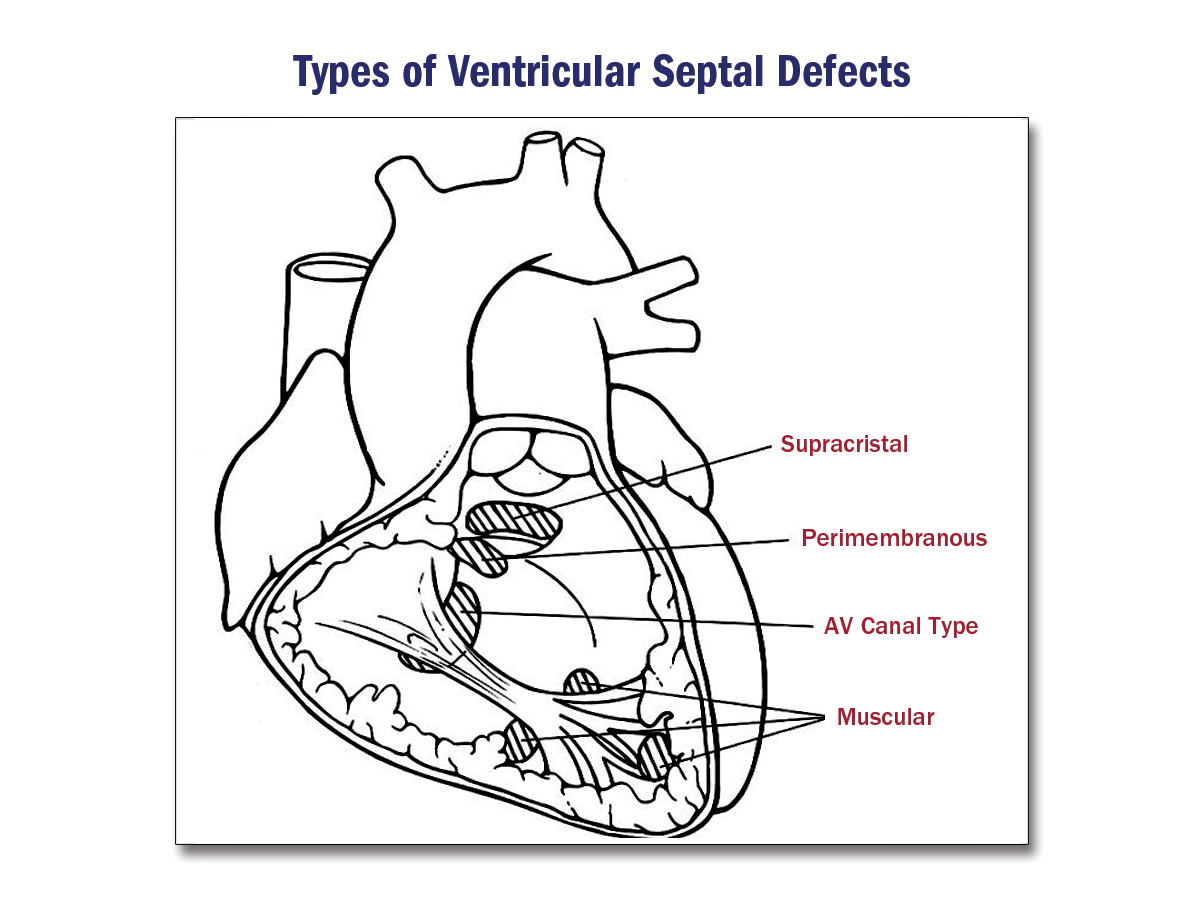
- The defect lies in the membranous septum just apical to the aortic valve and below the tricuspid valve's septal leaflet
- Parasternal long axis: seen below the aortic valve
- The orthogonal short axis of LVOT: beneath the tricuspid valve septal leaflet
- Subcostal: coronal and sagittal views
Muscular VSD: Echocardiographic evaluation
- Often multiple defects, especially post MI
- The use of colour flow is helpful across the septum
- The septum should be sweeped through in each view with colour doppler
- As the RV pressure increases, the VSD will become less apparent
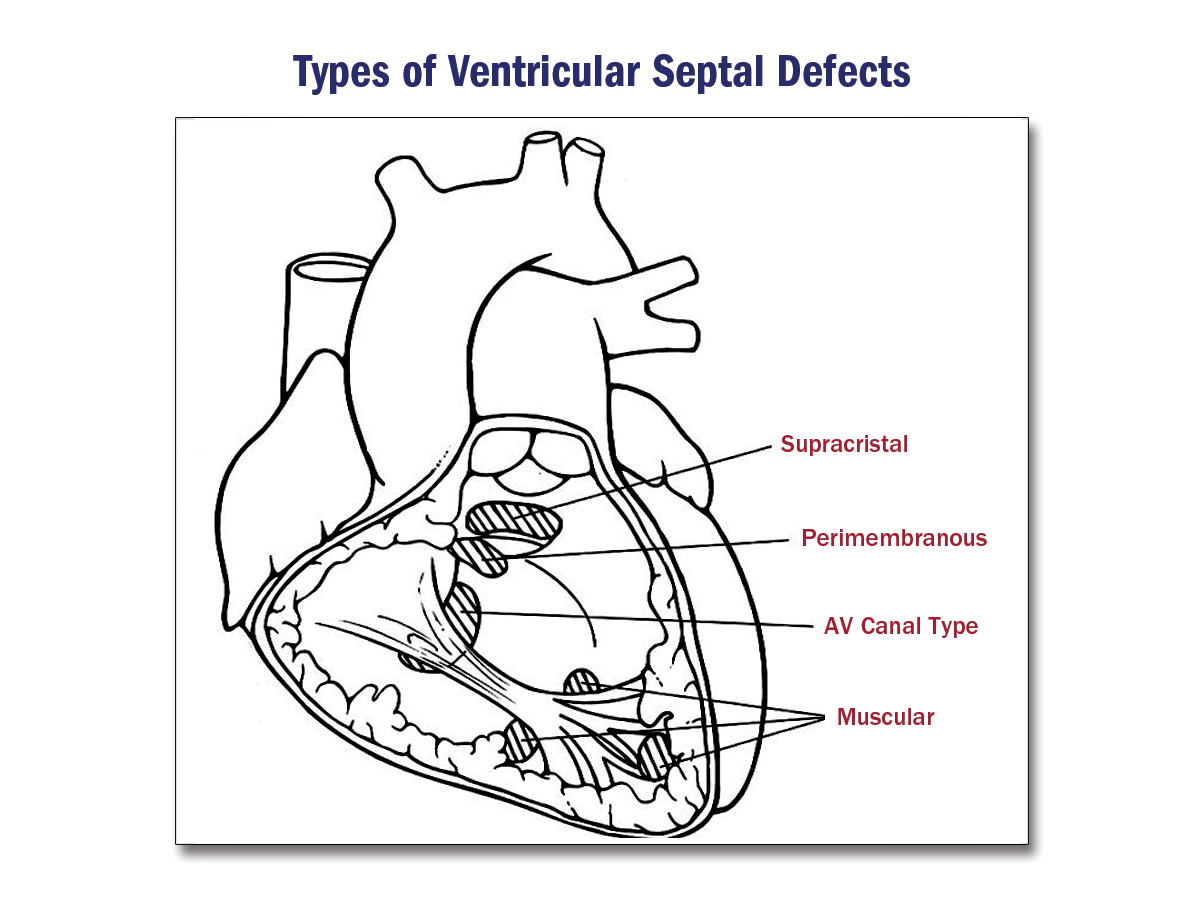
Supracristal VSD: Echocardiographic evaluation
- Located caudal to the pulmonary valve and above the crista supraventricular
- Parasternal short axis: beneath the pulmonary valve
- Parasternal and subcostal long axis and apical views: Aortic valve right coronary cusp might prolapse into the VSD
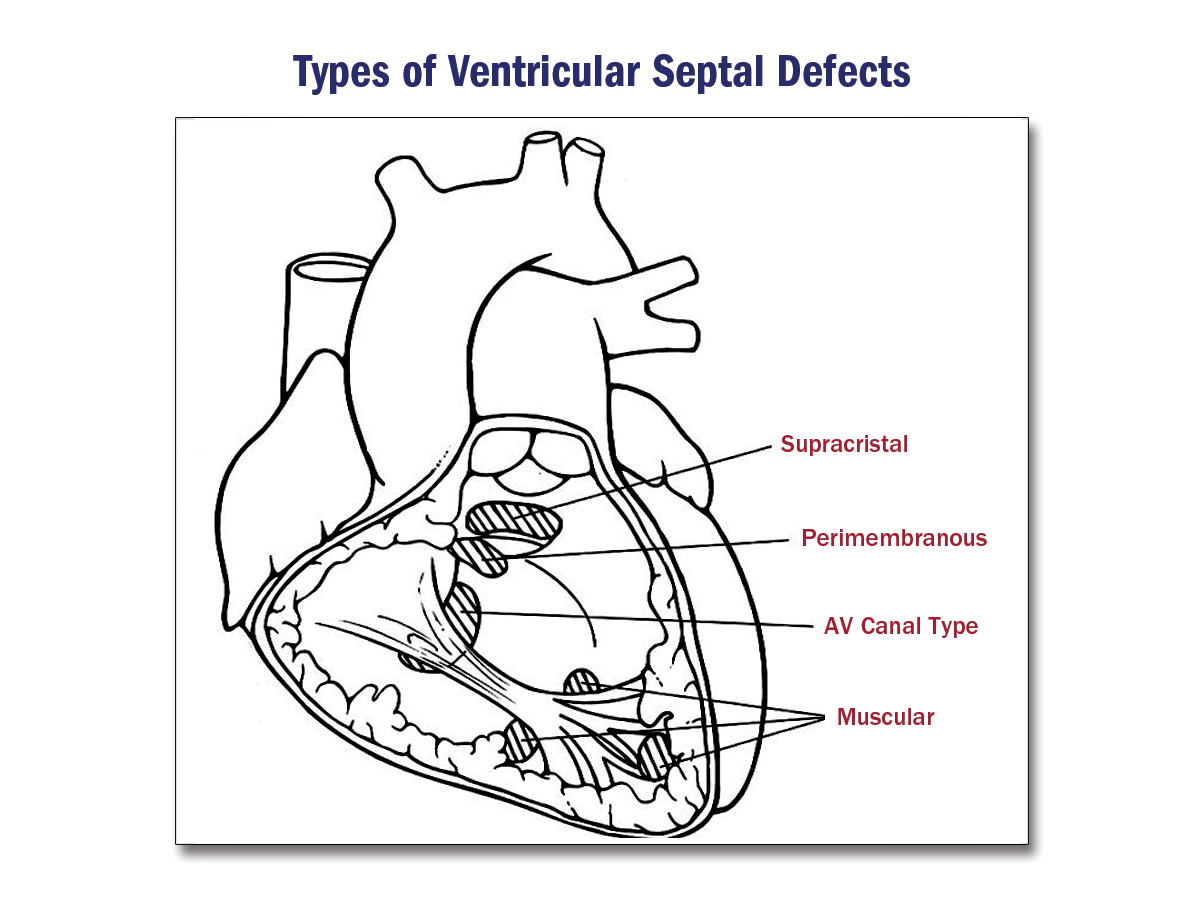
Inlet VSD: Echocardiographic evaluation
- Located at the crux of the heart, posterior and inferior to membranous and outlet defects
- Apical and subcostal views are the best to view these defects
Malalignment VSD: Echocardiographic evaluation
- This occurs when there is malalignment defects between the atrial and ventricular septa or individual parts of the septum
VSD: Echocardiographic evaluation of hemodynamics
- Measurement of RV and PA pressures are more useful than Qp/Qs
- Significant left-to-right shunting: LA and LV cavity dialate
- Increased transpulmonary and transmitral velocity by doppler
VSD: Echocardiographic evaluation of hemodynamics
- Timing of shunt:
- Normal: Left-to-right in mid and late diastole and throughout systole
- With increased pulmonary vascular disease/hypertension: Right-to-left in early and mid-diastole and late systole
VSD: Management
- VSD from infancy often close on their own
- They are often a part of a complex, e.g. transposition of the great arteries, tetralogy of Fallot
2018 AHA/ACC ACHD Guideline
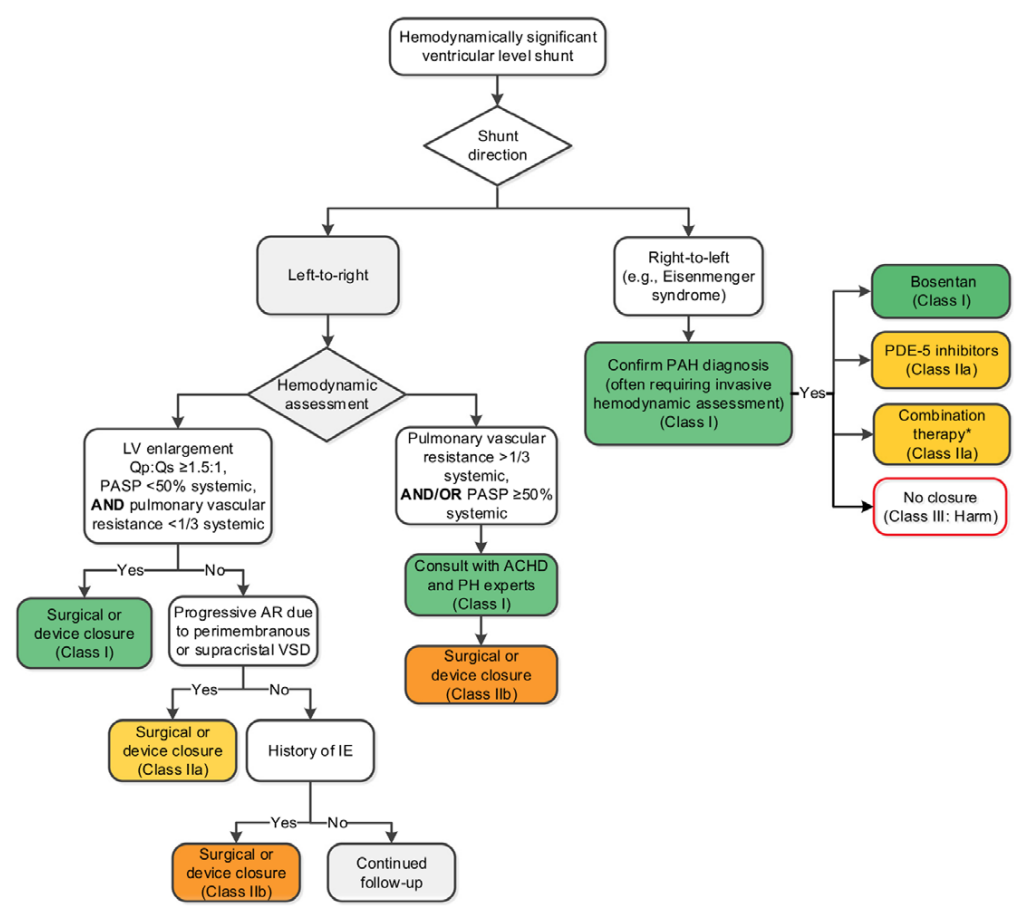
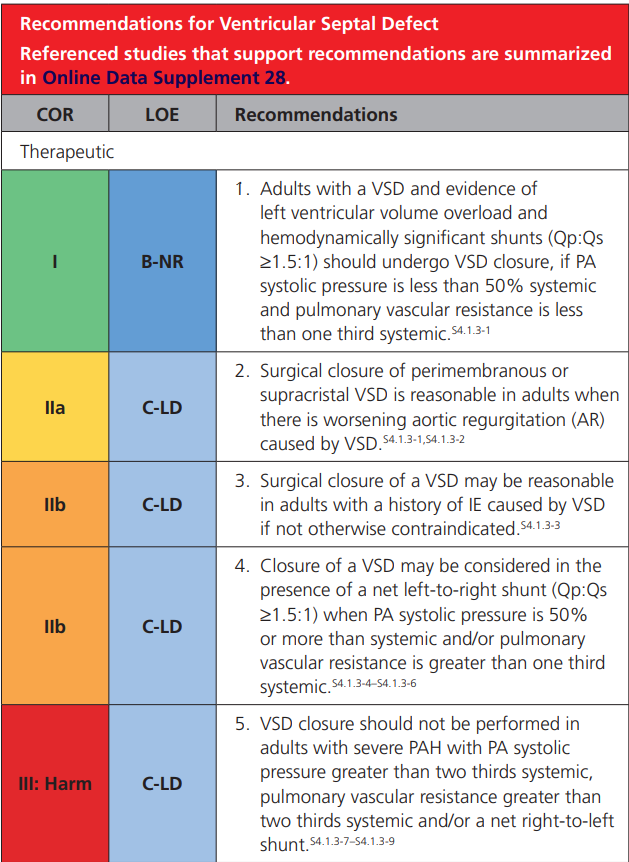
2018 AHA/ACC ACHD Guideline
2018 AHA/ACC ACHD Guideline
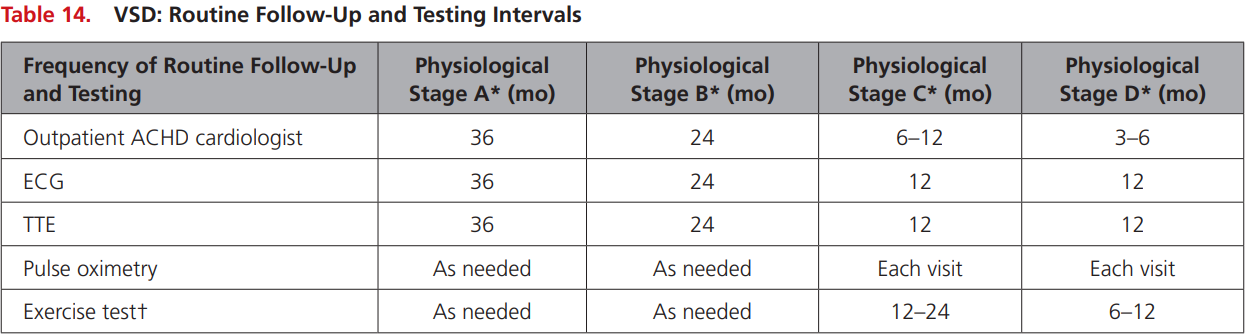
Stage A: NYHA FC I, no complications
Stage B: NYHA FC II, mild complications
Stage C: NYHA FC III, moderate complications
Stage D: NYHA IV, severe complications
2018 AHA/ACC ACHD Guideline

VSD Case
- 28yo M referred to cardiology for chest pain and fatigue associated with fevers. Found to have spontaneous type I Brugada
- Physical exam: S1S2, no RV lift or apical displacement. No signs of volume overload.
VSD Case
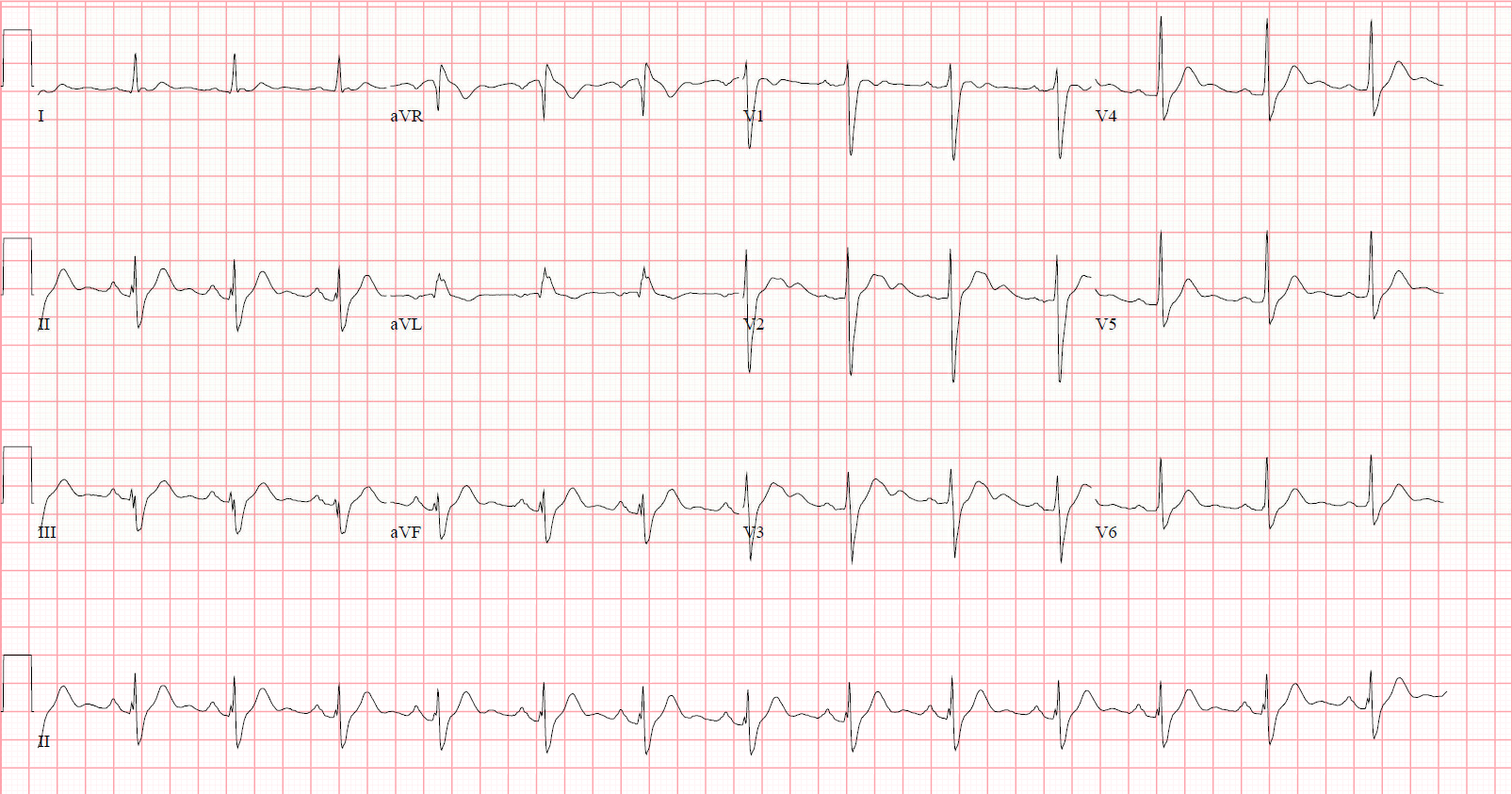
VSD Case
VSD Case
VSD Case
- Small restrictive VSD
- The patient will be followed long term
Patent Ductus Arteriosus
PDA
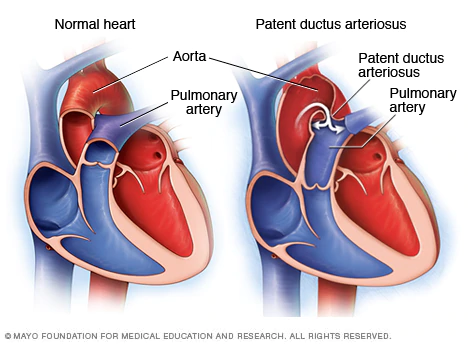
PDA
- Associated with maternal rubella
- More common in women (3F:1M)
Clinical features:
- Brisk upstroke pulse
- Dynamic LV
- Continuous "machinery murmur" best heard under the left clavicle
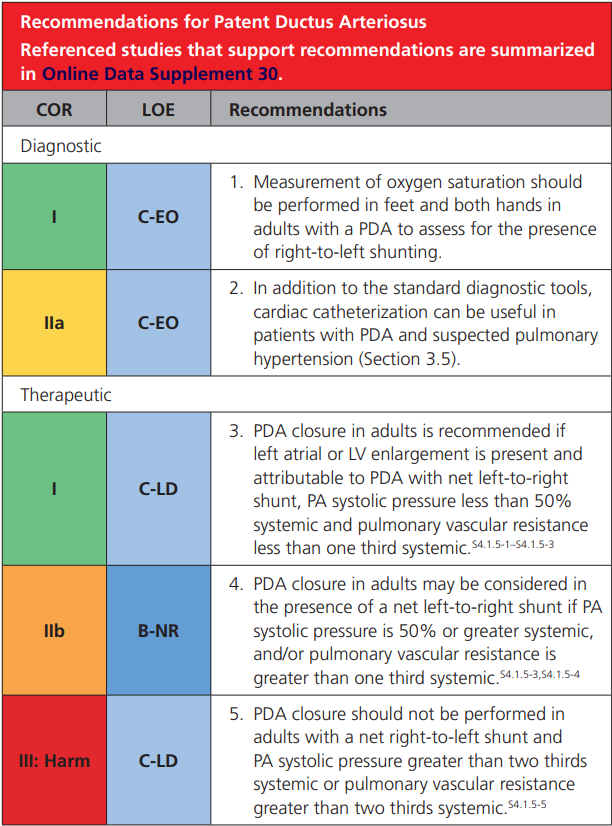
2018 AHA/ACC ACHD Guideline
PDA: Echocardiogram
- Parasternal Long Axis: PDA at the pulmonary end
- Parasternal Short Axis: Views of the main pulmonary artery and aorta
- Apical 4 chamber: Assess for evidence of left atrial, LV dilation
- Subcostal: PDA may cause runoff in the abdominal aorta - can be seen as flow reversal in diastole
- Suprasternal notch: Presence and directionality of shunting across the PDA between the aortic arch and main pulmonary artery
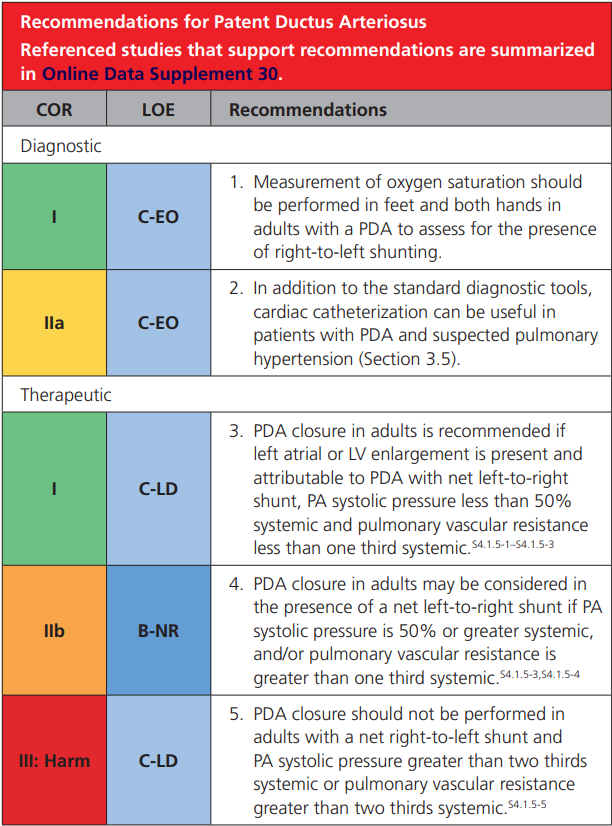
2018 AHA/ACC ACHD Guideline
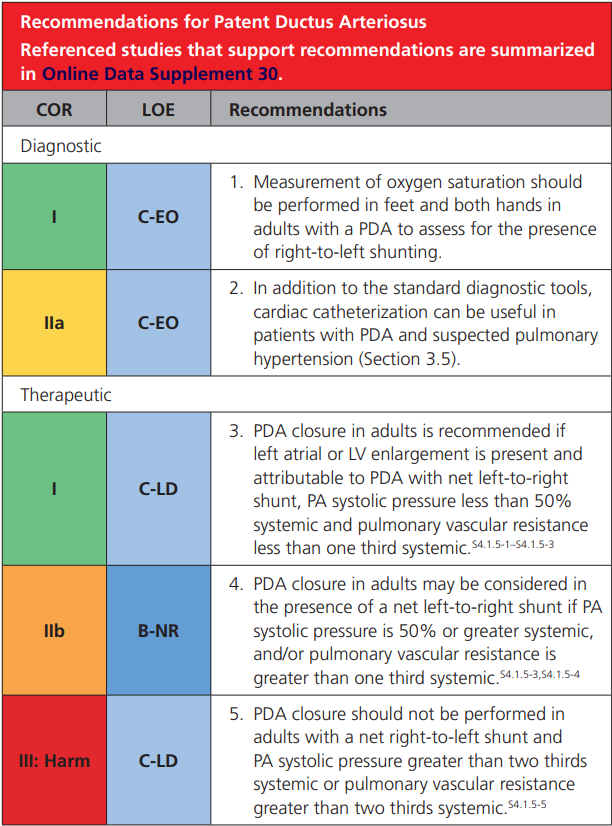
2018 AHA/ACC ACHD Guideline
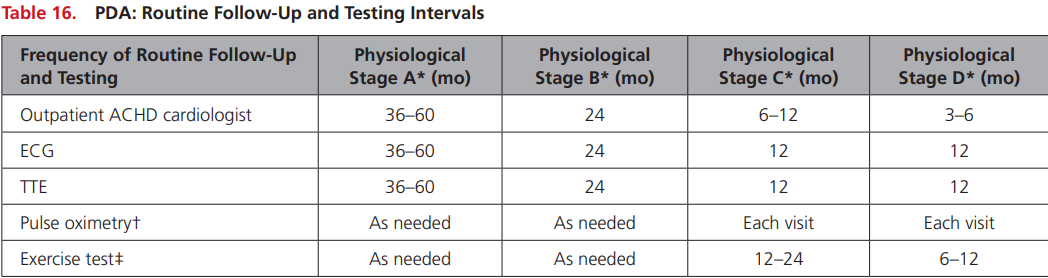
Stage A: NYHA FC I, no complications
Stage B: NYHA FC II, mild complications
Stage C: NYHA FC III, moderate complications
Stage D: NYHA IV, severe complications
PDA Case
- 32 yo F with history of syncope at 18 yo investigated with echo found to have a PDA. She has occasional palpitations
- Physical exam: S1S2, soft systolic ejection murmur over the left sternal border, no continuous murmur, no RV lift
PDA Case: Echocardiogram
- Parasternal Short Axis: Views of the main pulmonary artery and aorta
PDA Case: Echocardiogram
- Apical 4 chamber: Assess for evidence of left atrial, LV dilation
PDA Case: Echocardiogram
- Suprasternal notch: Presence and directionality of shunting across the PDA between the aortic arch and main pulmonary artery
PDA Case: Conclusion
The echocardiogram suggested a shunt ratio 1.3:1, no evidence of left-sided dilation or dysfunction.
She continues to be followed