Health, Wealth, and Public Policy
Sarah Miller
Hosmer Hall
Discussing joint work with Laura Wherry, Beth Rhodes and others
Poor People Have Poor Health

Where should we intervene?

Health Interventions
Strong link between health at birth and adult achievement (see Almond and Currie 2011 for an overview).
- Many studies look at negative shocks occurring early in life (flu pandemics, famine, poor nutrition, exposure to pollution); less evidence on policy-driven choices (food stamps, salt iodization).
Notoriously poor health outcomes for low income mothers and babies.
Could an early life health intervention break this cycle?
Coverage for Low Income Pregnant Women
Miller and Wherry, forthcoming Journal of Human Resources
From 1979 to 1993, fraction of women eligible for Medicaid in the event of a pregnancy more than tripled.
Single largest effort to improve prenatal and birth outcomes in the United States.
Initial evidence (e.g. Currie and Gruber 1996) suggested moms used more prenatal care, had more health interventions at the hospital, and gave birth to healthier babies.
Did better health at birth lead to better adult outcomes for those who gained coverage "in utero"/as newborns?
Coverage for Low Income Pregnant Women
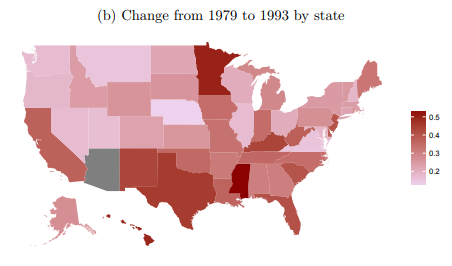
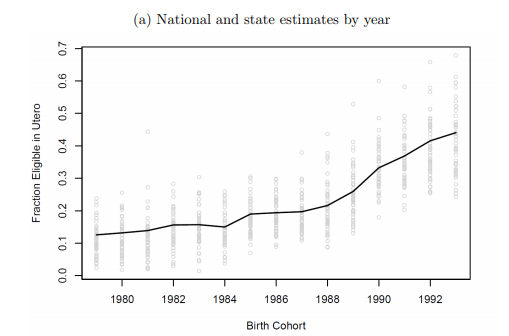
Use an instrumental variables model to separate policy-driven changes in eligibility from changes driven by (potentially endogenous) economic factors.
Long-Term Effects of Early Life Medicaid Coverage
Those who gained coverage in utero/as newborns:
Lower incidence of chronic disease in adulthood (particularly diabetes, high blood pressure).
Fewer hospitalizations for these types of conditions.
More likely to graduate high school.
Higher incomes, lower food stamps receipt rates [suggestive].
Effects are not huge, but show that health interventions can change economic outcomes
Intergenerational
Follow-up work using the same identification strategy looks at what happens when these cohorts themselves have children.
Can these policies echo across generations?
East, Miller, Page, and Wherry. 2018. "Multi-generational Impacts of Childhood Access to the Safety Net: Early Life Exposure to Medicaid and the Next Generation's Health" (r&r)
Intergenerational
Mothers who gained Medicaid eligibility in utero gave birth to babies with:
- higher birthweight (~30 grams)
- lower percentage in "very low birthweight" category (~1 percent)
- No changes in childbearing quantity or timing
East, Miller, Page, and Wherry. 2018. "Multi-generational Impacts of Childhood Access to the Safety Net: Early Life Exposure to Medicaid and the Next Generation's Health" (r&r)
Health Interventions Agenda
- Childhood Coverage Reduces Adult ED and Hospitalizations: Uses a regression discontinuity design comparing kids born just after a birth date eligibility cutoff. (Wherry, Miller, Kaestner and Meyer 2018 Review of Economics and Statistics)
- ACA Medicaid Expansions Improved Access to and Use of Care: Miller and Wherry 2018 New England Journal of Medicine, Wherry and Miller 2017 Annals of Internal Medicine, Carey, Miller and Wherry 2018 NBER Working Paper.
- Impact of Medicaid Expansions on Financial Outcomes: Mazumder and Miller 2016 AEJ: Economic Policy, Hu, Kaestner, Mazumder, Miller and Wong forthcoming Journal of Public Economics, Miller et al 2018 NBER Working Paper
The Other Causal Arrow
Meaningful improvements in economic and financial outcomes that result from health interventions. But could we reduce health disparities by targeting the "other" arrow?

Basic Income RCT
With Y Combinator and University of Chicago Poverty Lab, I am working on a randomized controlled trial of a "basic" income.
Intervention: $1000/month for 3 years; N=1100.
Control: $50/month for 3 years, N=2000.
- Tax free (according to the lawyers).
- Two sites (one Midwest, one sunbelt), mix of urban, suburban, and rural.
- Eligibility: below median income (with over-sampling of low income), excludes recipients of SSI, SSDI, and housing assistance.
In-person enrollment and surveys conducted by UMich's SRC.
Could receiving a basic income improve health?
Collecting outcome data on:
Biomarkers (height, weight, blood pressure, blood sugar, cholesterol).
Healthy behaviors (sleep, exercise).
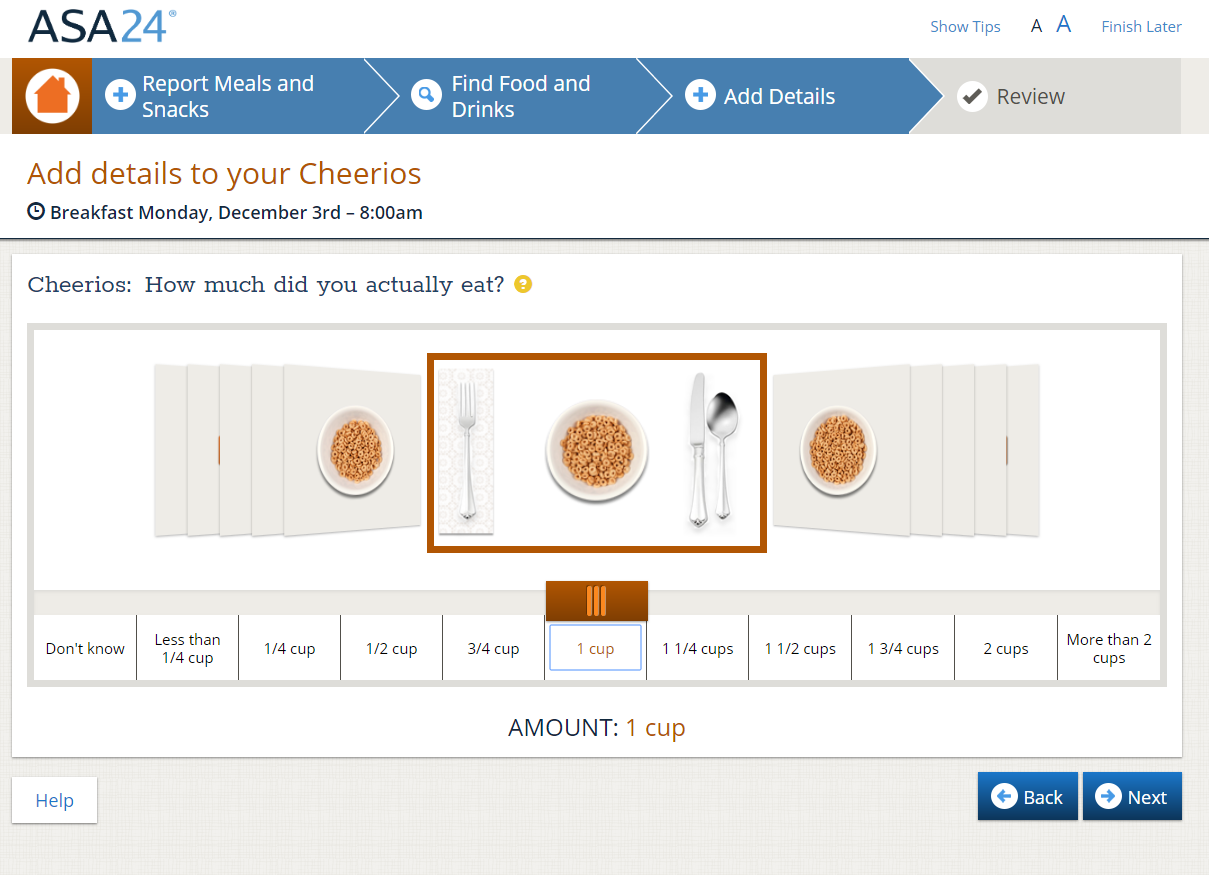
Nutrition diaries.
Use of health care services.
Insurance coverage.
Stress and mental health (including cognition/decision-making).
Current Status
Pilot:
This fall, SRC enrolled 100 individuals in our pilot which runs until the end of January.
Goals of the pilot:
- Testing out passive data cell phone collection (GPS, time spent on social media etc).
- Testing out survey collection via "apps" versus traditional surveys.
- Refining survey instruments.
- Match rates to admin data.
- Ironing out logistical bugs.
April 2019: Enrollment in the main study begins.
Study will run through 2022.
Current Status

Current Status
Future Health Intervention Projects
Bringing big (bigger!) data to early life health research:
Linked all birth records for those born in California from 1960 to 2014 to:
the 2000 Census
2001-2017 American Community Survey
Administrative records on mortality from SSA
Admin records on SSI receipt
Admin records on TANF receipt
Admin data on quarterly earnings from UIAs
Admin data on Medicaid/Medicare enrollment
Admin data on college attendance from NSC
Other Health-related Data Linkage Projects
- Credit report/payday loan data linkage project with Cindy K Soo (Finance).
- Currently linking UM EHR data to Michigan administrative data on earnings to look at the effect of pregnancy interventions on mothers' return to workforce/future earnings.
- Project with Turnaway Study on long-term financial/economic effects of being denied an abortion.
- Selected to conduct long-term follow up analysis of Family Options Study RCT by HUD using admin data.
All at different stages of progress...
Questions?
Always happy for feedback:
mille@umich.edu