The Affordable Care Act and Mortality
Sarah Miller
University of Michigan
Ross School of Business
Context
High degree of inequality in health outcomes by income.
- 55-64 year olds in households earning under 138 FPL have annual mortality rate of 1.7pp. In households earning 400%FPL+: 0.4pp. 4x higher for low income households.
- 787% higher chance of dying from diabetes, 552% higher chance of dying from cardiovascular disease, 813% higher chance of dying from respiratory disease.
- Correlation between income and health exists in all countries, correlation is higher in the US than in other wealthy countries (Semyonov, Lewin-Epstein and Maskileyson 2013).
Could the coverage expansions help reduce these very high mortality rates?
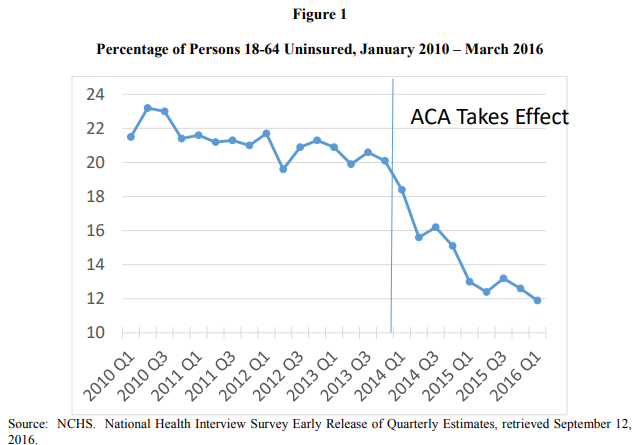
Overall Coverage Gains
The number of people with insurance increased by about 20 million
Source: Duggan, Goda, Jackson 2017 NTA
2014 Coverage Expansions
Eligibility for Medicaid extended to everyone with incomes below 138% of the Federal Poverty Level (effective Jan 2014 for most states.)
Originally intended to be implemented in all states, but due to a 2012 Supreme Court decision, this became optional.
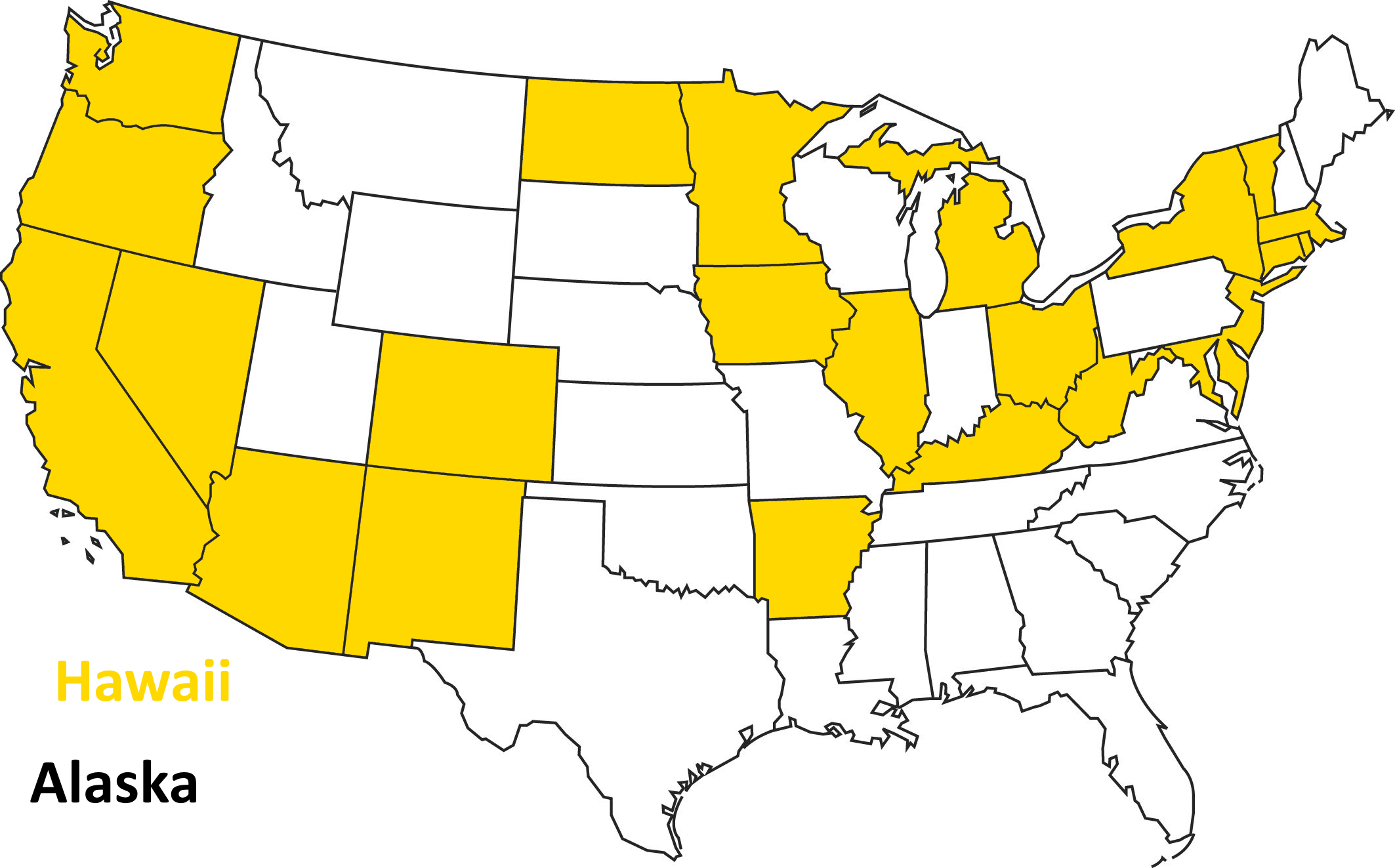
Opted to Expand in 2014
Coverage Gains Largest in states that expanded Medicaid
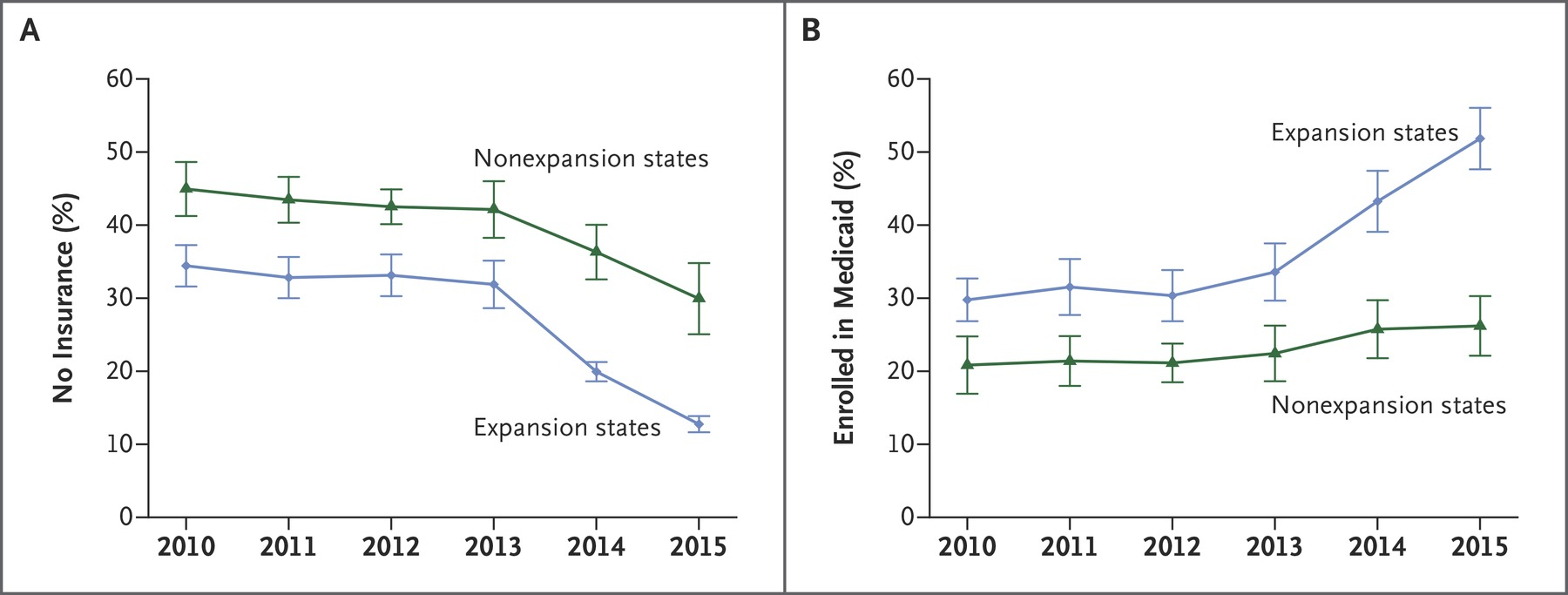
Sample among low income adults, Miller and Wherry 2016 New England Journal of Medicine
Analysis of ACA Medicaid Expansions
- In joint work with Altekruse, Johnson, and Wherry...
- Take advantage of non-universal adoption of the Medicaid expansion that resulted from the 2012 Supreme Court decision.
- Use a "difference in differences" quasi-experimental empirical design
Compare changes in outcomes across expansion and non-expansion states.
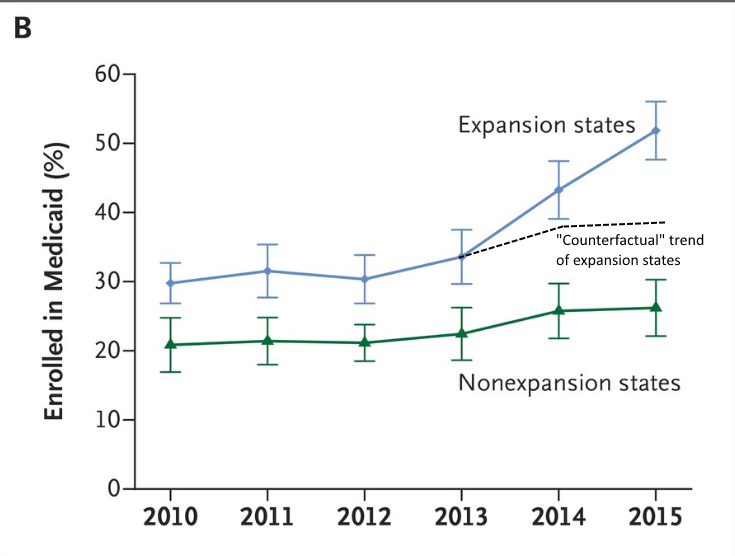
Expansion states and non-expansion states might be at different levels, but are they on the same trajectory?
Difference in Differences
Let's go back to this figure:
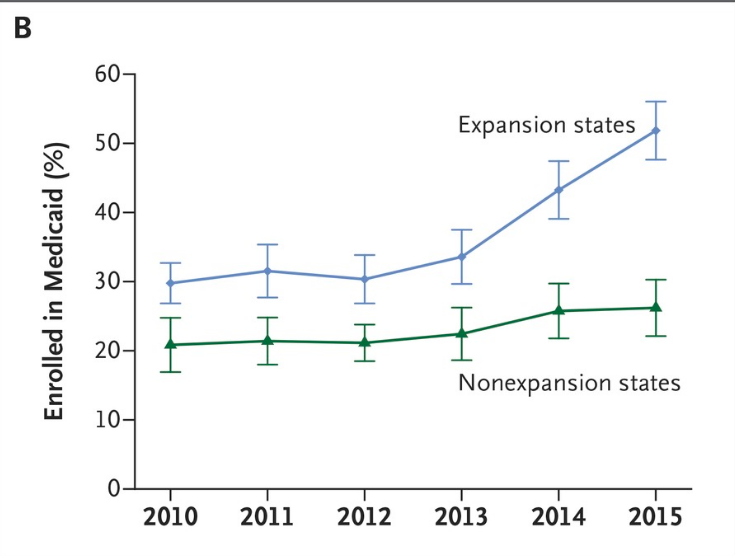
Difference in Differences
Let's go back to this figure:
Linked Survey and Admin Data
Link data from American Community Survey (ACS) to Social Security Administration mortality records
- ACS is large survey (4 to 4.5 million respondents per year) and has information on household income, eligibility for other programs, and other information relevant to determine who is most likely to gain eligibility
- We focus on individuals age 55-64, low income or disadvantaged (no high school degree), not otherwise Medicaid eligible, citizens.
- A large % of this group gained Medicaid eligibility.
- Follow this group across expansion and non-expansion states for 4 years after the ACA expansions.
How Many Gained Eligibility?
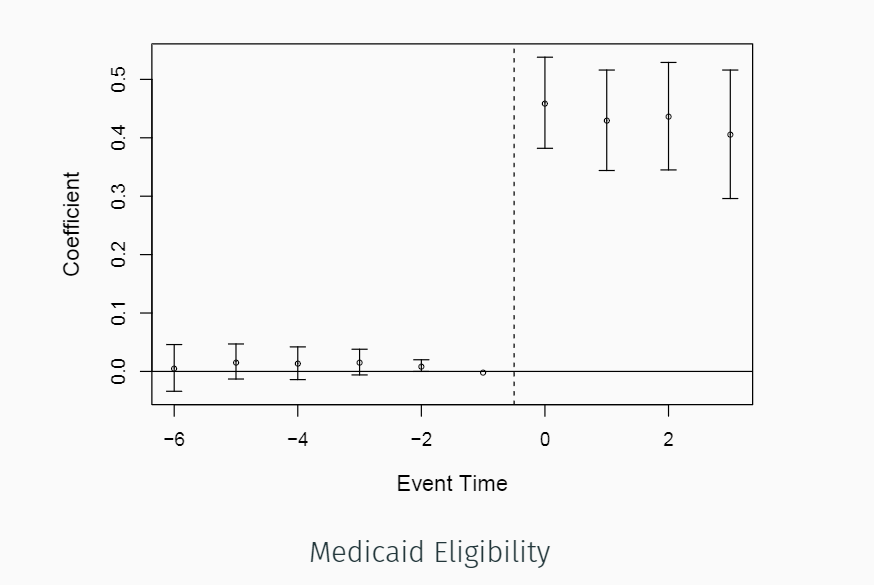
Nearly half of the group gained eligibility
How Many Enrolled?
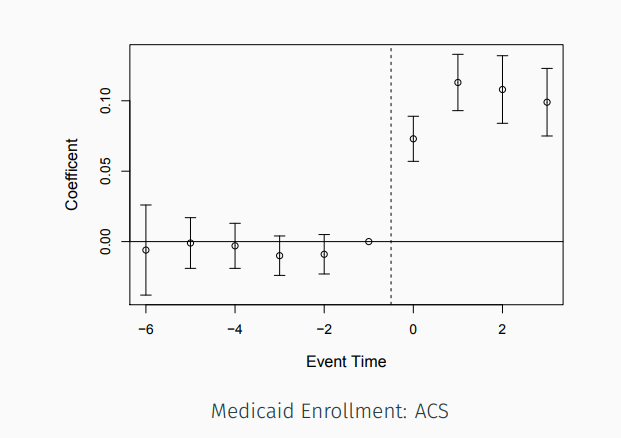
About 10-11percent enrolled (possibly higher due to misreporting in survey)
Takeaway?
In the paper, we show this for other measures and other surveys (NHIS) as well.
- Successfully identified a group that was highly impacted by Medicaid expansions.
- ACA policy had meaningful impact on coverage for this group.
Mortality Reduction from Medicaid
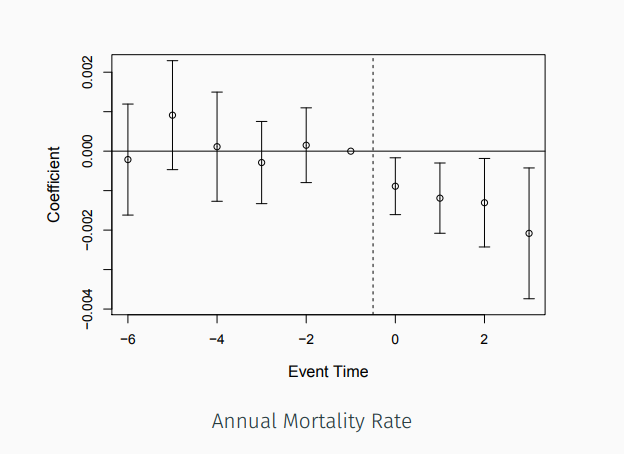
Reduction of 0.09 percentage points first year, increasing to about 0.2 percentage points by year 4
Mortality Reduction from Medicaid
Is this big or small?
~3.7 million people meeting our sample criteria in expansion states: implies 19,200 deaths averted over the period we study
~3 million people meeting our sample criteria in non-expansion states:
implies 15,600 excess deaths that would have been averted if the state had expanded.