Health care spending in the United States: Where are we coming from and where are we going?
Per capita health care spending in the US and OECD countries in 2021 (source: OECD health Statistics)

Health Spending per Capita, 1980–2019
Source: KFF and Peterson/Kaiser Health System Tracker (based on NHE data)

Health Spending as Percent of GDP, 1970–2021
Source: Commonwealth Fund analysis of OECD Health Data

A big part of this difference is driven by prices
- Americans don't use a particularly large quantity of care
- Except for diagnostic services/imaging, we tend to use less care - fewer hospital stays, shorter lengths of stay, fewer drs visits etc.
- So why are prices so high?
So.. where do prices come from?



Negotiate rates



Negotiate rates


Choose among providers--based on what?
So.. where do prices come from?



Negotiate rates


Choose among providers

Competition among insurers affects mark-up above claims.
So.. where do prices come from?
Provider Competition
•Competition in markets takes place in 2 stages.
Stage 1: hospitals & insurers negotiate over network inclusion & price.
Stage 2: Hospitals compete for patients (not typically on price).
•Negotiated prices will depend on:
~ importance of provider is to insurer’s network
~ willingness of insurer to steer patients elsewhere
The balance of power has changed over time.
Pre-Managed Care Era
•Fee-for-service indemnity insurance predominated.
~Insurers were passive: little or no negotiating
~Plans covered “all willing providers”, paying “usual, customary and reasonable” fees
•Hospitals competed via a “medical arms race.”
~High tech capital, non-clinical amenities as a signal of quality
~Cost-based reimbursement => excess capacity & incentive for over-use
This led to high spending, spurring the rise of managed care.
Managed Care "Revolution" (?)
•Insurers began using supply-side strategies to lower costs.
~Aimed at lowering both P and Q
•Utilization review used to control costs by reducing quantities
~Reducing admissions, unnecessary tests and procedures
~Managing care = saying no
•Negotiating lower prices with providers
~Selective contracting: offering volume in return for lower prices
Post-Managed Care "Revolution"
Gains from managed care were not sustained. There were several factors behind the “managed care backlash.”
1.Employers wanted broad networks
2.Provider push-back
3.Provider consolidation
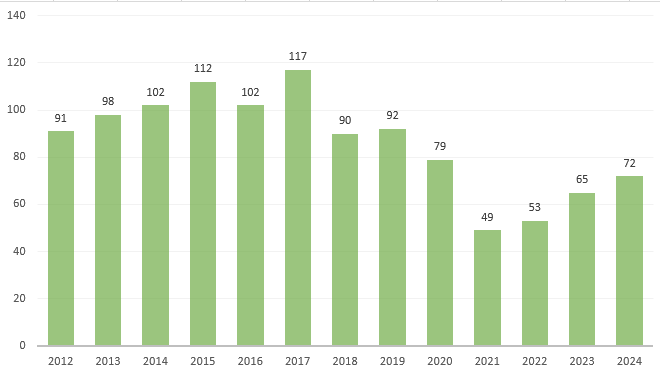
Hospital Mergers and Acquisitions
Source: Kaufman Hall Transactions Data
Trends in Hospital Payments by Payer

Selden et al Health Affairs 2015
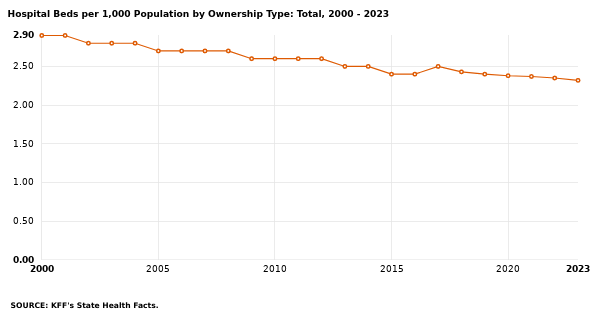
Hospital Beds per Population (1000)
Market Concentration
Hospital markets have changed!
In the 1980s: 5 major competitors + smaller players
By 2010s: 1 dominant system, 2-3 fringe players
- 16% of hospital markets are monopolies
- 19% of hospital markets are duopolies
- Only about half have at least 4 players
Markets that are monopolies have higher prices and these hospitals are less likely to participate in risk-sharing contracts (Cooper et al. 2018).
History of Hospital Anti-trust Action
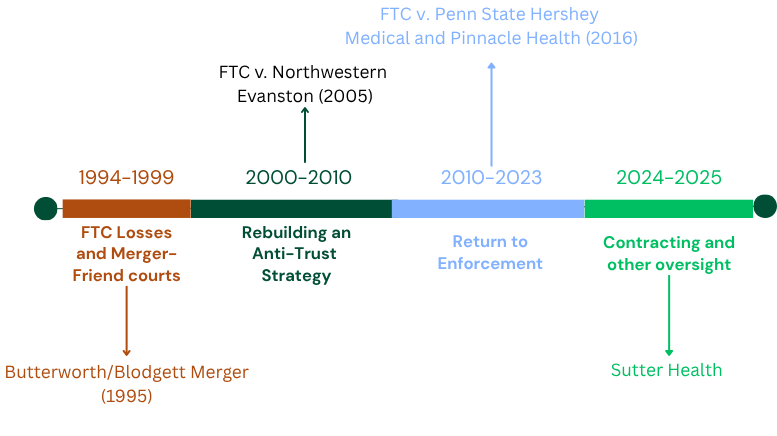
Is there enough hospital anti-trust?
- From 2002-2020 there were 1000 hospital mergers.
- The FTC blocked 13.
- 90 percent of hospital markets are considered "highly concentrated."
In a typical merger year between 2010 and 2015, the mergers increased spending by $204 million.
The entire budget for enforcement for the FTC is $136 million.
Challenges in the US

These Challenges are Tightly Connected

Rising costs have led to an erosion of insurance coverage
Over-utilization increases costs and harms patients
The uninsured often go without necessary care
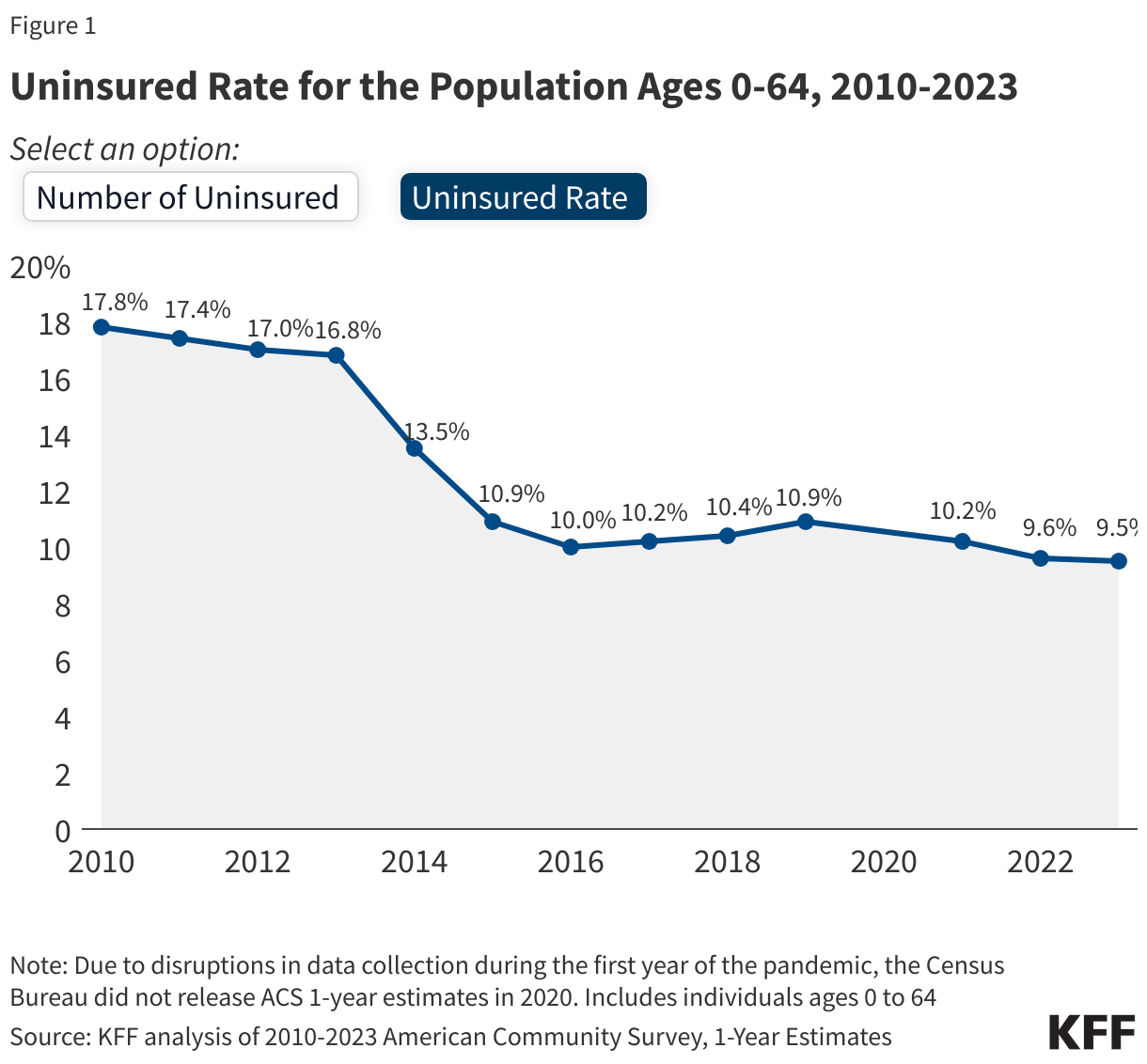
Who remains uninsured?
- Low-income adults in "coverage gap" in states like Texas, Florida, South Carolina etc.
- Young "invincibles" those age 19-25
- Ineligible for assistance due to immigration status
Policy Changes On the Horizon
- Current government shut down is in part due to expiration of temporary enhanced health insurance subsidies
- What is "affordable"?
- HR1/OBBB changes to Medicaid and ACA exchanges
- ~10mill additional uninsured
- Key elements of the ACA remain in place, but these will probably result in uninsured rate ticking up.

"Bending the cost curve"
Cutler et al. Health Affairs 2019
Silver linings?
Cutler et al. Health Affairs 2019

Silver linings?
Silver linings?