



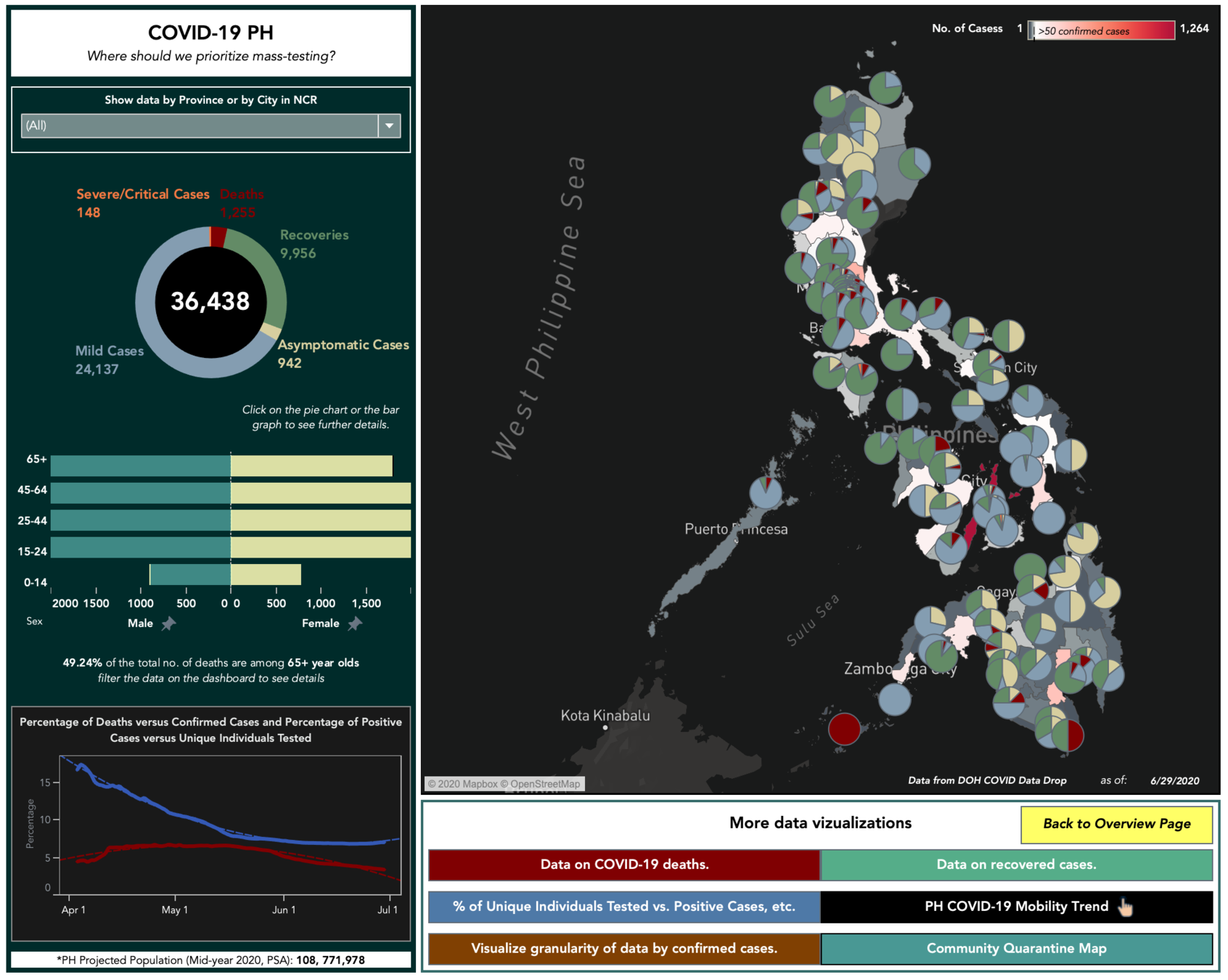
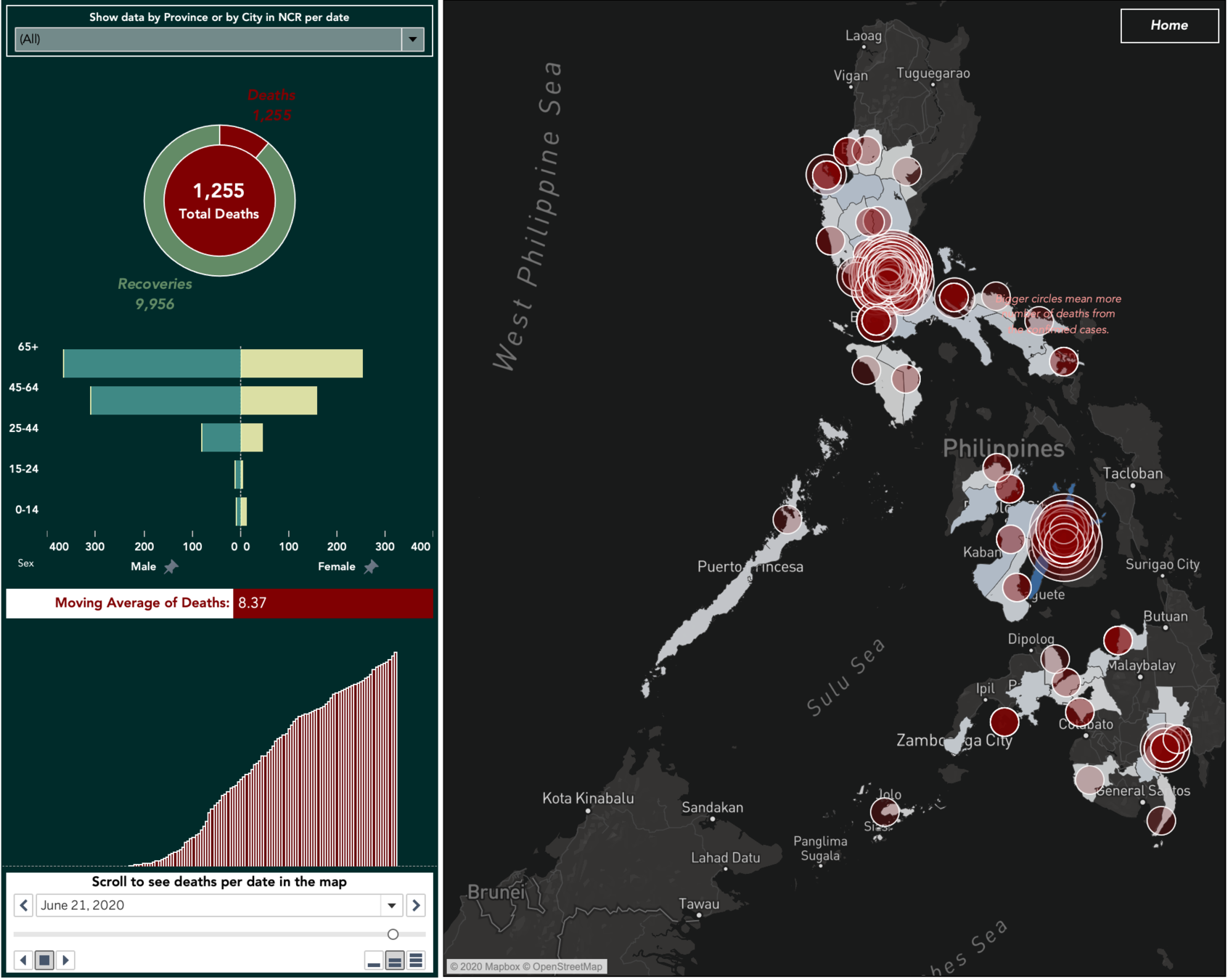
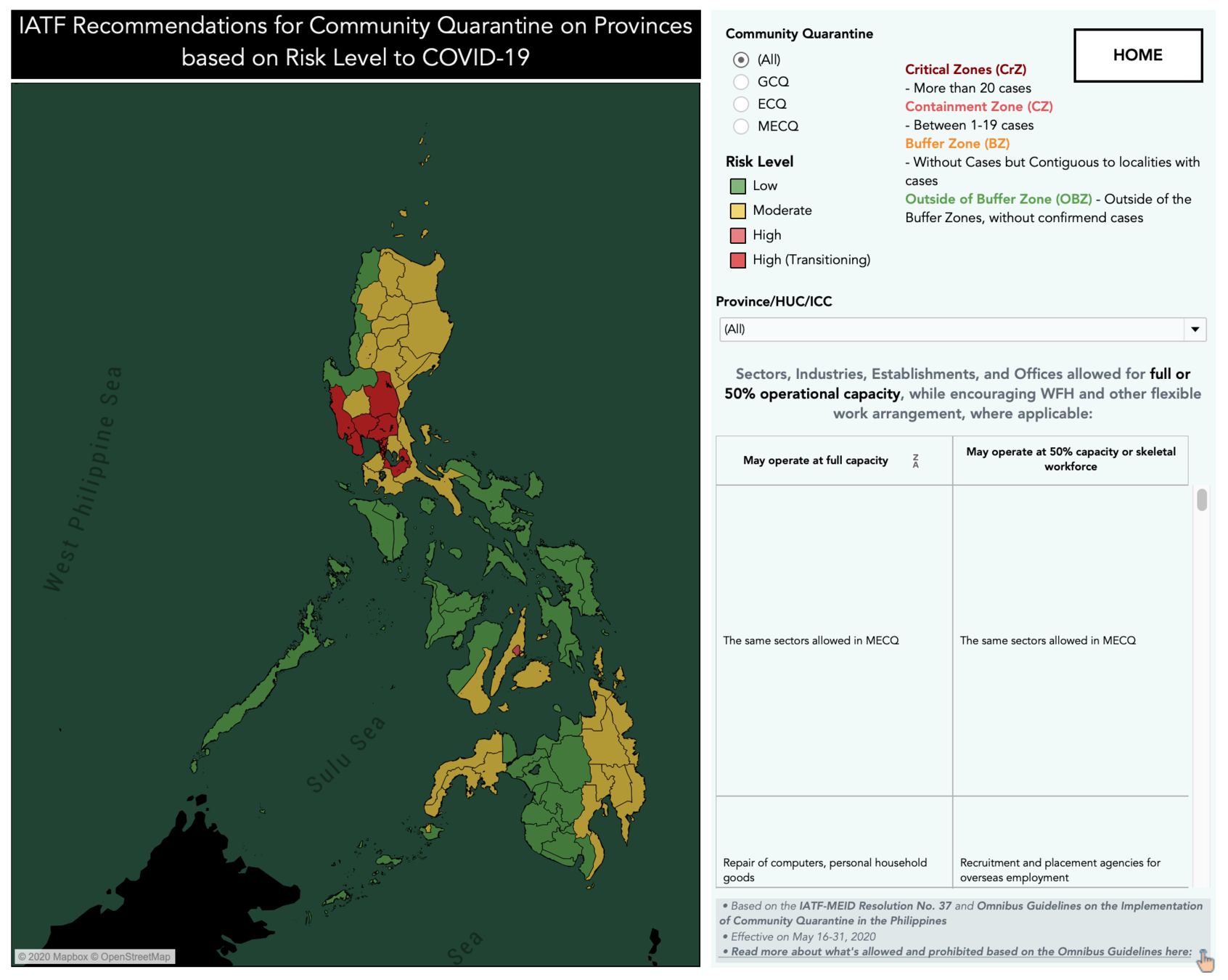
https://bit.ly/COVID19PHdash


Common responses of people affected (both directly and indirectly) might include:
-
Fear of falling ill and dying
-
Avoiding approaching health facilities due to fear of becoming infected while in care
-
Fear of losing livelihoods, not being able to work during isolation, and of being dismissed from work
-
Fear of being socially excluded/placed in quarantine because of being associated with the disease (e.g. racism against persons who are from, or perceived to be from, affected areas)
-
Feeling powerless in protecting loved ones and fear of losing loved ones because of the virus
-
Fear of being separated from loved ones and caregivers due to quarantine regime
-
Refusal to care for unaccompanied or separated minors, people with disabilities or the elderly due to fear of infection, because parents or caregivers have been taken into quarantine
-
Feelings of helplessness, boredom, loneliness and depression due to being isolated
-
Fear of reliving the experience of a previous epidemic
Source: WHO-IASC Interim Briefing Note on COVID-19
Outbreak Readiness and Response Operations for Mental Health
and Psychosocial Aspects












Community Care



committing to being there for others and intentionally showing compassion






How about outside your circle?



‘WHOLE OF SOCIETY’ APPROACH
- Promotion of self-care strategies, such as breathing exercises, relaxation exercies or other cultural practices
- Normalisation messages about fear and anxiety and ways people can support others
- Clear, concise and accurate information about COVID-19, including how to access help if one becomes unwell.


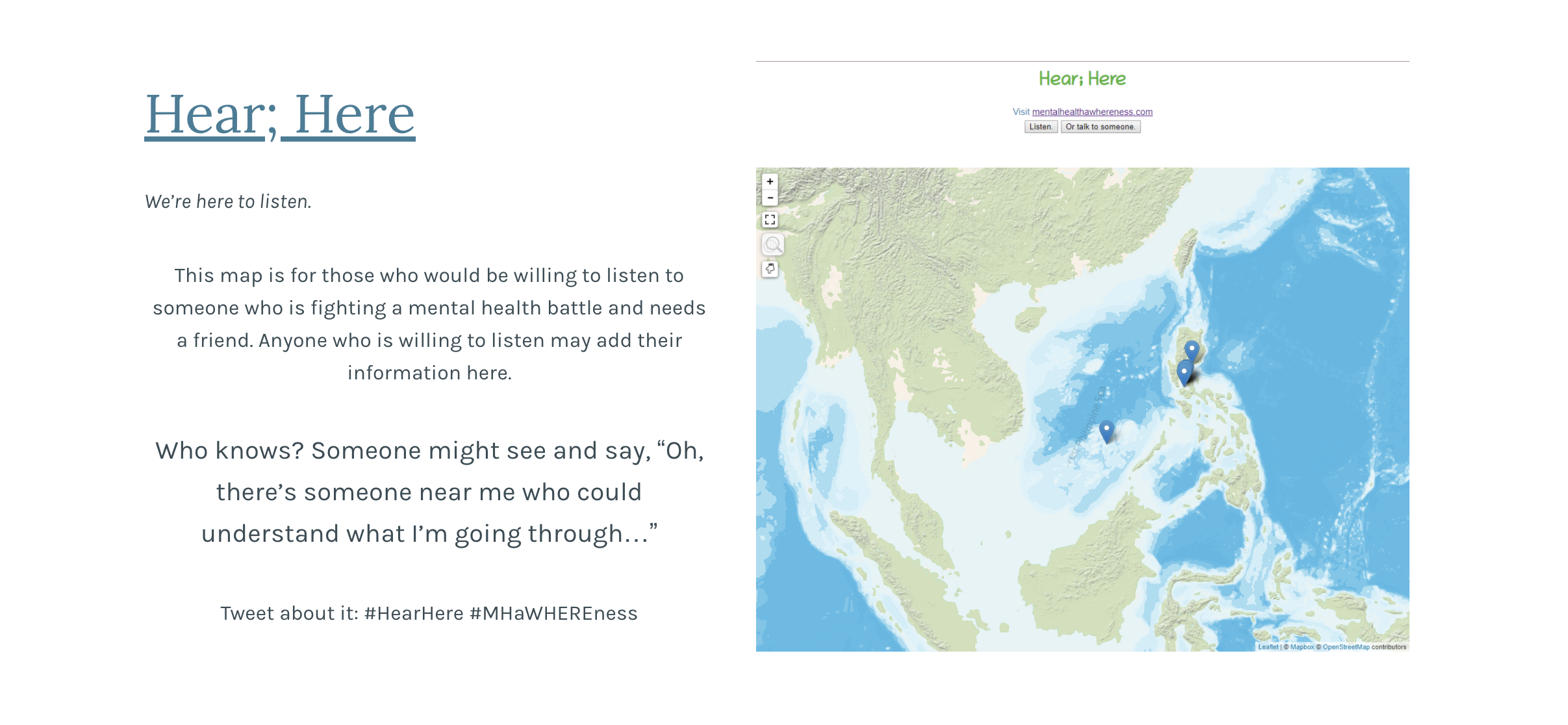
BIT.LY/HEARHEREADDANDVIEW
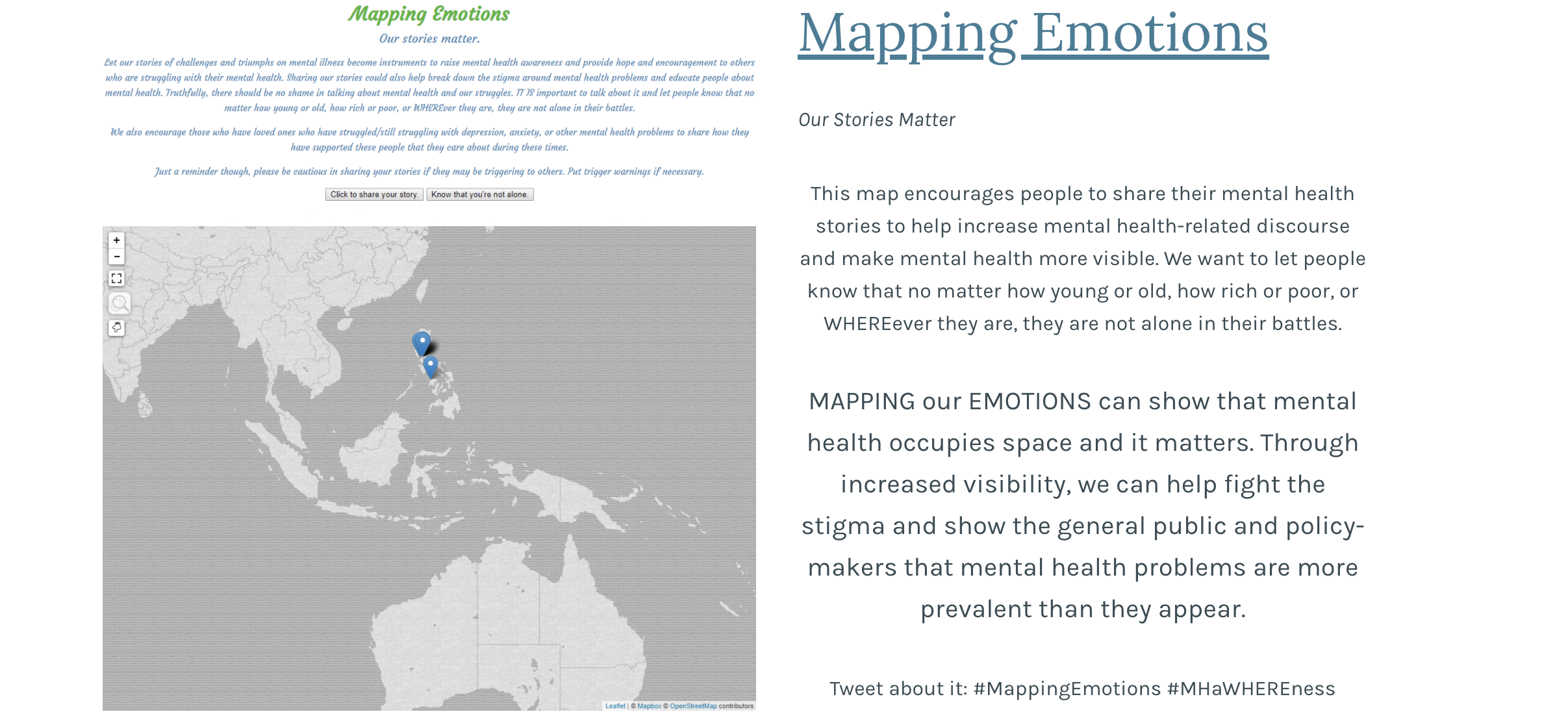
BIT.LY/MAPPINGEMOTIONS


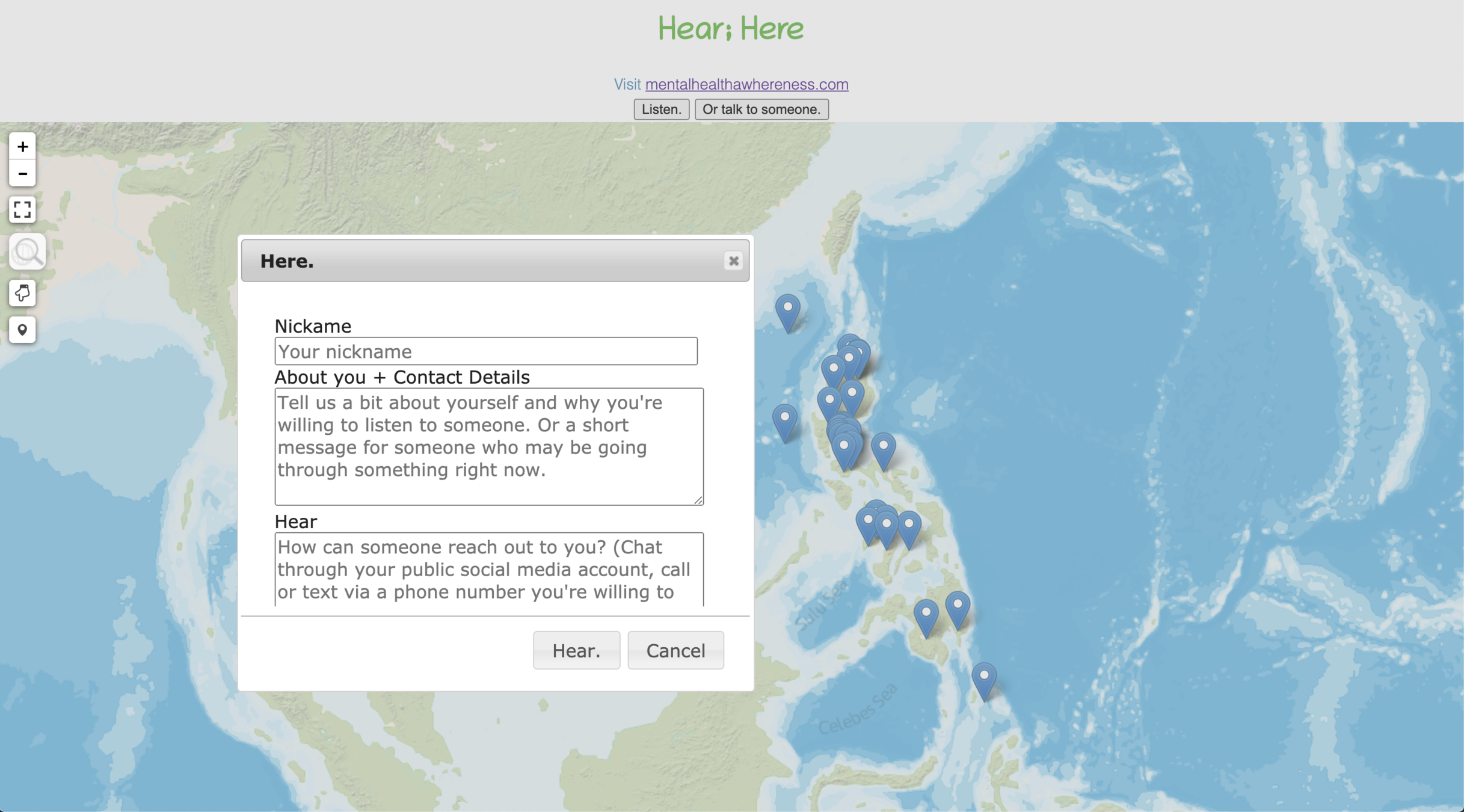
BIT.LY/HEARHEREADDANDVIEW_MHA


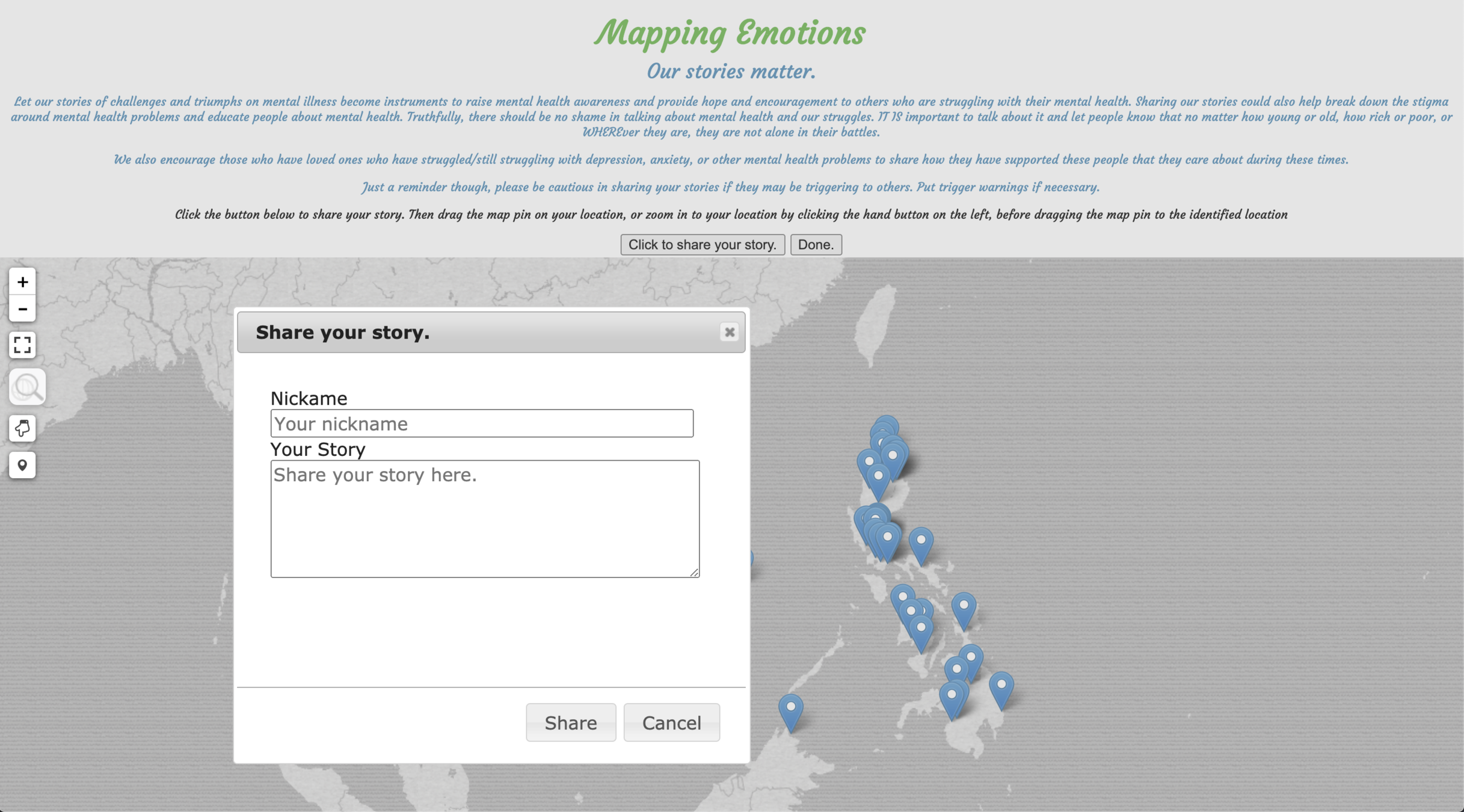
BIT.LY/MAPPINGEMOTIONS_MHA







EMPHASIZED COORDINATION
Coordination amongst all sectors/emergency pillars involved in the response.
KNOWLEDGE AND EXPERTISE SHARING
Where there are gaps in knowledge and expertise, online training for MHPSS in emergencies should be facilitated and pooled.









EXISTING SERVICES
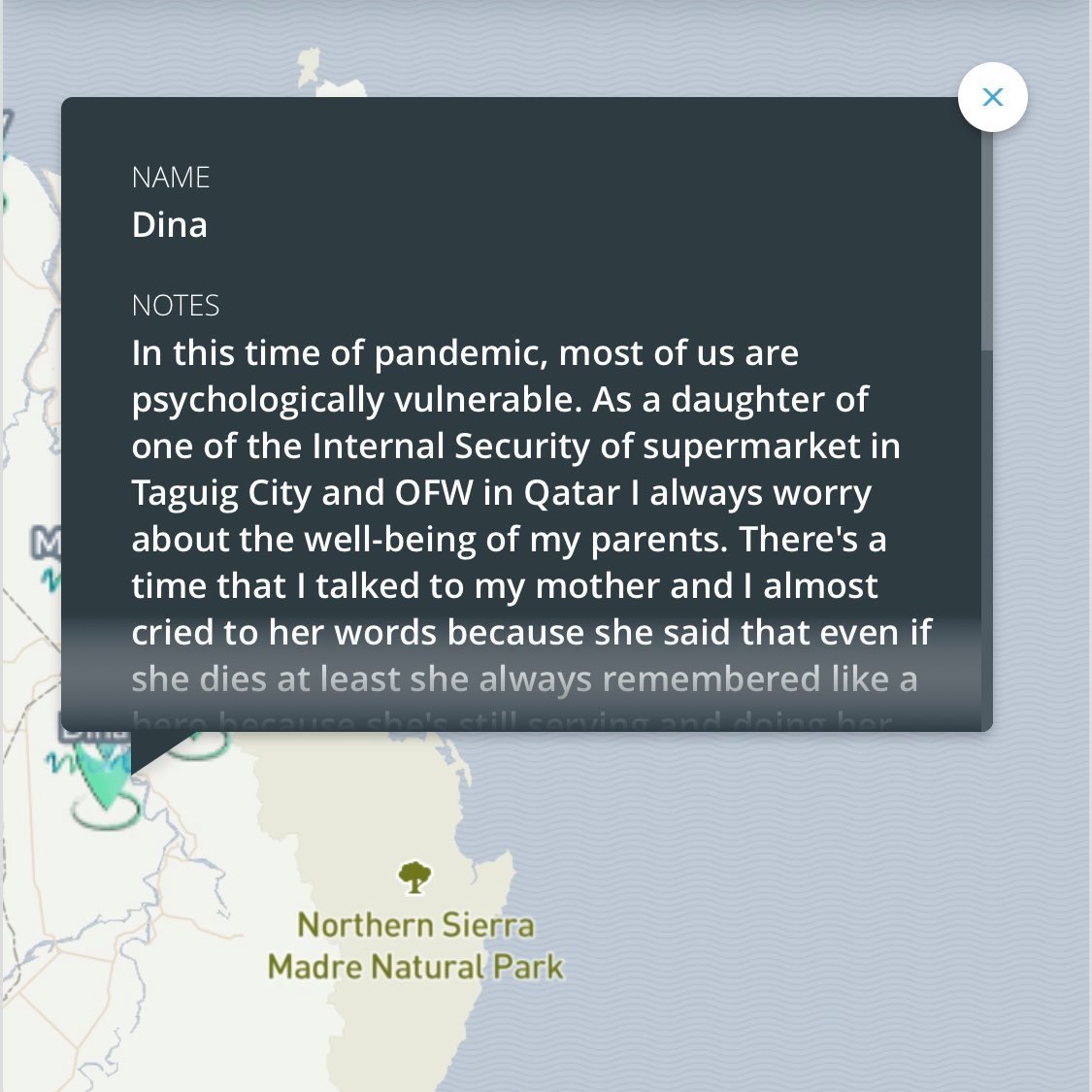
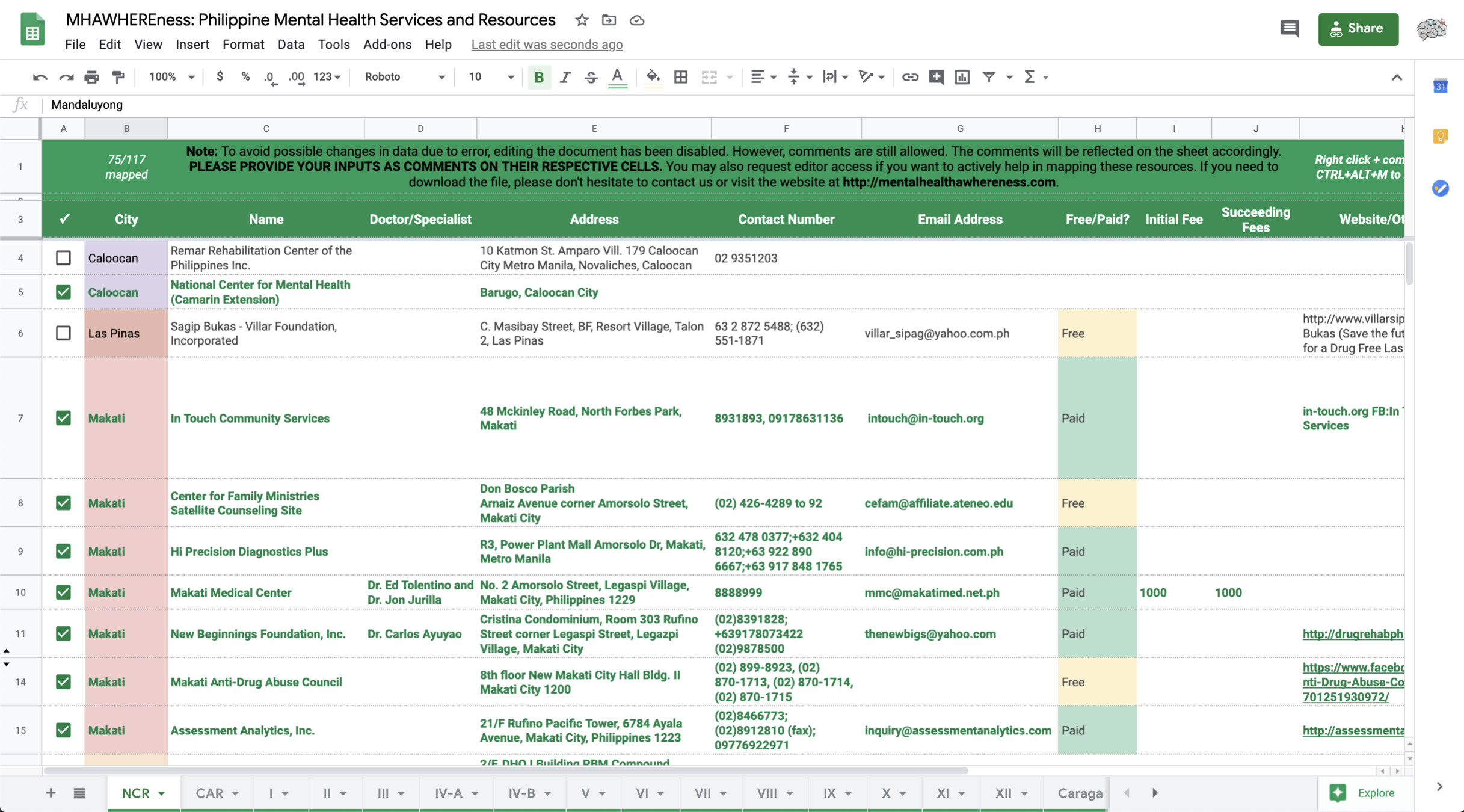
It is important to map existing Mental health and psychosocial support (MHPSS) expertise & structures in each region, including private & public health, social welfare and education services. Mapping serves as a mechanism to pool, mobilize and coordinate resources









mentalhealthawhereness@gmail.com
https://facebook.com/mentalhealthawhereness
https://twitter.com/MHawhereness
anditabinas@gmail.com
Maraming salamat po!
Mental Health AWHEREness PH (MHAPH)