Stress Echo 2030
ABCDE+ Protocol
Cardiology Rounds Oct 16, 2024 | Atul Jaidka
Objectives
- Discuss components of the ABCDE+ Protocol
- Discuss evidence for the ABCDE+ Protocol
- Practical applications of the ABCDE+ Protocol in the Echo Lab
Background
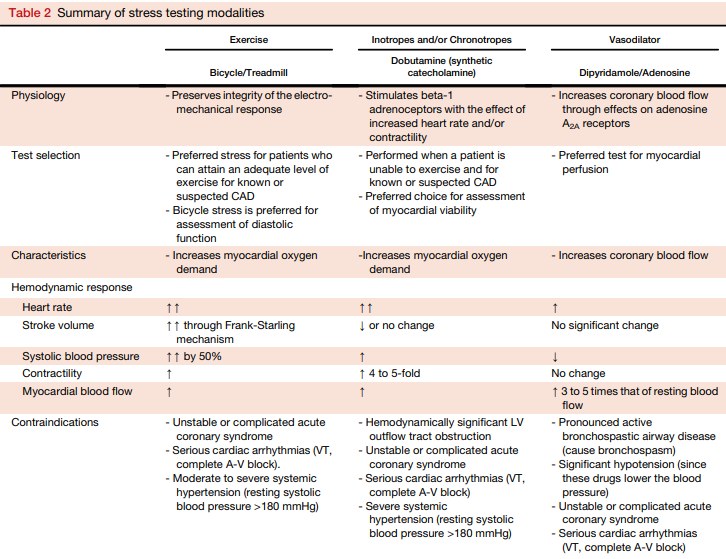
Traditional Stress Echo
-
Identification of regional wall motion abnormalities to identify obstructive coronary artery disease
- Qualitatively assessed
- Other prognostic parameters:
- Exercise duration, BP response, ST-T changes and LV dilation (not reliably reported)
- Functional test: thus does not diagnose non-obstructive atherosclerotic disease that can still cause events
Compared to Alternatives
-
Advantages
- Inexpensive
- No radiation
- Portable
- Exercise and non-exercise
- Less environmental impact compared to MRI/SPECT
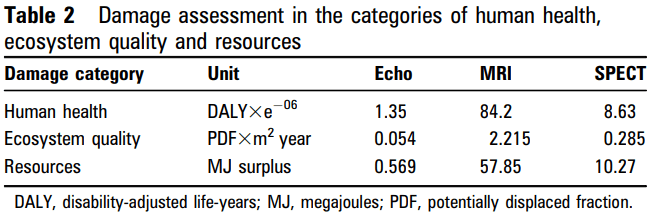
Compared to Alternatives
-
Disadvantages
- Functional testing thus may not pick up non-obstructive clinical atherosclerosis that can cause future events
- Compared to Coronary CT
- WMA are later in the ischemic cascade (not capturing perfusion changes)
- Compared to myocardial perfusion imaging
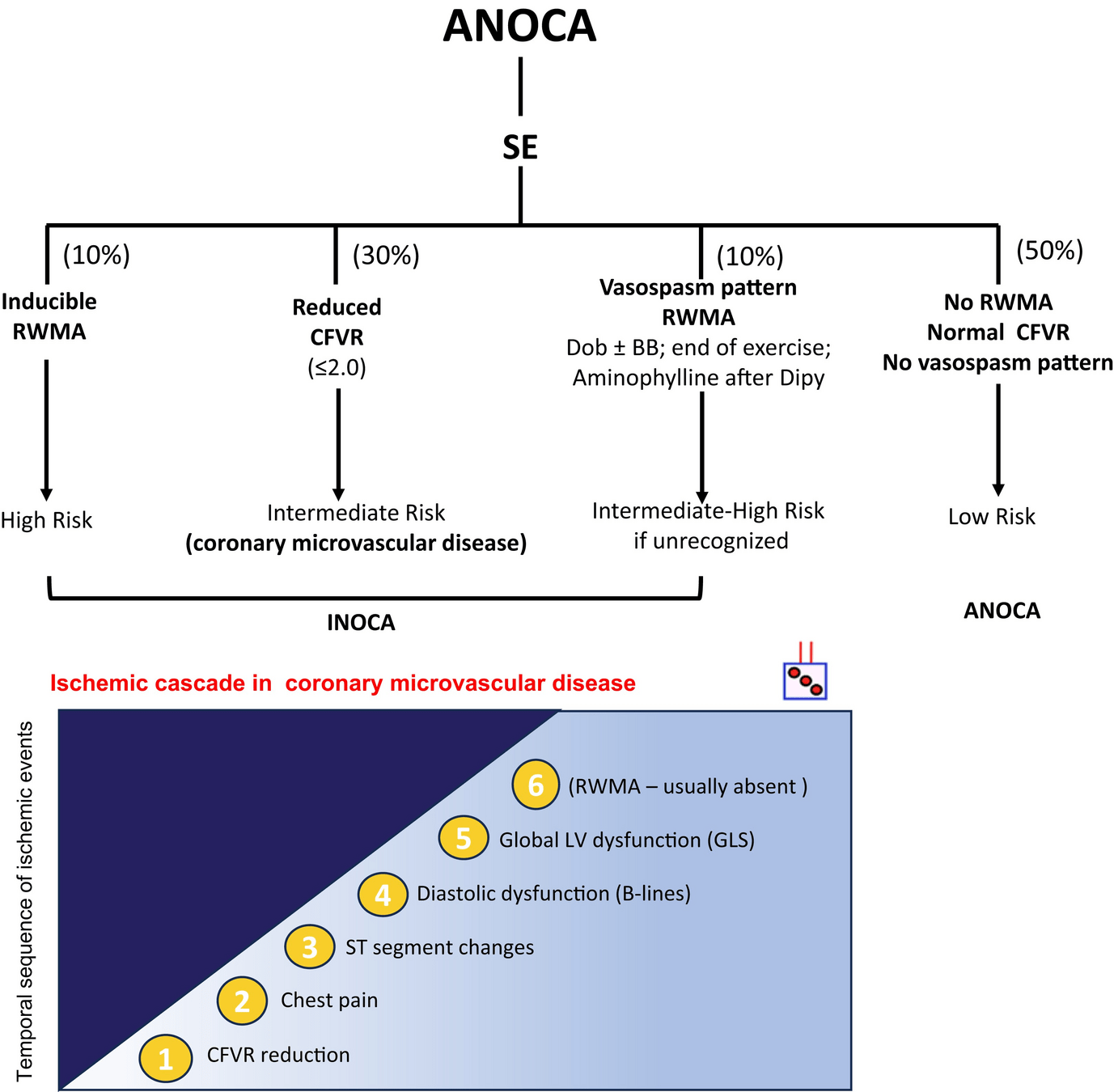
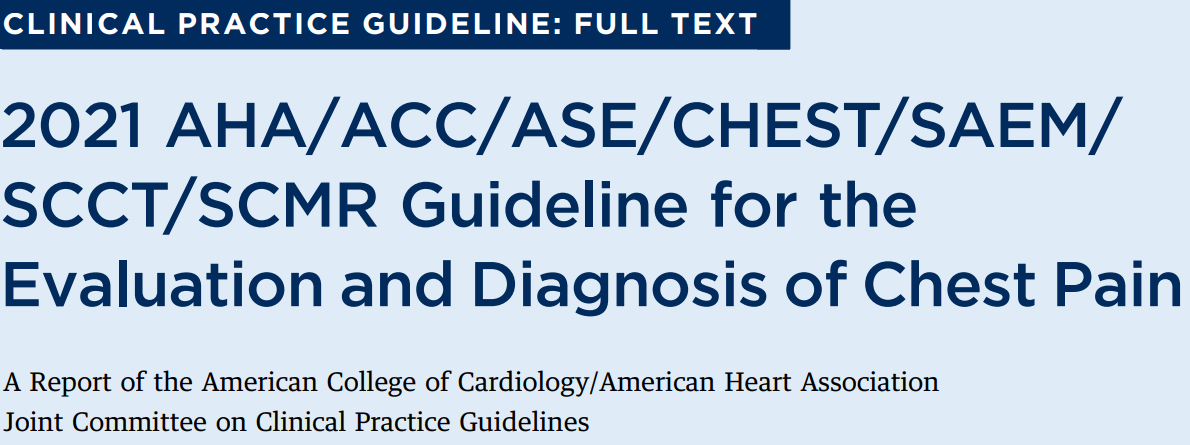
- WMA based protocol less useful in evaluating INOCA (ischemia with no obstructive CAD)
- Functional testing thus may not pick up non-obstructive clinical atherosclerosis that can cause future events
Rest
Post Exercise
LAD Ischemia
Why New Protocol?
- Change in referral pattern leading to a dropping positivity rate (<10% in some studies)
- Reduced predictive value
- Traditional stress echo protocol does not capture other areas of vulnerability in a heterogeneous population beyond identifying obstructive CAD
- ie. lung water, LV contractile reserve, coronary microcirculation and cardiac autonomic dysfunction
- New parameters are able to be implemented in Echo Labs without new technologies/sofware
ABCDE-SE Protocol
ABCDE-SE Protocol
A - Wall motion abnormalities, volumes*
B - B Lines
C - Left ventricular contractile reserve*
D - Coronary flow reserve
E - Heart rate reserve*
*do not require additional imaging based on current protocol
ABCDE Stress Echo
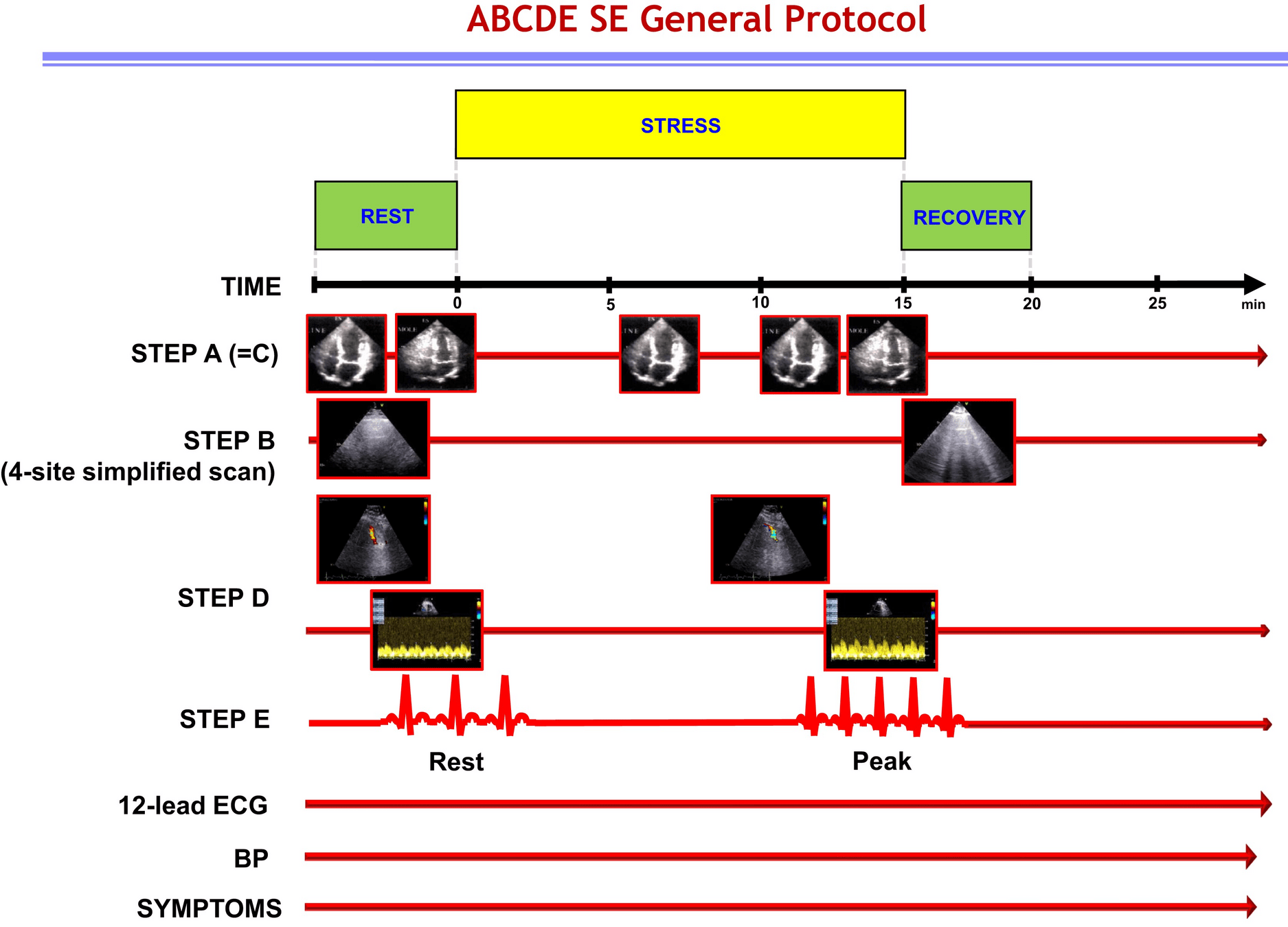
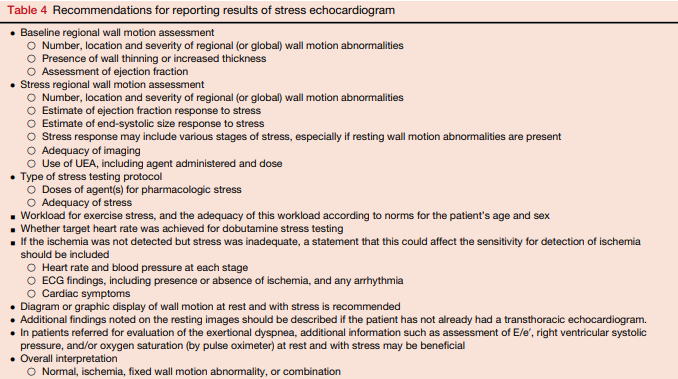
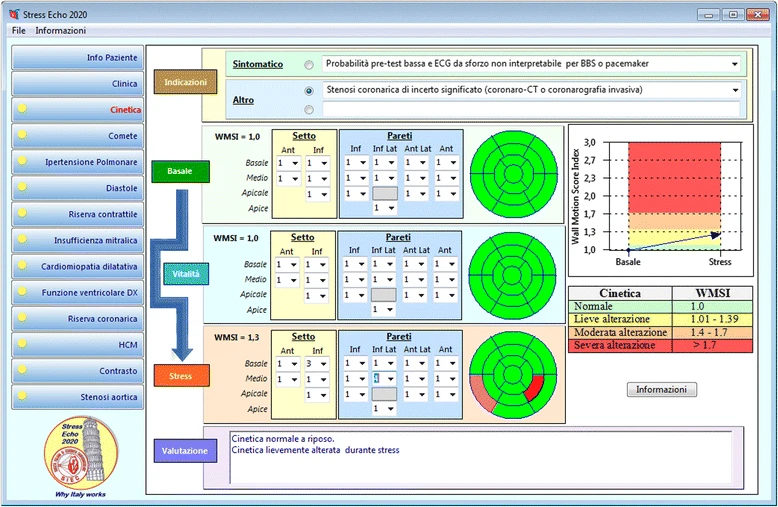
Step A: Myocardial Ischemia
- Assessment: Wall motion score index, 1 (normal) - 4 (dyskinetic) in a 17 segment LV model
- Positivity: 2 adjacent segments of same vascular territory increment by at least 1 point
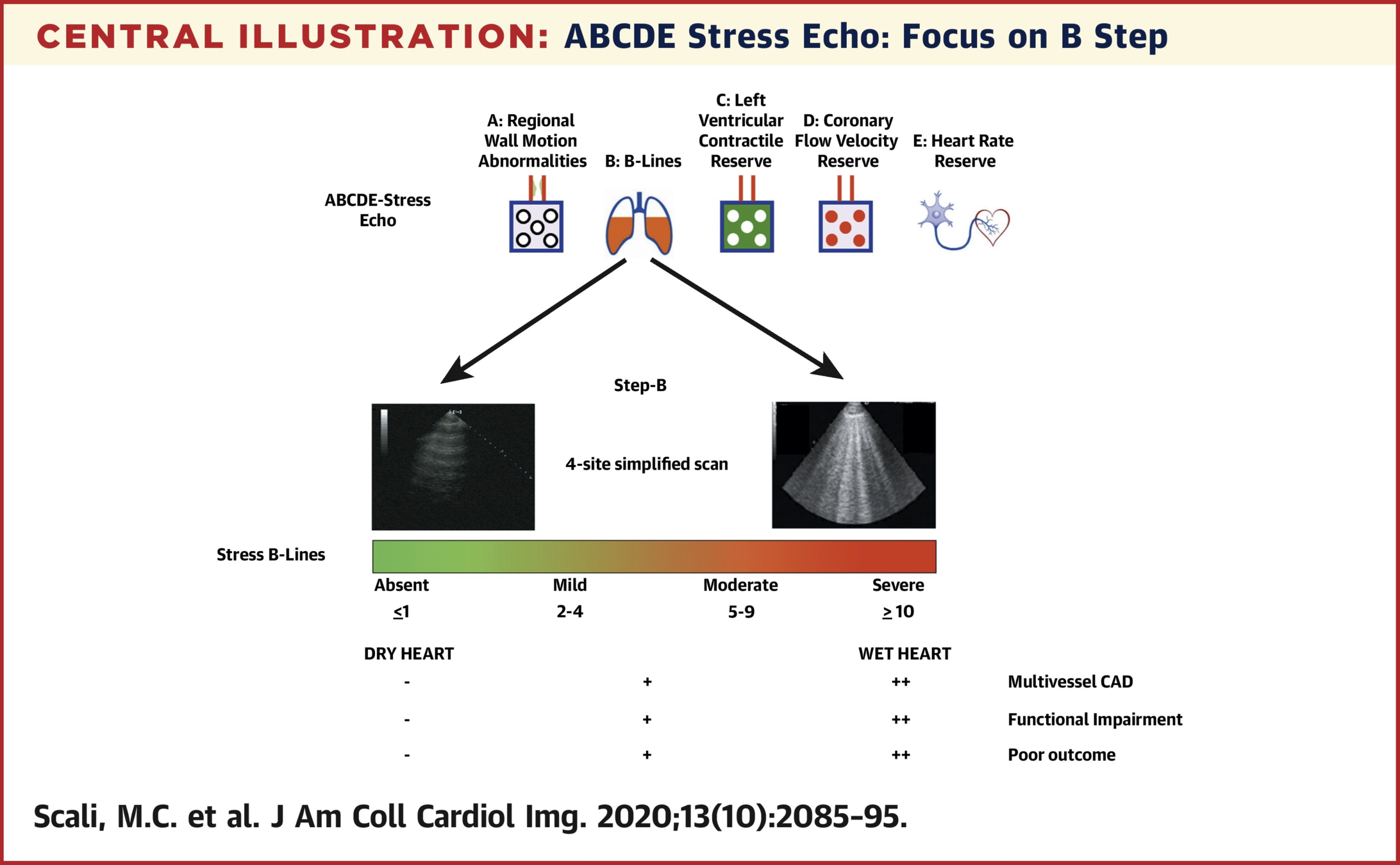
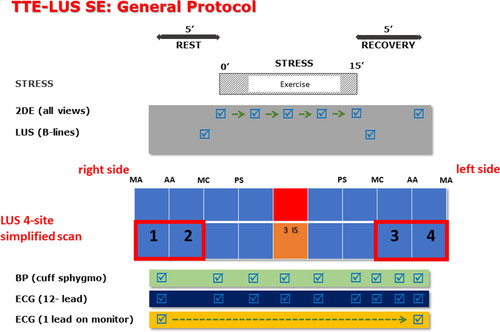
Step B: B Lines
- Assessment: 4 quadrant lung ultrasound for b lines
- Positivity: 2 or more
- Cardiac transducer
- Perpendicular to ribs
- 18cm depth
- 6s clips
- 3 Intercostal space
- Mid-Ax, Mid-clavic
Step B: B Lines
Scali MC, et al. (2020) Lung Ultrasound and Pulmonary Congestion During Stress Echocardiography. JACC Cardiovasc Imaging 13:2085-95.
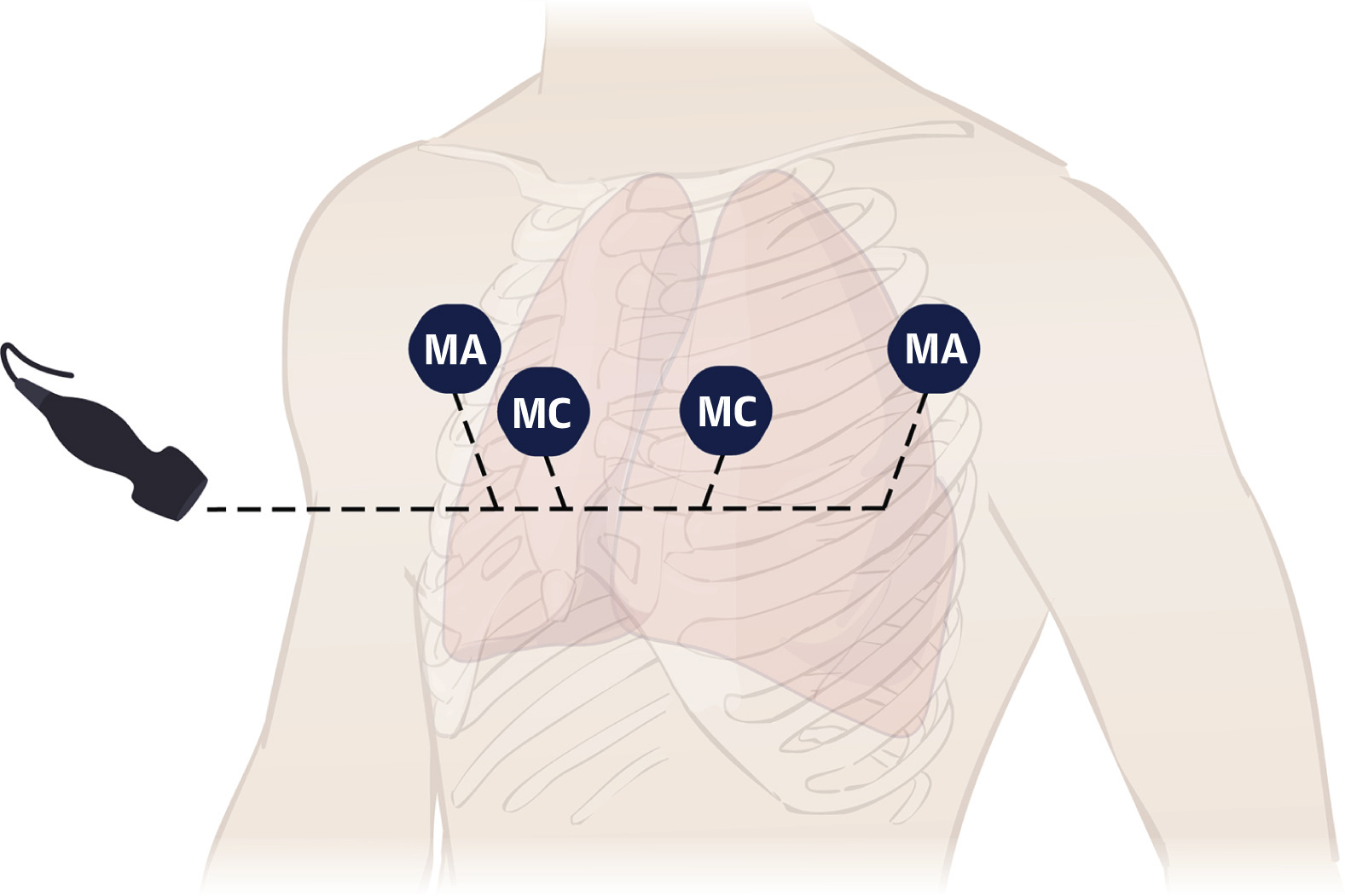
Example Acquisition
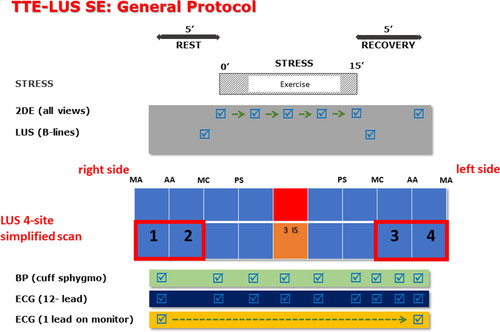
Picano E, et al.. Stress lung Ultrasound stress echo2020.2019. Available at https://www.youtube.com/watch?v=BwzgoG15E_A
Scoring Patients
Scali MC, et al. (2020) Lung Ultrasound and Pulmonary Congestion During Stress Echocardiography. JACC Cardiovasc Imaging 13:2085-95.
- 4 zone protocol
- Score each zone from 0-10 B-lines and sum 4 zones
- Report total at rest and stress and interval change
- Stress B-lines are categorized as:
- absent (score points 0 to 1), mild (2 to 4), moderate (5 to 9), and severe (=10 points)
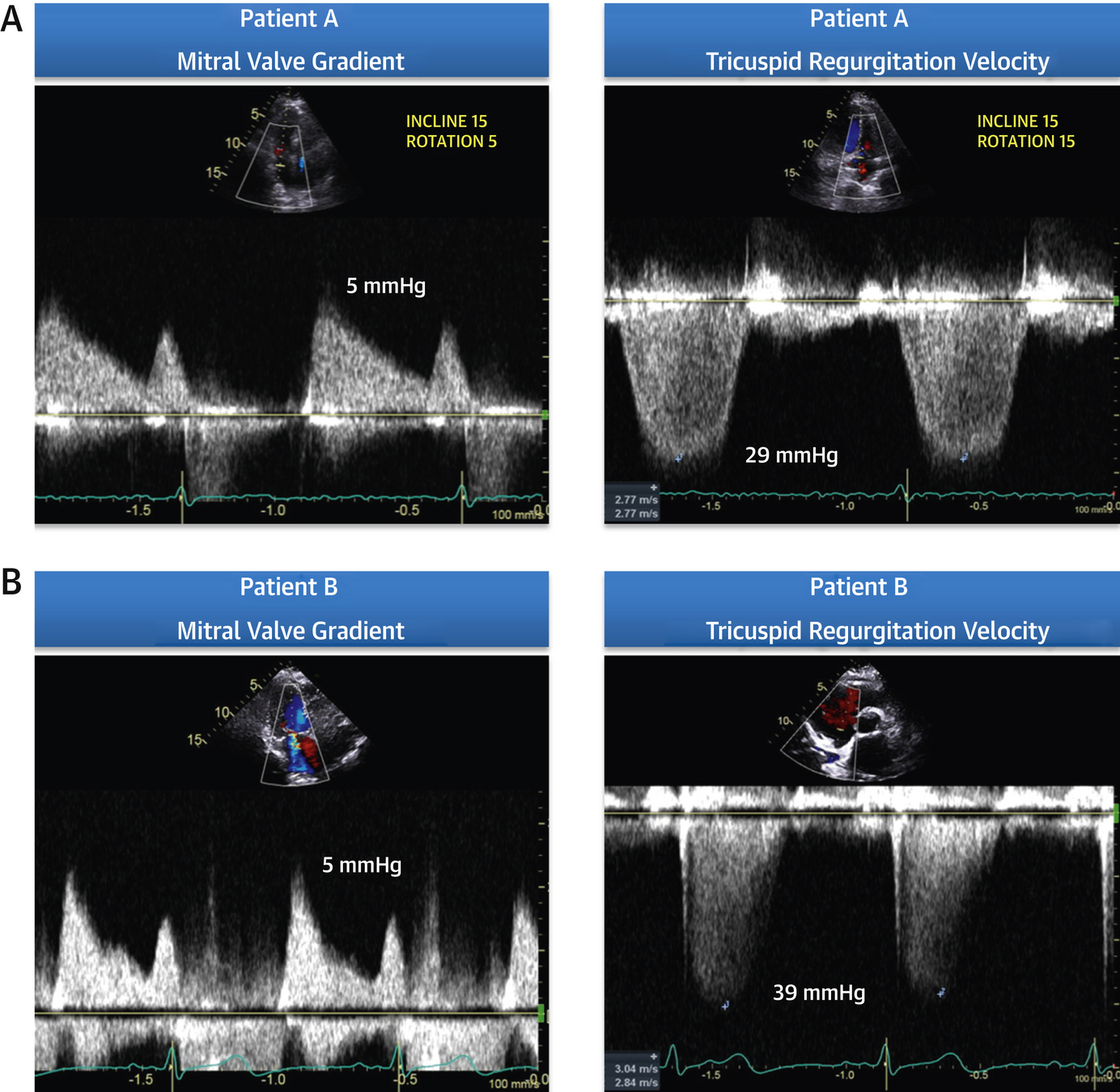
Case
- RFR: dyspnea
- 58-year-old female
- PHT 141 ms, MVA 1.6 cm2 (Mod MS)
- Mild to moderate regurgitation
Wiley BM, et al. (2020) Lung Ultrasound During Stress Echocardiography Aids the Evaluation of Valvular Heart Disease Severity. JACC Cardiovasc Imaging 13:866-72.
Case
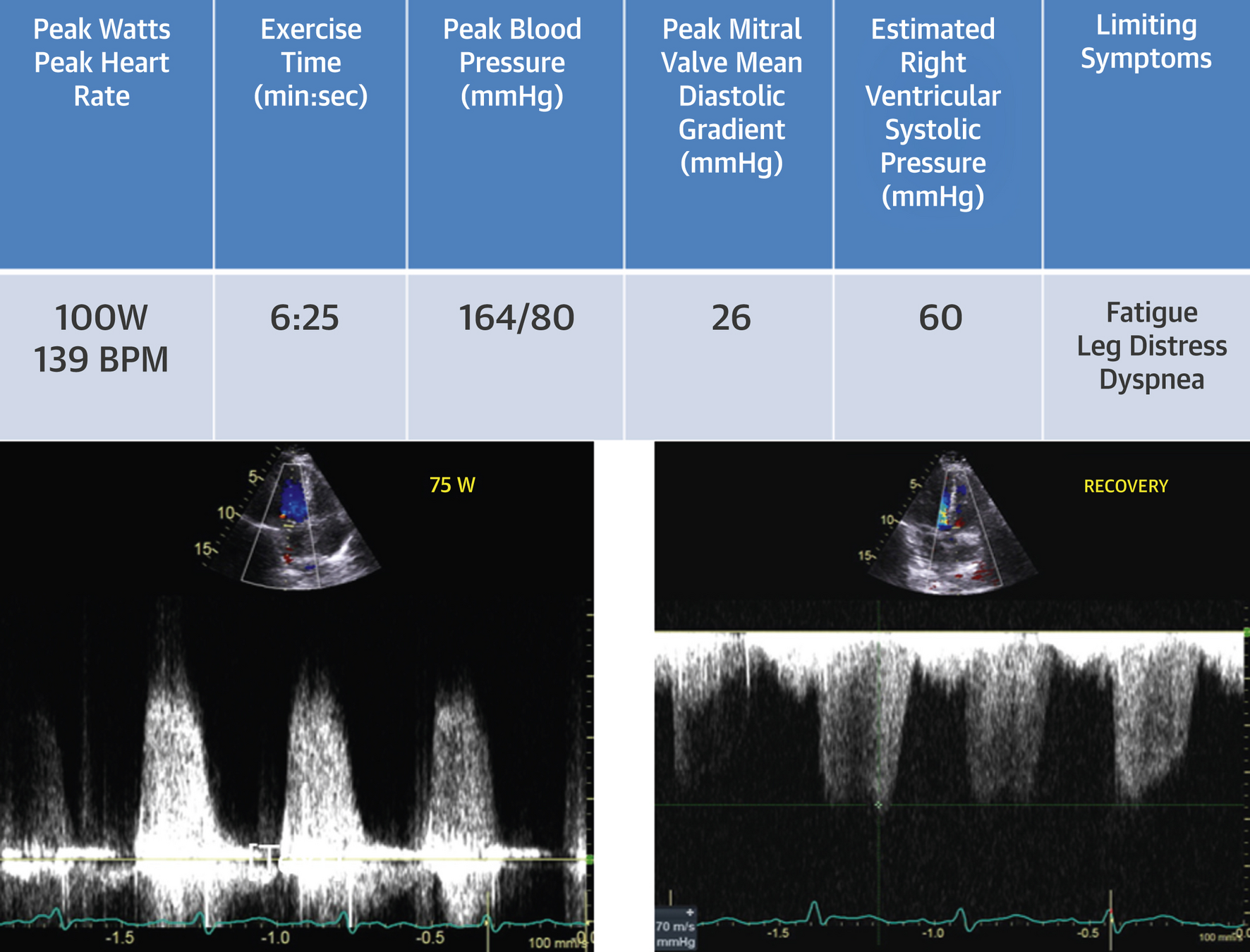
Wiley BM, et al. (2020) Lung Ultrasound During Stress Echocardiography Aids the Evaluation of Valvular Heart Disease Severity. JACC Cardiovasc Imaging 13:866-72.
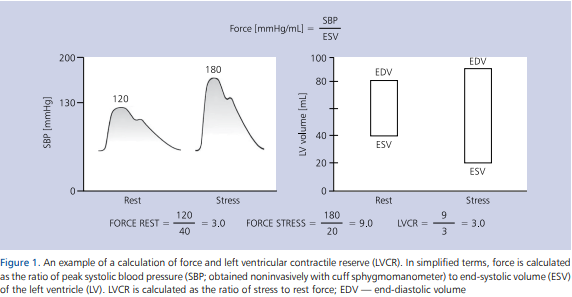
Step C: LVCR
- Assessment: Left ventricular contractile reserve is calculated as systolic blood pressure/end-systolic volume
- Positivity: LVCR < 2 for exercise/dobutamine or <1 for vasodilators
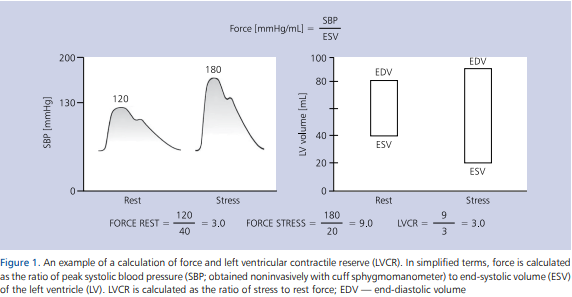
Step C: LVCR
- Lower number is worse (<2 for exercise or dobutamine)
- Combines two prognostic variables
- SBP not rising (or decreasing)
- ESV not decreasing (or increasing)
- Creates a unitless variable that is not load dependent
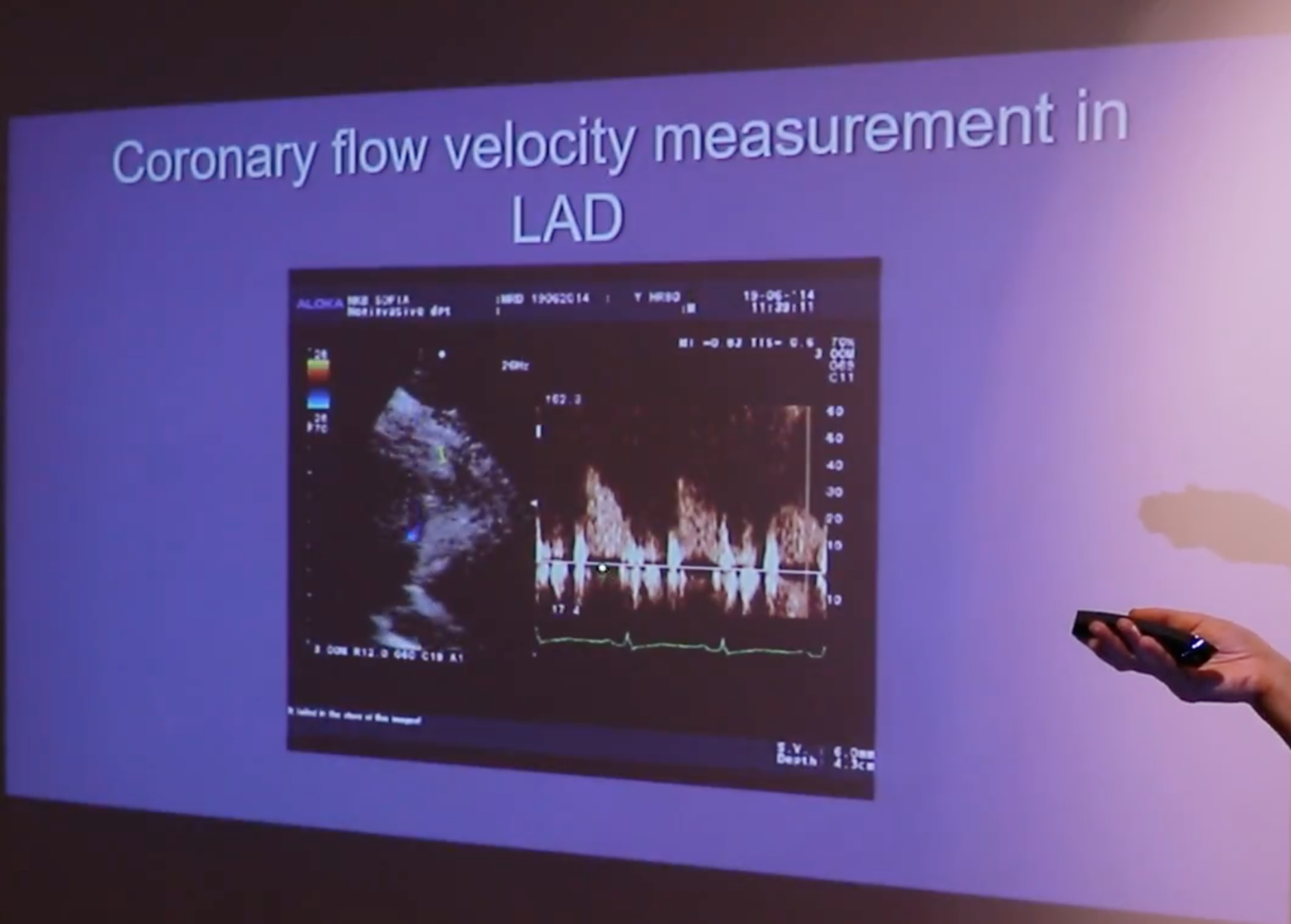
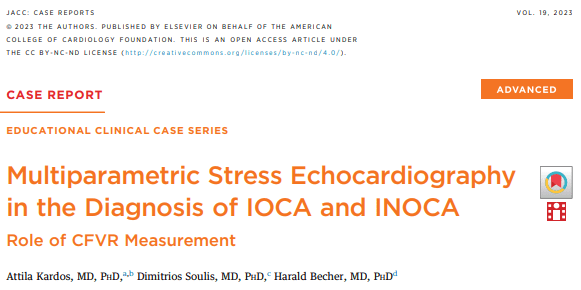
Step D: CFVR
- Assessment: Coronary flow velocity reserve of mid-distal LAD
- Positivity: CFVR < 2
- Success rate of 88% in obtaining CFVR on LAD (3000/3410)
- 80% with exercise (bike) and 81% with dobutamine
- Acquisition and Interpretation in < 4 minutes
- Assesses both epicardial CAD and coronary microcirculation
- Dopplers obtained and reviewed offline
- *Note: Stress Echo 2030 protocol, pharm SE or if exercise, then given adenosine bolus at end of recovery to assess CFVR
Step D: CFVR
- Acquisition: modified low parasternal and apical views
- Studies agree, onerous, but with training it is possible
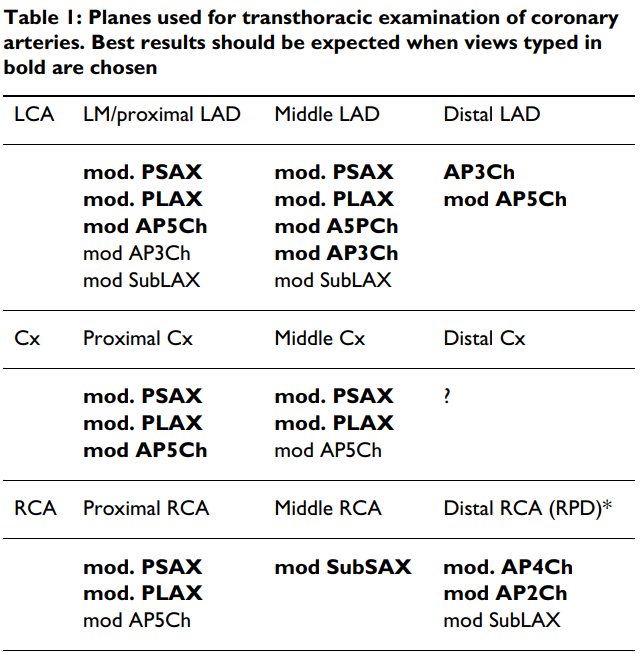
Step D: CFVR
- Acquisition: modified low parasternal and apical views
- Studies agree, onerous, but with training it is possible
Mod PSAX
Mod PLAX
Step D: CFVR
Step D: CFVR
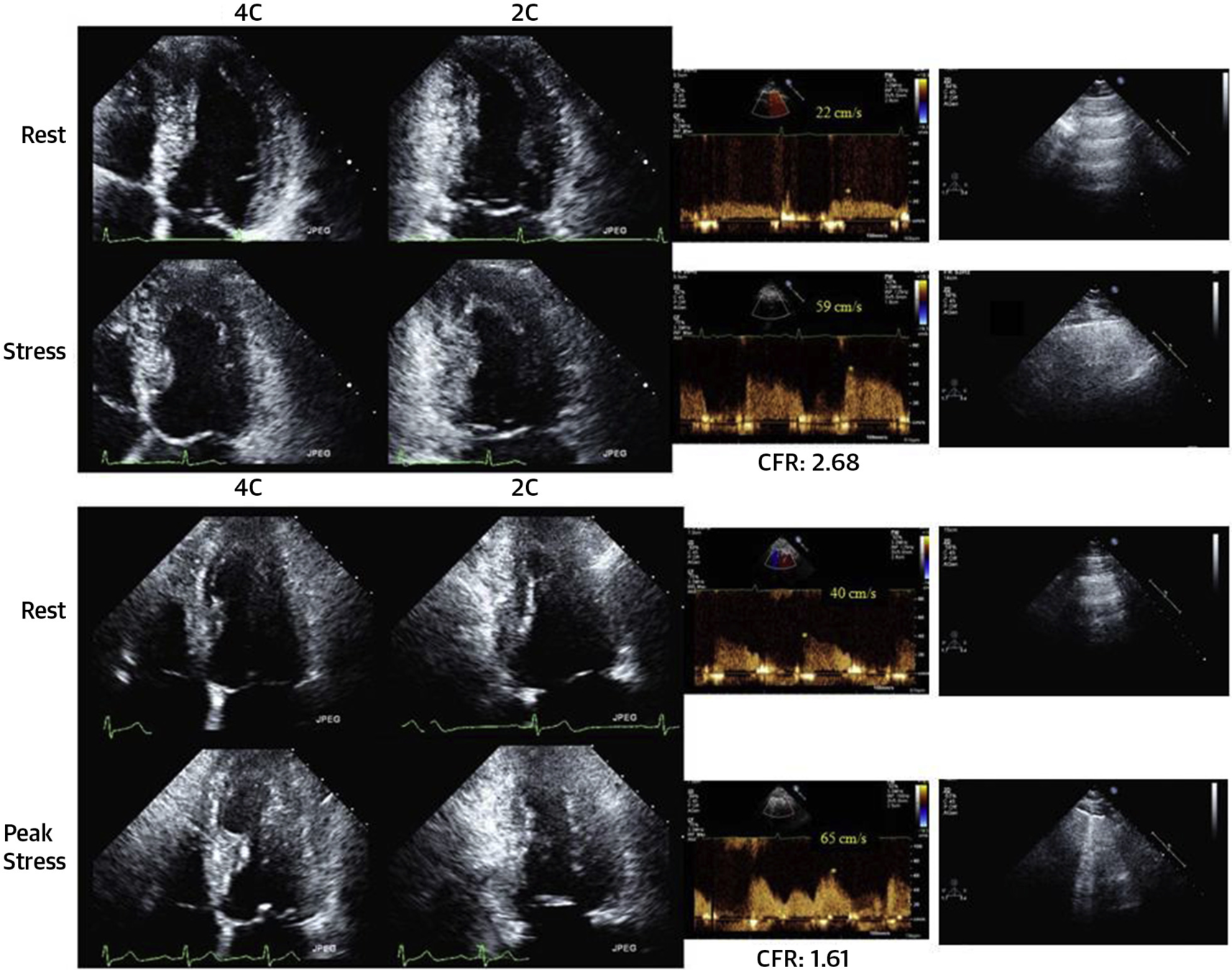
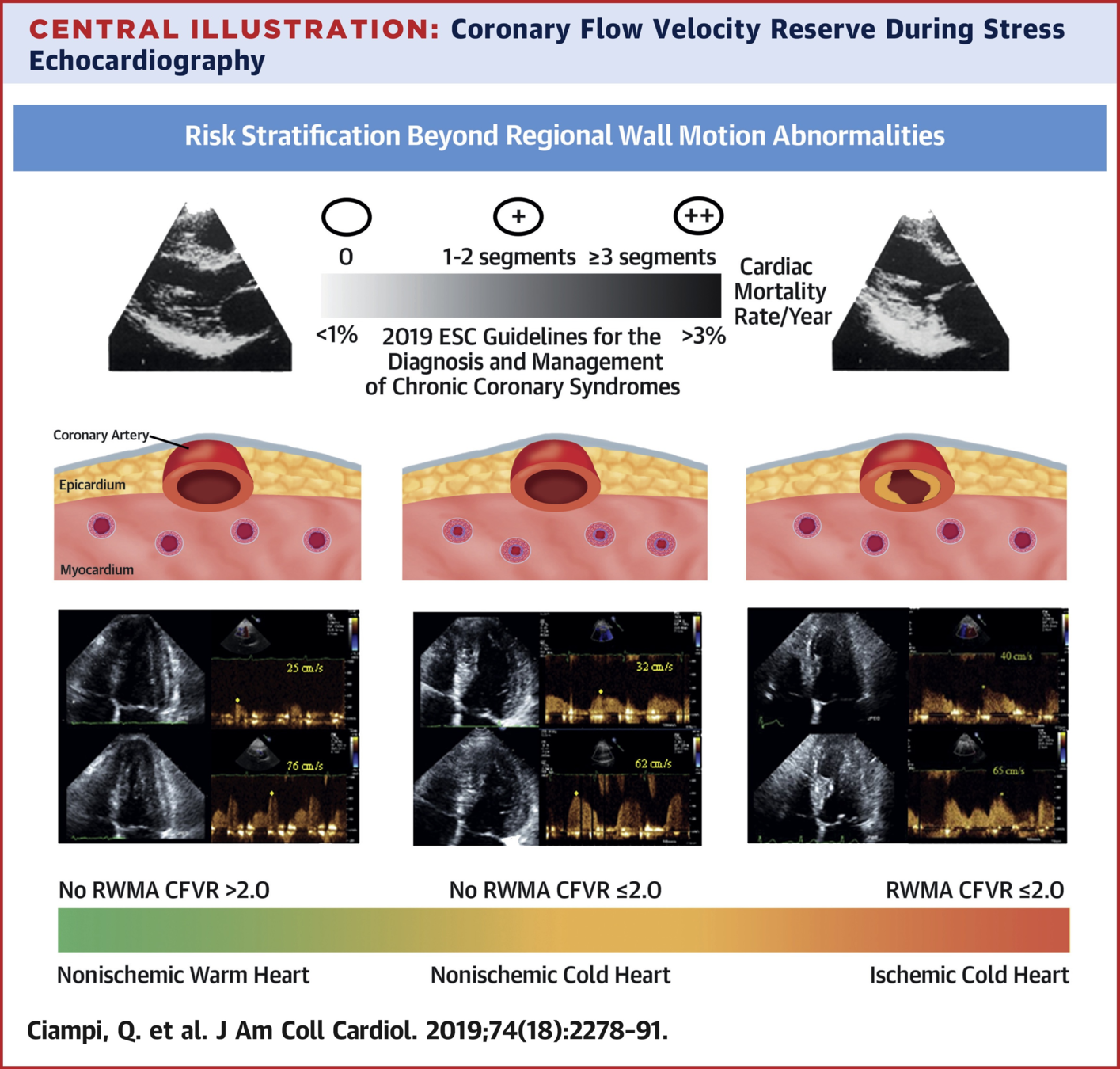
- Angina
- No WMA
- CFVR < 2
- Dx: chronic microvascular dysfunction
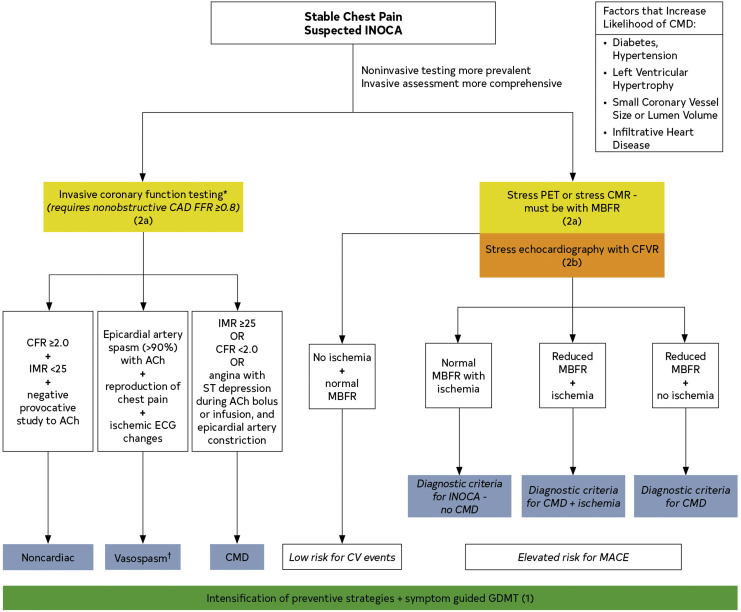
Step E: HRR
-
Assessment: Heart rate reserve =
- [(peak HR - rest HR) / (220 - age) - rest HR]
- Positivity: HRR <1.8 for exercise/dobutamine or <1.22 for vasodilator
- Previous studies show blunted HRR is a predictor or adverse events in vasodilator stress echo independent of inducible ischemia and beta blocker therapy
Example: Normal
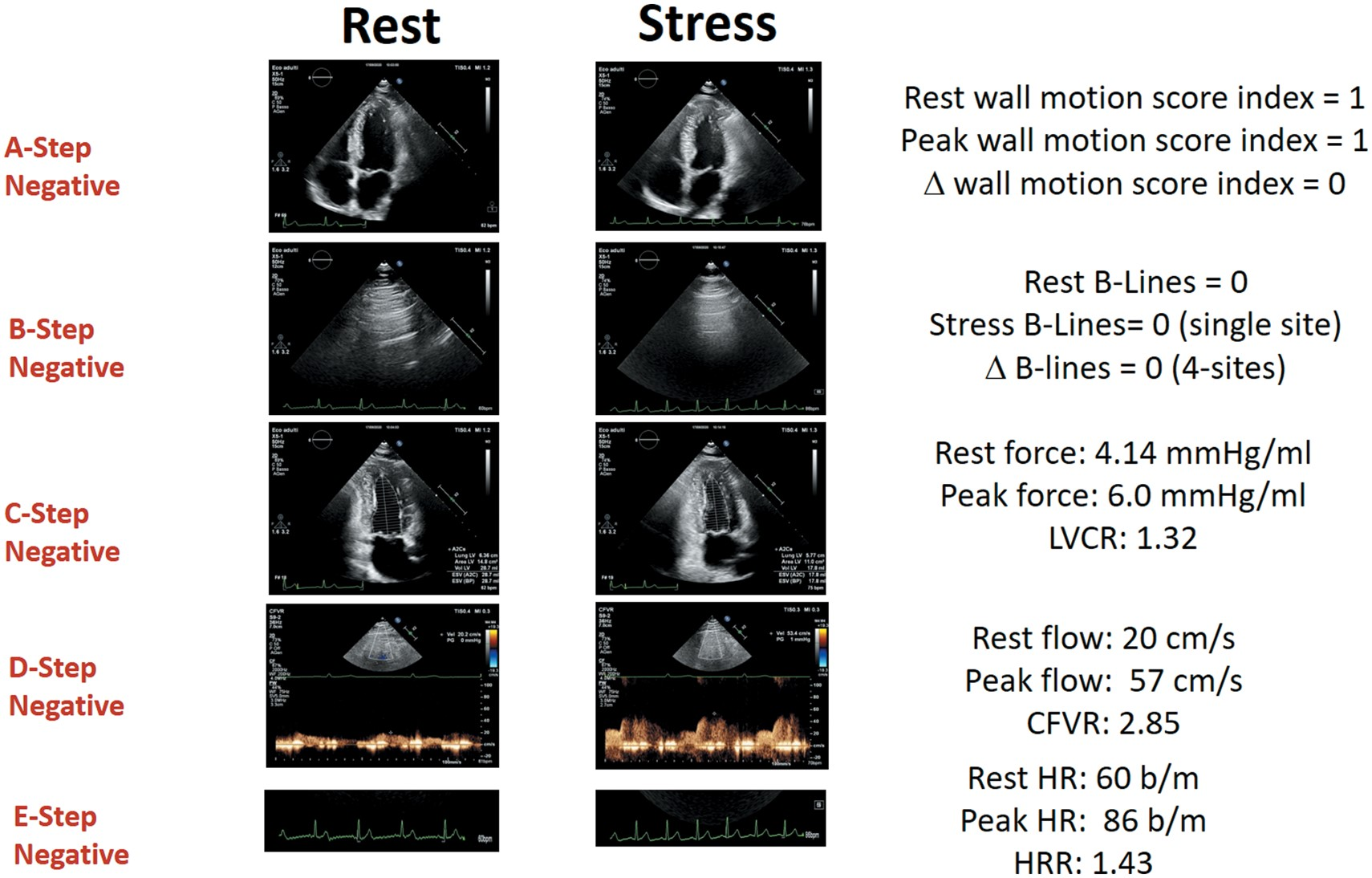
Example: Abnormal
Study
European Heart Journal 2021
Ciampi et al.
Prognostic value of stress echocardiography assessed by the ABCDE protocol
Design
- Design: prospective, multi-centre, international, effectiveness study
- Intervention: ABCDE stress echo protocol
- Patients: known or suspected chronic coronary syndrome
- Outcomes: All cause death
Inclusion/Exclusion
- age >18 years
- referral for known or suspected CAD
- no severe primary valvular or congenital heart disease, or presence of prognosis-limiting comorbidities, such as advanced cancer, reducing life expectancy to <1 year
- echocardiography of acceptable quality at rest and during stress
Results
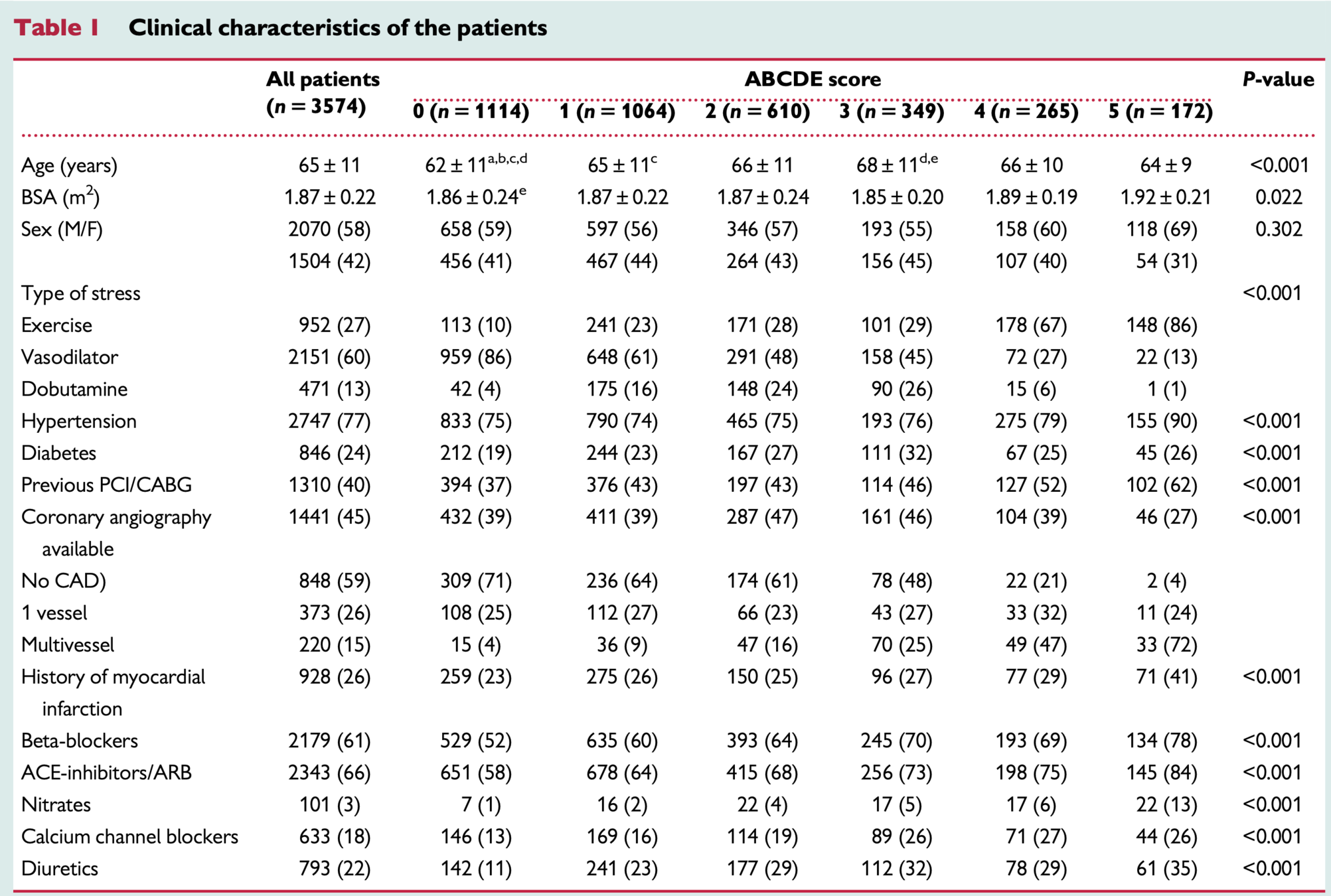
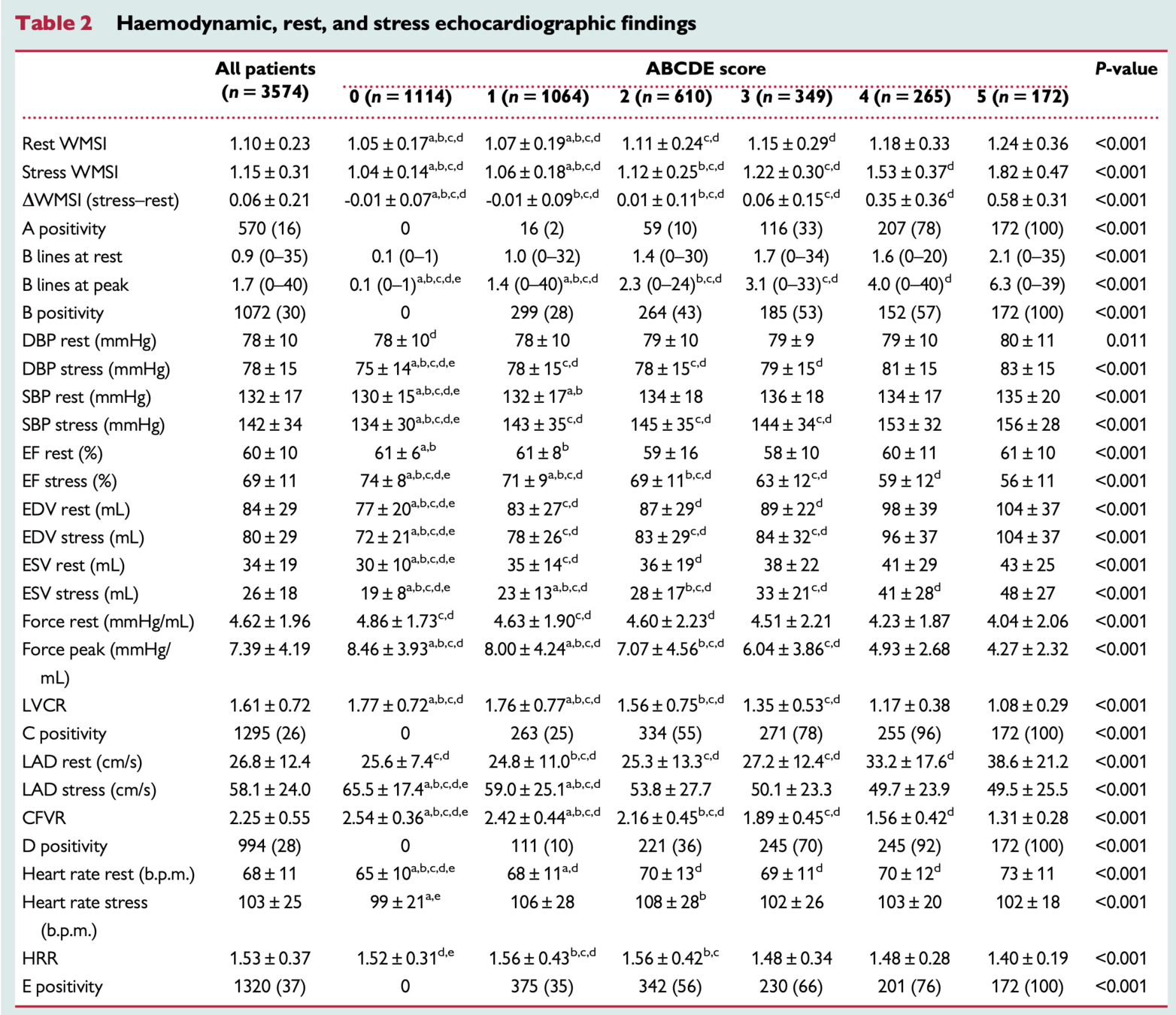
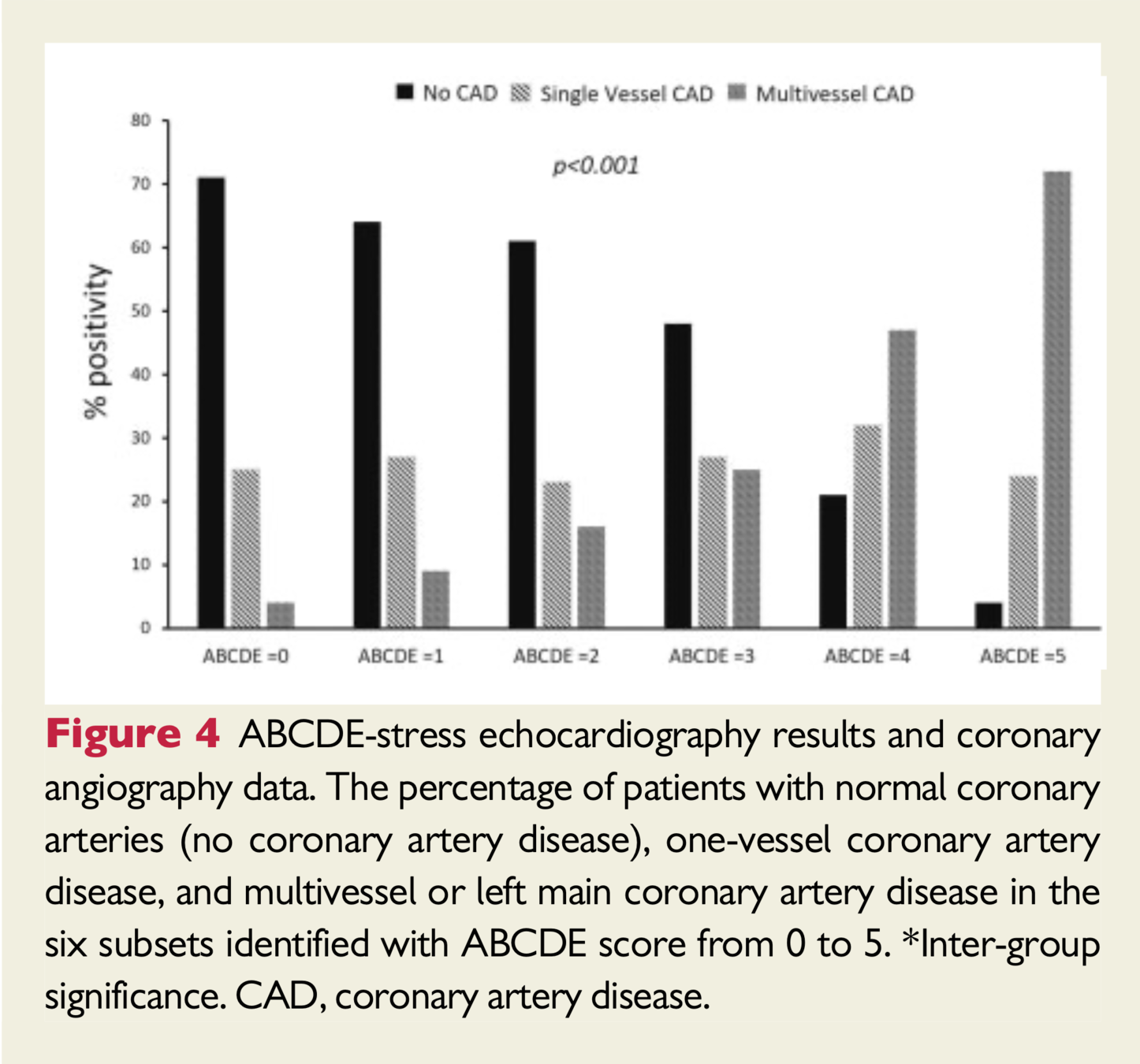
- Of those with normal SE who underwent coronary angiography, 30% demonstrated obstructive CAD, whereas in those with all five abnormal steps on SE, 95% had significant CAD.
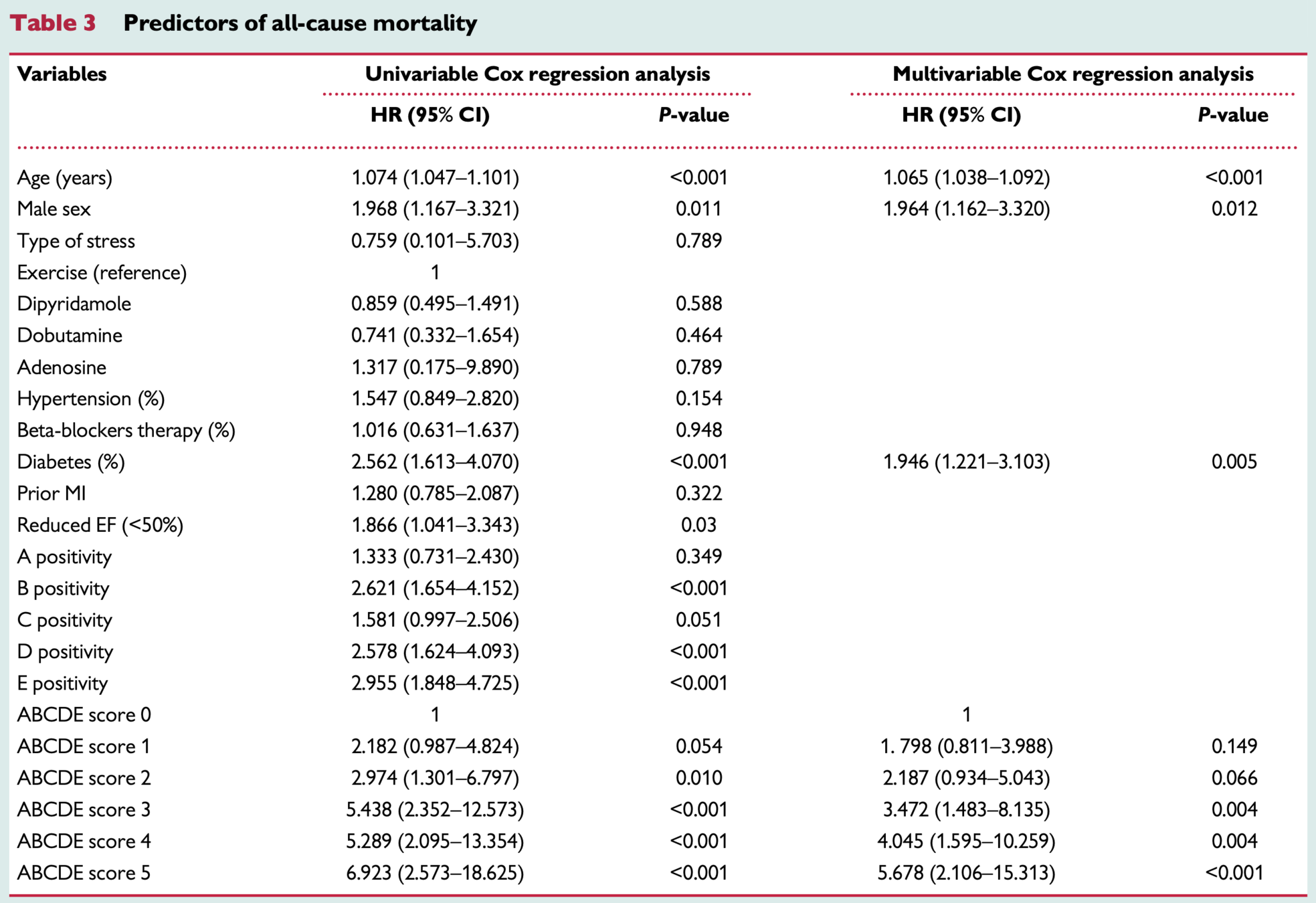
Predictors of Mortality
-
Postive:
- B-lines
- Coronary flow velocity reserve
- Heart rate reserve
- ABCDE Score 3 or greater
-
Negative:
- Regional Wall Motion Abnormalities
- Left ventricular contractile reserve
- The mortality rate was 0.4%/year for a normal SE compared with 2.7%/year when all SE steps were abnormal.
Incremental Benefit
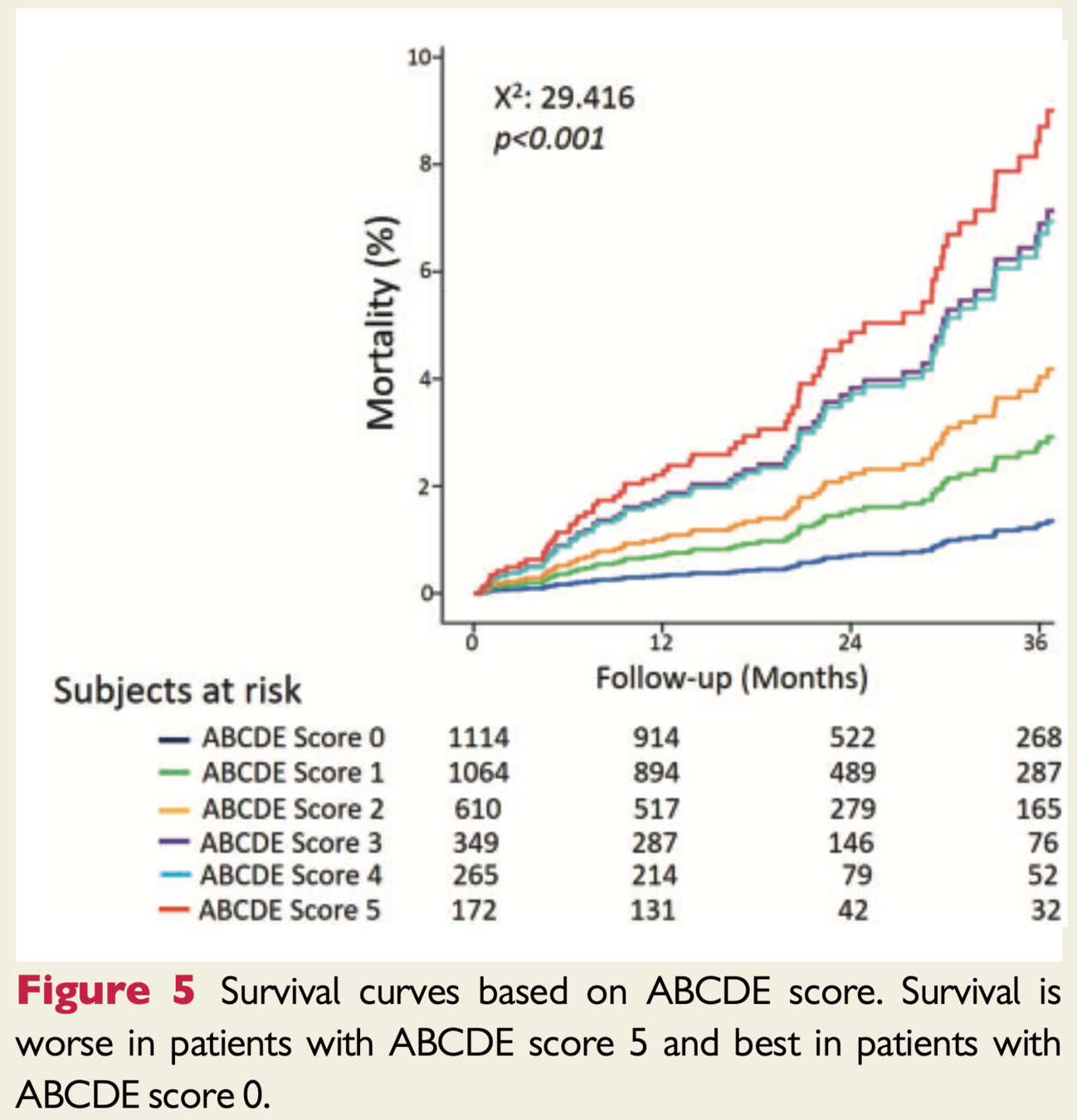
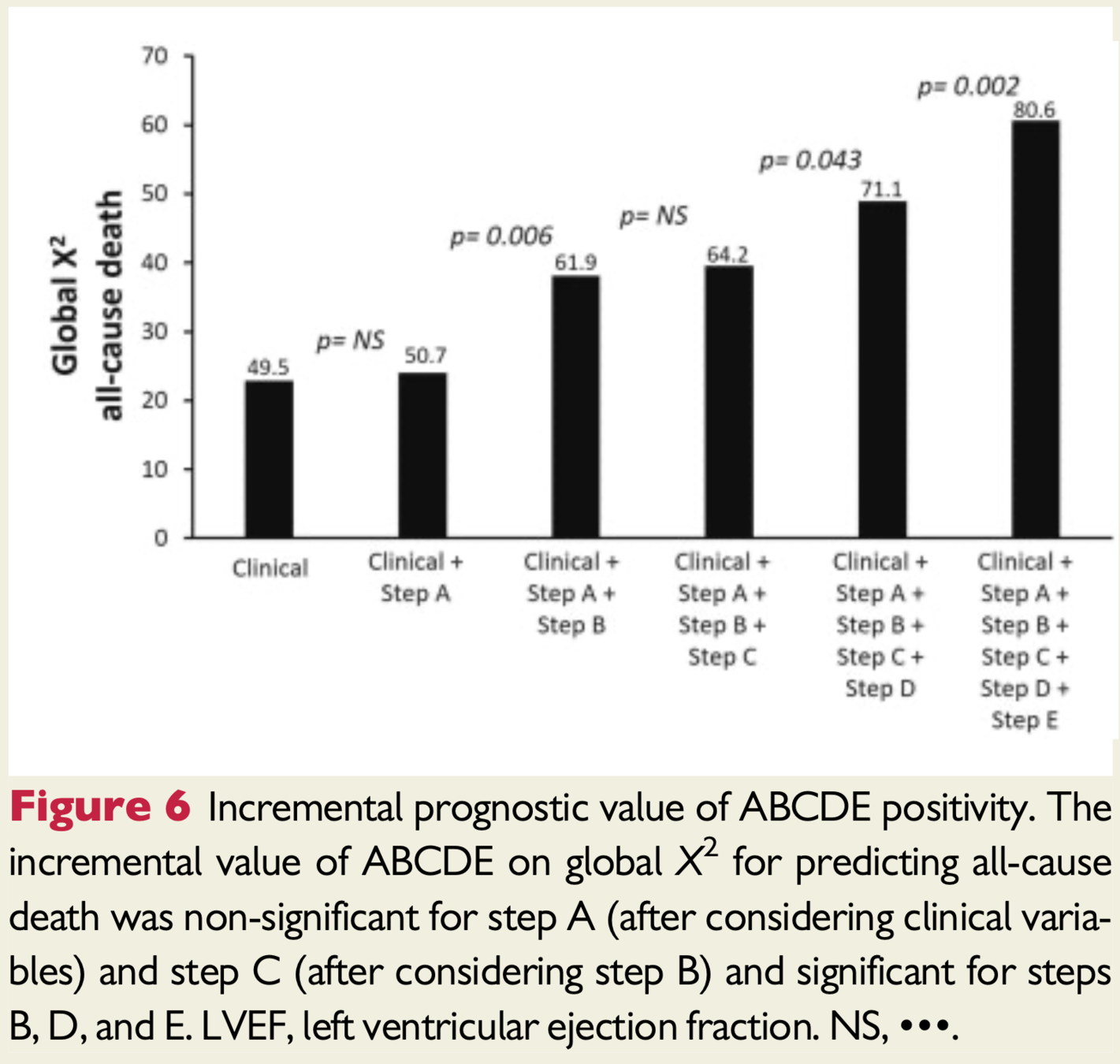
Study Conclusions
- Higher ABCDE score predicts less benign outcome
- Regional wall motion abnormalities, most used measure, less helpful in predicting prognosis
- Steps B-E are feasibly added to current stress echo protocols
- Shift assessing only coronary stenosis to patient as a whole
- Other vulnerabilities including coronary microvascular dysfunction and autonomic dysfunction
Study Conclusions
- Consider targeting treatments towards the identified abnormal steps
- Stress echo low cost/risk/environmental impact and no radiation
- ABCDE protocol can be used with any stress - exercise or pharmacological (ie. in a global pandemic pharm preferred)
Proposed Tailored Therapy
- Step A identifies inducible ischemia --> BB/CCB/nitrates or possible revasc
- Step B identifies pulmonary congestion --> diuretics
- Step C (LVCR) identifies LV dysfunction --> ACEi
- Isolated Step D identifies microvascular dx --> statin
- Step E abnormalities can be targets by neurohormonal modulation (ie. BB/ACEi/MRA/renal denervation)
Treatments potentially titratable to ABCDE risk score
Discussion
Discussion
- Dedicated training required to implement protocol
- Specifically coronary flow of LAD is most challenging
- Originally planned 5000 patients and 3 year followup but achieved ~3600 and 21 month followup
- 2020 was planned last year of study but COVID
- No other end points other than mortality to assess predictive power of protocol steps
- Ie. B-lines and HF admissions
Discussion
- Images were not reviewed by core lab
- Practical for effectiveness study as has real-world applicability
- Parameters were binary, positive or negative, future studies plan to consider mild-mod-severe stratification
- Most patients underwent dipyridamole stress, would be beneficial to compare predictive value of the steps by stress modality (could explain why physiological measures such as LVCR were not predictive)
- High score 4-5 were mostly in exercise group
Discussion
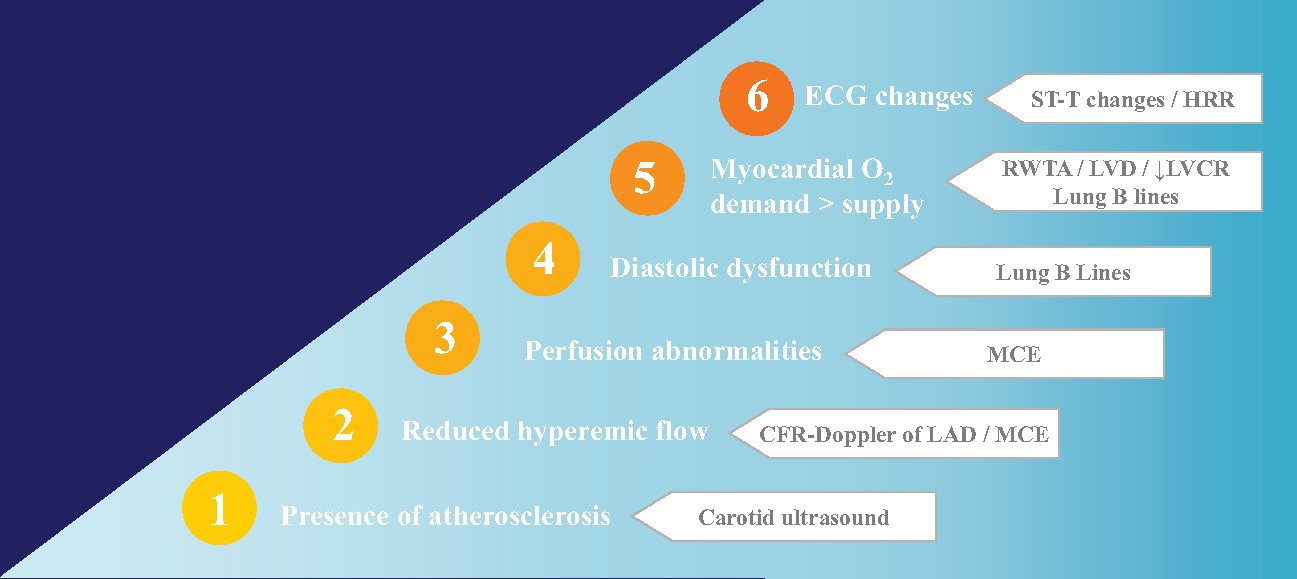
- RWMA may not be a strong enough tool to assess for ischemia as significant oxygen supply demand mismatch is needed
- Future protocols could employ myocardial contrast echocardiography to assess perfusion
- Low usage of contrast in general in the study
- Functional testing may not pick up non-obstructive lesions which can still lead to to events
- Critics recommend carotid ultrasound to pick up on clinical atherosclerosis
Where now?
Modified ABCDE?
ABCDE+
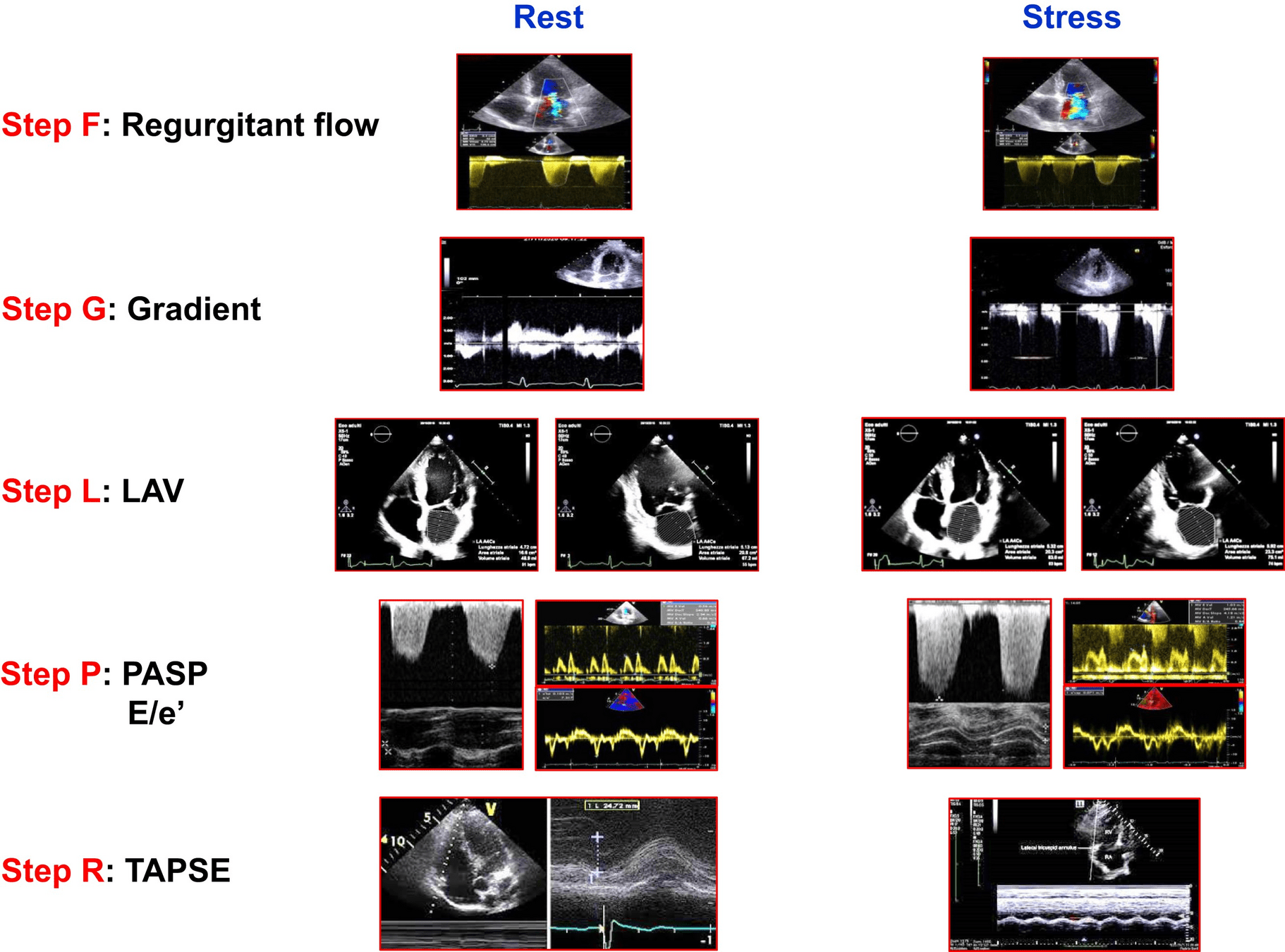
ABCDE + F (regurgitant flow) G (LVOT gradients) L (left atrial volume/function) P ( pulmonary and LV pressures) L (RV function)
Stress Echo 2030

ABCDE + F (regurgitant flow) G (LVOT gradients) L (left atrial volume/function) P ( pulmonary and LV pressures) L (RV function)
Stress Echo 2030
- 1-SE in coronary artery disease (SECAD)
- 2-SE in diastolic heart failure (SEDIA)
- 3-SE in hypertrophic cardiomyopathy (SEHCA)
- 4-SE post-chest radiotherapy and chemotherapy (SERA)
- 5-Artificial intelligence SE evaluation (AI-SEE)
- 6-Environmental stress echocardiography and air pollution (ESTER)
- 7-SE in repaired Tetralogy of Fallot (SETOF)
- 8-SE in post-COVID-19 (SECOV)
- 9: Recovery by stress echo of conventionally unfit donor good hearts (RESURGE)
- 10-SE for mitral ischemic regurgitation (SEMIR)
- 11-SE in valvular heart disease (SEVA)
- 12-SE for coronary vasospasm (SESPASM)
Questions?
"The current shift toward using SE protocols with both known and novel parameters is a new frontier. It will be interesting to observe the impact of SE 2020 in shifting practice. There has been a reluctance to “go with the flow” on this side of the Atlantic, but perhaps this will change with clear demonstration of feasibility and incremental value of a multiparametric SE approach, especially in women, who could benefit greatly from a noninvasive, nonionizing assessment of myocardial microvascular integrity."
-Sharon L. Mulvagh (Editorial Comment)