Diagnosis and Management
of Atrial Fibrillation
Atul Jaidka
Disclosures
- None
Objectives
- Screening and opportunistic detection of atrial fibrillation
- Identifying and managing risk factors associated with atrial fibrillation
- Acute and chronic management of atrial fibrillation -stroke prevention, rate vs rhythm control, and catheter ablation
- Review current Canadian clinical practice guidelines
Classification
- Paroxysmal
- 30s - 7 days
- Persistent
- 7 days to 1 year
- Longstanding persistent
- 1 year or greater
- Permanent
- No longer pursuing rhythm control
- Primary vs Secondary (reversible vs provoked)
Burden
- Significant impact on quality of life
- Independently associated with increased risk of mortality
- Increased risk of stroke
- Generally worse outcomes compared to non-AF strokes
- SIgnificant health care utilization (ED, hospital, clinic, procedural)
Frame Shift
- Over past 5-10 years there has been a frame shift in the management of AF
- Treatment of AF as a part of a multi-system disease
- Earlier management is beneficial
- Growing evidence in certain populations on the benefit of maintaining sinus rhythm
Case
You are seeing a 68 year old male (Class I obesity, Hypertension, and diet controlled DM2) in clinic who presents with anxiety. His brother developed atrial fibrillation and he is wondering whether he should have screening. How should we approach screening in this patient?
Screening
Screening
- Reasons to screen
- AF is often asymptimatic
- 1/4 of patients with stroke are later found to have AF
- There is a need to balance screening with economic cost and potential harms
- Number needed to screen over 65 is 69 to yield 1 AF

- Number needed to screen over 65 is 69 to yield 1 AF
Kardia
- Many clinics don't have ECG cart
- Kardia is cheaper and faster and recommended in the AF guidelines
- <$100 from Costco/Amazon
- Takes 30 seconds to obtain a reading and can cross check the strips

Screening in Stroke
- Guidelines recommend at least 24 hours of ambulatory ECG monitoring
- Prolonged monitoring in select older patients if AF is still suspected
- Personal practise is for a 2 week patch ECG monitor
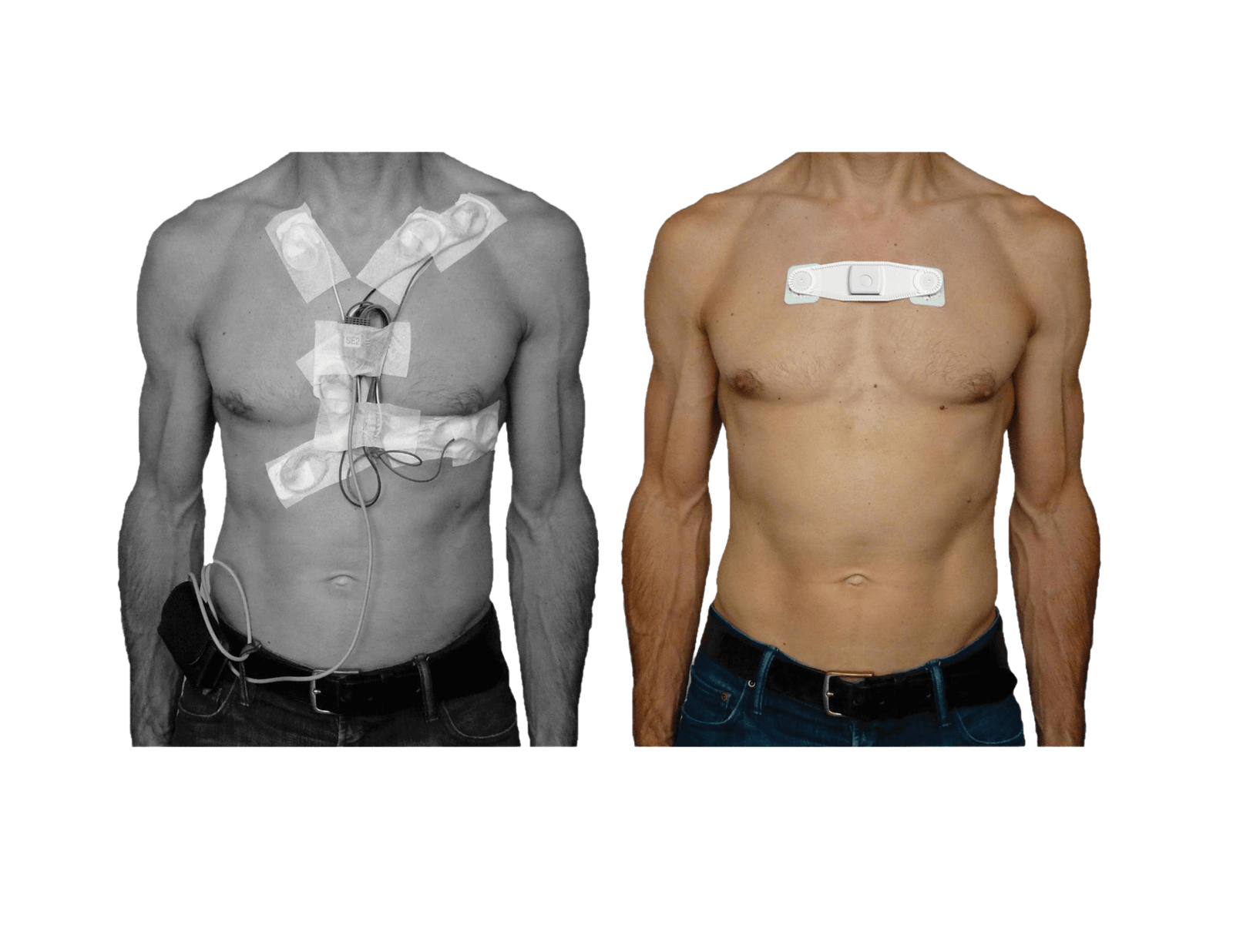
Kardia
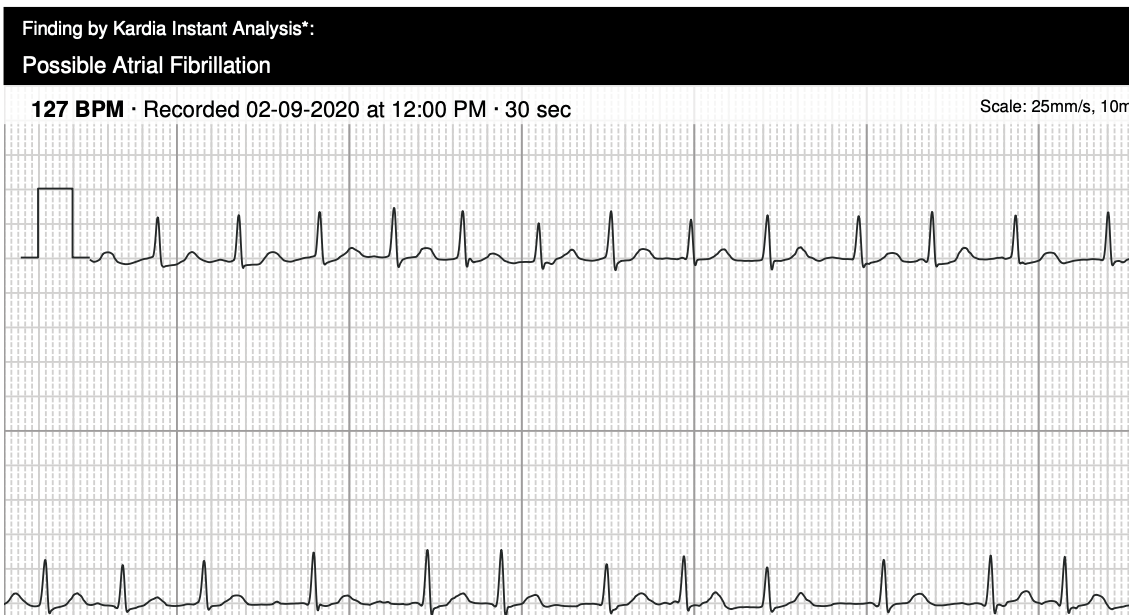
https://theskepticalcardiologist.com/
ECG
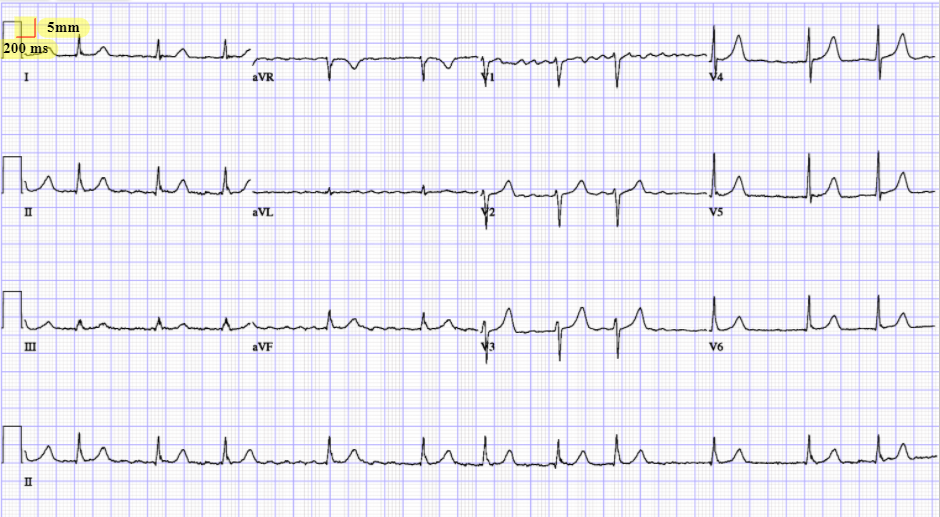
How should we work up this patient?
Initial Workup
- Complete Hx and Phx
- Includes all past history of AF and symptoms
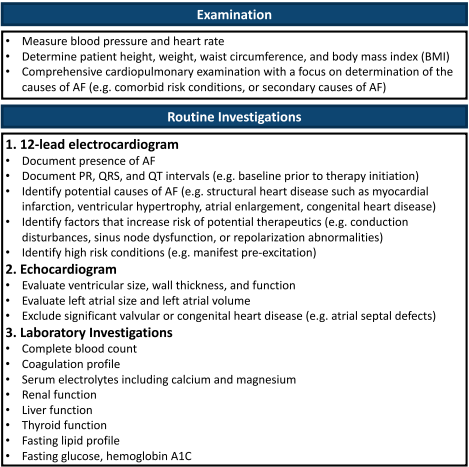
- Can use QoL Scale
- Identify RFs, triggers and secondary causes of AF
- ECG, TTE, Labs
- CBC, Coags, Lytes + Ca +Mg, Renal, Liver, Thyroid, Lipids, A1C
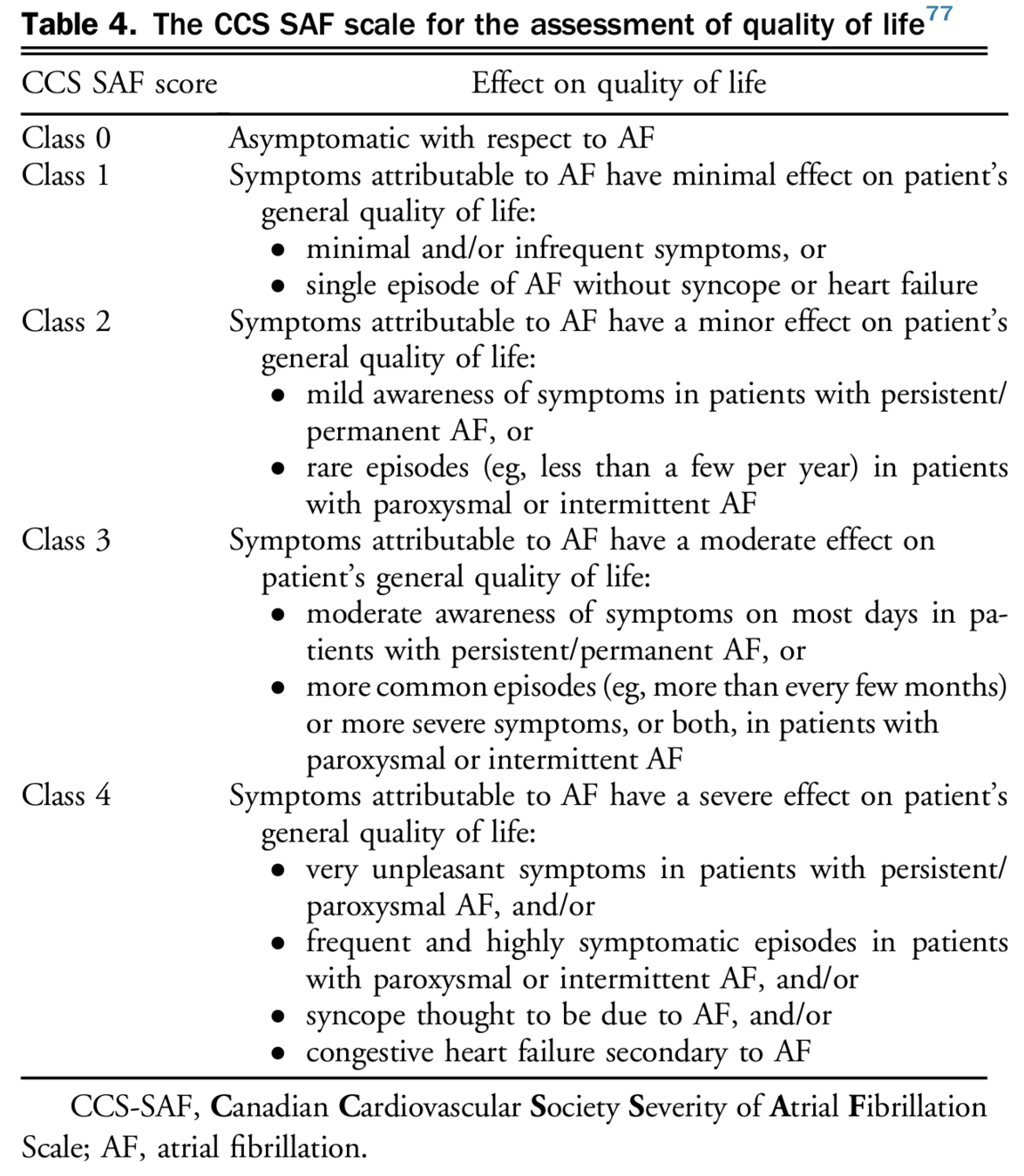
Workup
Case
What are risk factors for atrial fibrillation and how would you counsel the patient on modifying them?
Risk Factors
"HEAD 2 TOES"
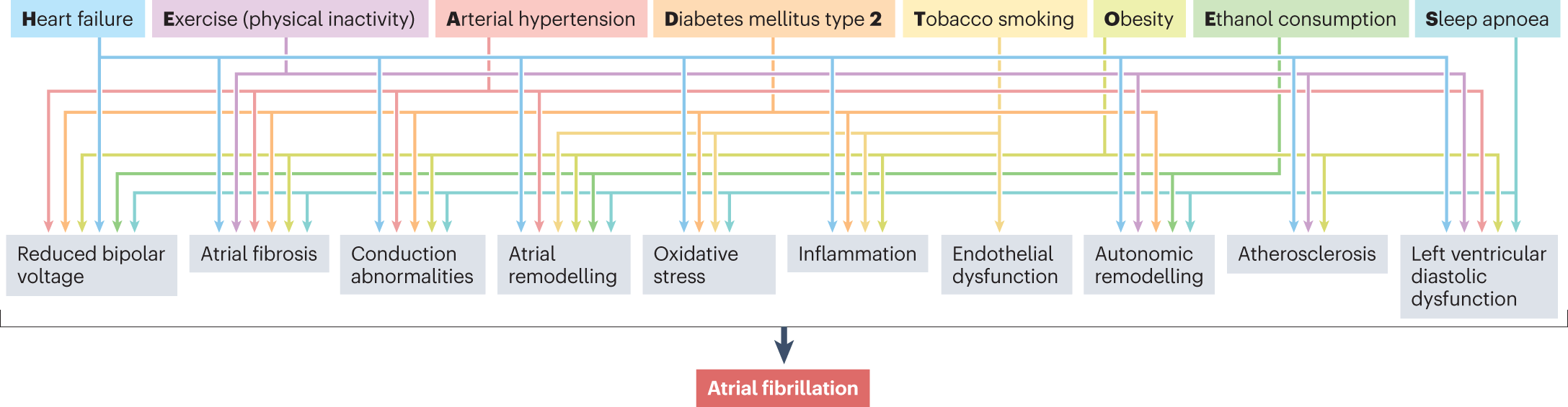
https://www.nature.com/articles/s41569-022-00820-8
Risk Factors
"HEAD 2 TOES"
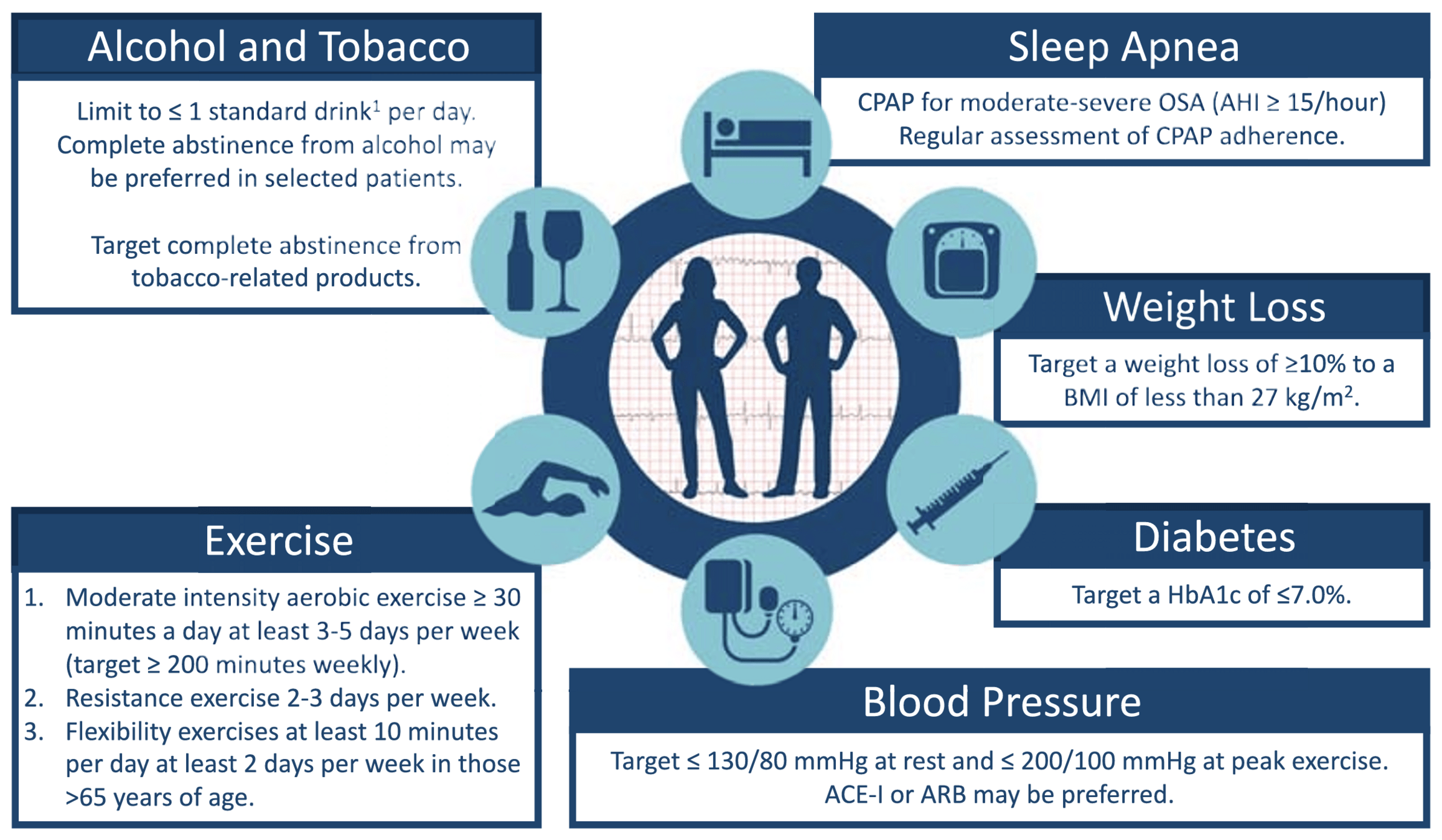
- AHA 2023: recommends againt abintence from caffeine (common question) unless it provokes symptoms
Case
We have initiated a multi-disciplinary risk factor modfication plan for the patient and now move to the stroke prevention and arrhythmia management. How should we manage this patient?
Stroke Prevention
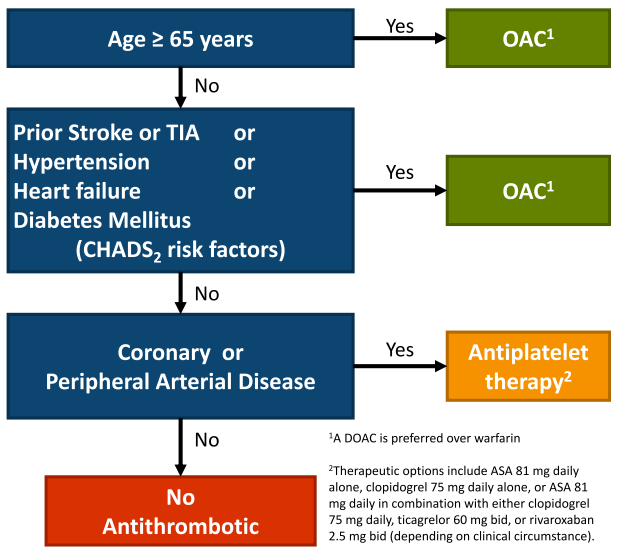
- Note: annual reassessment
- Warfarin: only for mechanical heart valves or moderate to severe mitral stenosis (valvular afib)
SPARCtool
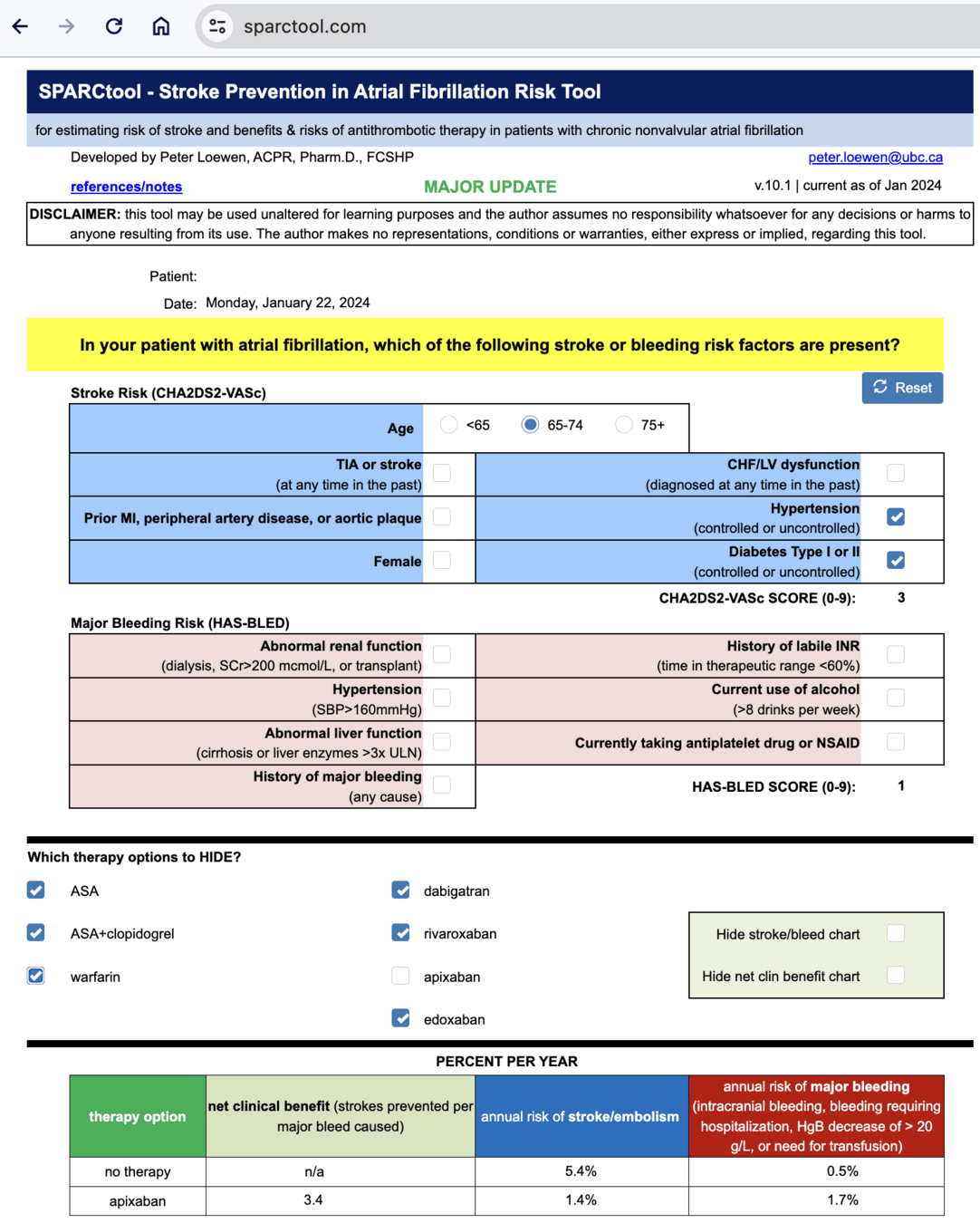
SPARCtool
SPARCtool
Special Circumstances
Renal Failure
- Stage 3 CKD or better (eGFR > 30 mL/min): we recommend that such patients receive antithrombotic therapy as determined by the “CCS algorithm” (YES)
- Stage 4 CKD (eGFR 15-30 mL/min): we suggest that such patients receive antithrombotic therapy as determined by the “CCS algorithm” (YES)
- Stage 5 CKD (eGFR < 15mL/min or dialysis dependent): we suggest that such patients not routinely receive antithrombotic therapy for stroke prevention in AF (NO)
AHA 2023
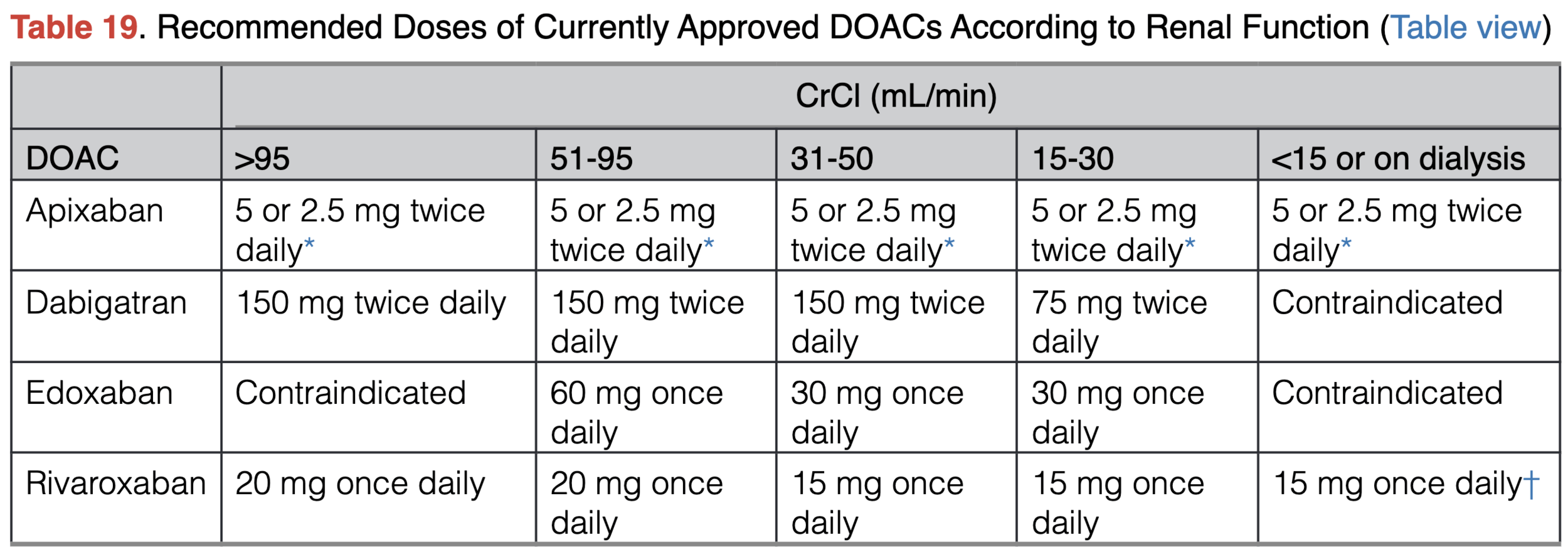
*If at least 2 of the following are present: serum creatinine ≥1.5 mg/dL, age ≥80 y, or body weight ≤60 kg, the recommended dose is 2.5 mg twice daily
Note: would initiate AC CrCl <30 in conjunction with Nephro
CAD
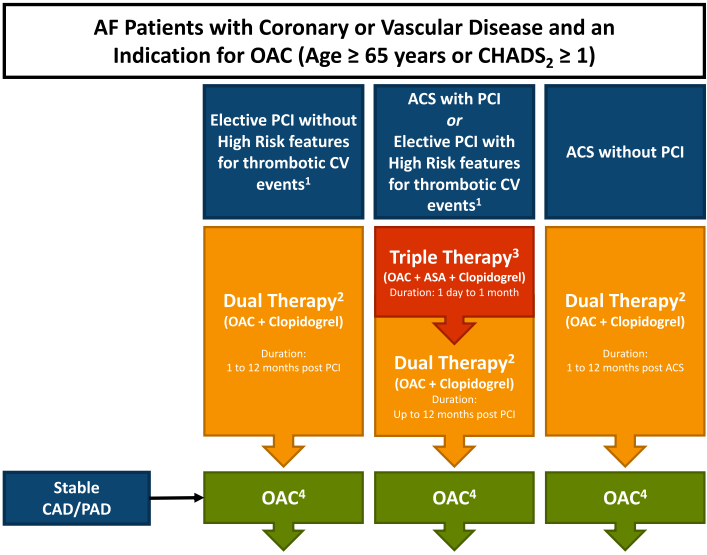
- Note: duration of triple therapy varies by operator/procedure
- Recommendation: go by cath report and if no recommendation need to follow-up with the specific interventionalist
- Note: triple and dual therapy doses can be different (need to look up)
Other Special Populations
- Liver disease: No AC for class C or liver disease associated with significant coagulopathy.”
-
Cancer: Individualize OAC treatment in pts with active cancer.
- Consider DOAC> VKA
-
Frail Elderly
- OAC for most frail elderly – individualizing recommendations if high-risk for bleed, falls
Secondary AF
- Provoked
- Substrate present and the event tipped them over
- Reversible
- No significant substrate, caused by severe transient events such as septic or thyrotoxicosis
- Guidelines recommend anticoagulation while risk factor is present (ie. while hyperthyroid) but not routinely long-term if no reoccurrence
- In practice:
- Repeat Holters
- Risk-benefit discussion with patient and often if significant substrate (ie. RF, valve disease, large atria) will lean towards anticoagtion
Left Atrial Appendage Closure
- Evidence controversial
- Considered in patients with absolute contraindication to anticoagulation
- Recommendation: options due exist, consider referral to a LAAO closure centre for consideration but only done in very select patient population
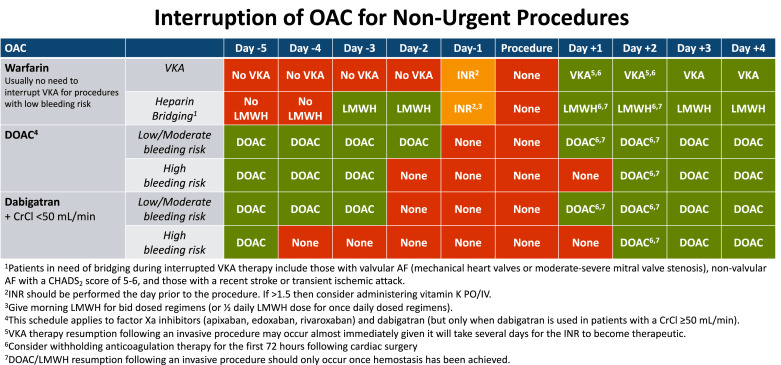
Interrupting Anticoagulation
Interrupting Anticoagulation
- DOACs do not require bridging and warfin only if high risk
- Thrombosis Canada has excellent tools/algorithms
- Key is to confirm with the operator
- Often each site/operator will have own guidelines
- For example, TGH TEE many patients had DOACs inappropriately held. Also many did not have recent INR checks (needed within 48-72 hrs, and INR <4)
Arrhythmia Mangement
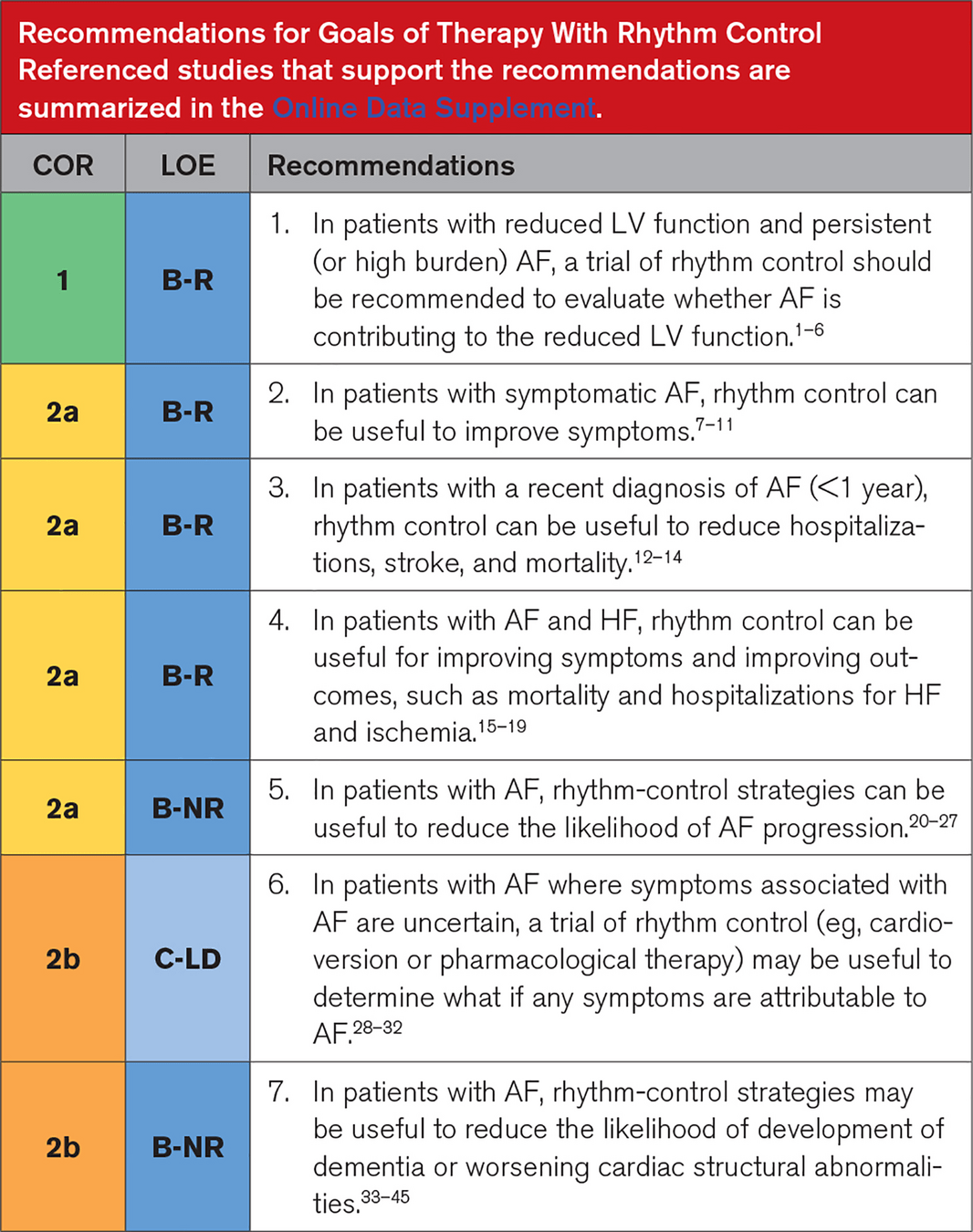
Rate vs Rhythm Control
- Evolving evidence, but broadly we now consider rhythm control:
- New diagnosis (<1 year)
- Symptomatic
- Multiple reocurrences
- Difficult to rate control
- Arrhythmia related cardiomyopathy
- Heart Failure
- Recommendation for family practice
- Always reasonable to initiate rate control but consider early referral to Cardiology
Rhythm Control
Key Points
- Management centralizing to multi-disciplinary AF teams
- Rate control
- EF > 40% - beta blocker or CCB, digoxin
- EF < 40% - beta blocker, digoxin
- Rhythm control
- Antiarrhythmic drugs
- Significant drug-drug reactions
- Monitoring needed (ie. amiodarone)
- Catheter ablation
- Often first line for rhythm control
- Antiarrhythmic drugs
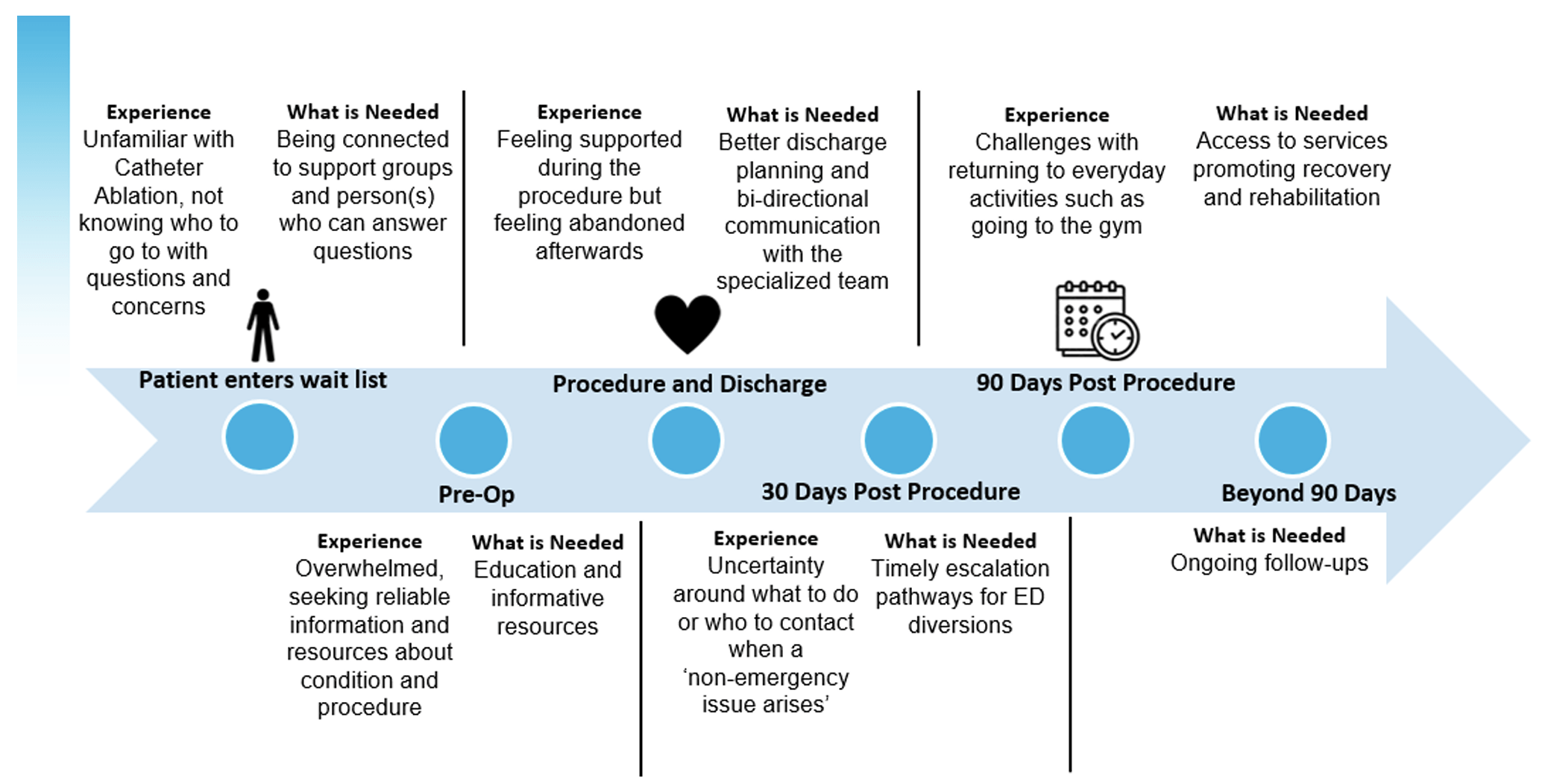
Catheter Ablation
- Will be expanding across the province but anticipate issues
- CorHealth Survey: