CERVICAL DYSTONIA INJECTION TECHNIQUES
Professor Con Yiannikas

Role of EMG

Cervical Dystonia
Clinical Assessment
-
Accuracy of Muscle Localisation
-
Planning of muscles to inject - determination of active muscles
-
Less problems with diffusion
-
Localisation of endplates
Accuracy of Localisation

Cervical Dystonia
Clinical Assessment
-
Muscles deep
-
Not easily identified by surface landmarks
-
Not palpable on examination


Accuracy of Localisation

Cervical Dystonia
Clinical Assessment
- 14 patients with forearm dystonia
- Muscles targeted clinically and then via EMG.
- Only 37% reached the targeted muscles
Molloy et al Neurology 2002
Accuracy of Localisation

Cervical Dystonia
Clinical Assessment
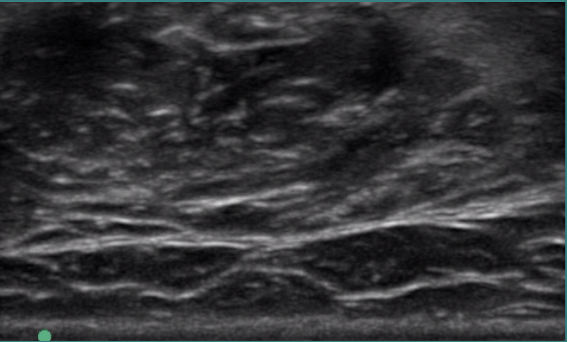
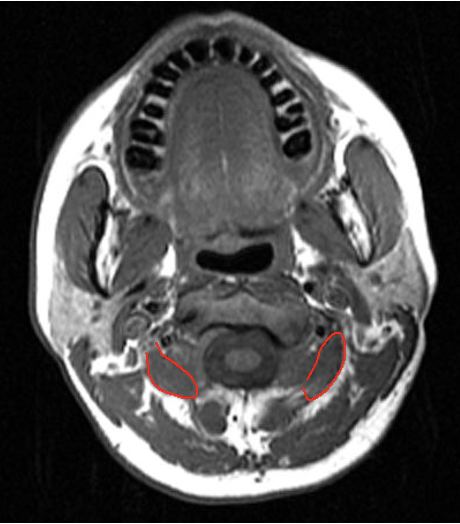
Scalenes


Accuracy of Localisation

Cervical Dystonia
Clinical Assessment
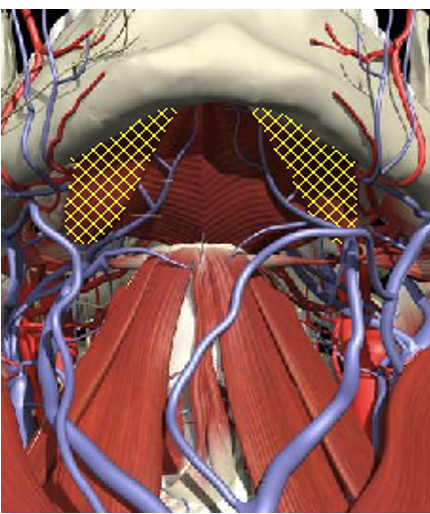
Submentals
Accuracy of Localisation

Cervical Dystonia
Clinical Assessment
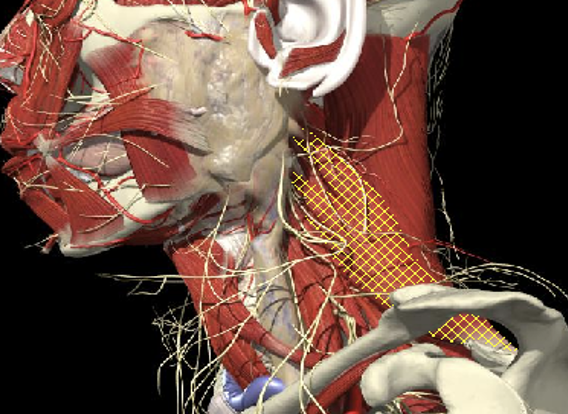
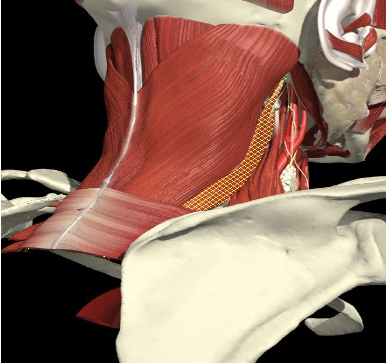
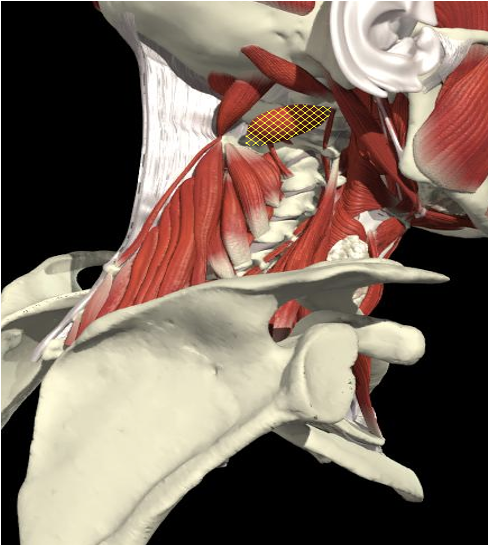
Levator Scapulae

Accuracy of Localisation

Cervical Dystonia
Clinical Assessment
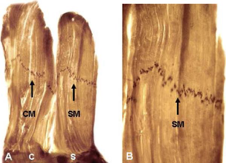
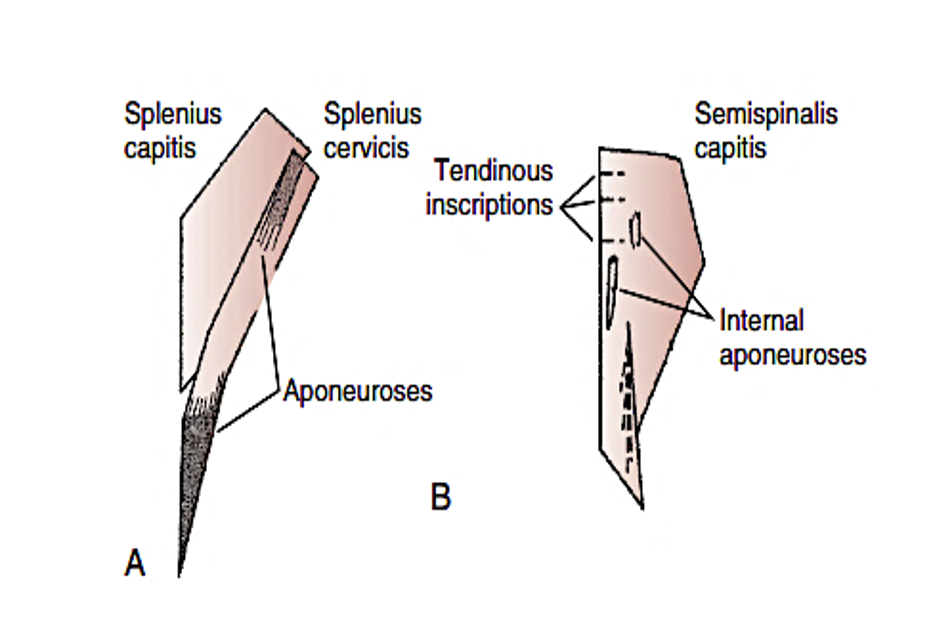
Deep Layers
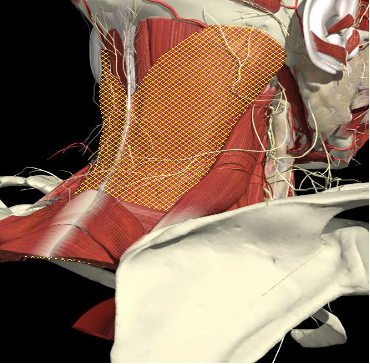
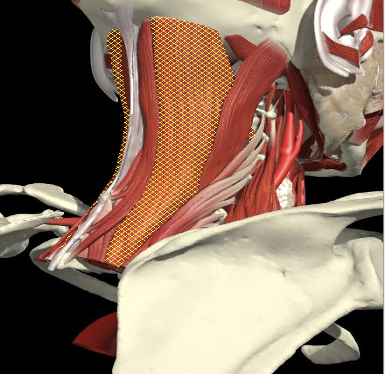
Splenius Capitis
Splenius Cervicis
Semispinalis Capitis
Semispinalis Cervicis
Layer 1
Layer 2
Layer 3

Accuracy of Localisation

Cervical Dystonia
Clinical Assessment

Deep Layers
Accuracy of Localisation

Cervical Dystonia
Clinical Assessment
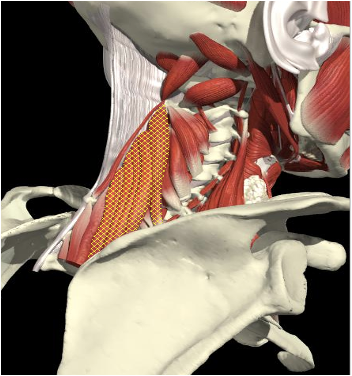
Sub-Occipital
Obliquus Capitis Inferior
-
The C2 vertebral level is identified as a plane 2.5 cm below the mastoid process (3.0 cm below the occipital bone).
-
Midway between the posterior border of the sternomastoid and the dorsal midline. Depth of 3.0-3.5 cm.
Accuracy of Localisation

Cervical Dystonia
Clinical Assessment

Deep Layers

Planning Injections

Cervical Dystonia
Clinical Assessment
Determination of Active Muscles
- Planning treatment requires identification of dystonic muscles and quantification of their involvement.
- Clinical judgment is based on head position and palpation of muscles involved.
- Muscles involved are numerous and interactions complex.
- Examination has a sensitivity of only 0.35 and specificity of 0.74 — a finding that holds even for superficial muscles such as the trapezius and scalenes.
Planning Injections

Cervical Dystonia
Clinical Assessment
Determination of Active Muscles
Dreschler 2000
- looked at 10 patients with rotation and lateral flexion and found significant discrepancy between clinical and EMG determination of dystonic muscles related predominantly to SCM , Trapezius and SC.
- with CD
- Based on physical examinations, 137 neck muscles (33%) were considered to be involved, whereas EMG recordings revealed activity in 302 neck muscles (72%).
Brans – 42 patients
Planning Injections

Cervical Dystonia
Clinical Assessment
Determination of Active Muscles
Planning Injections

Cervical Dystonia
Clinical Assessment
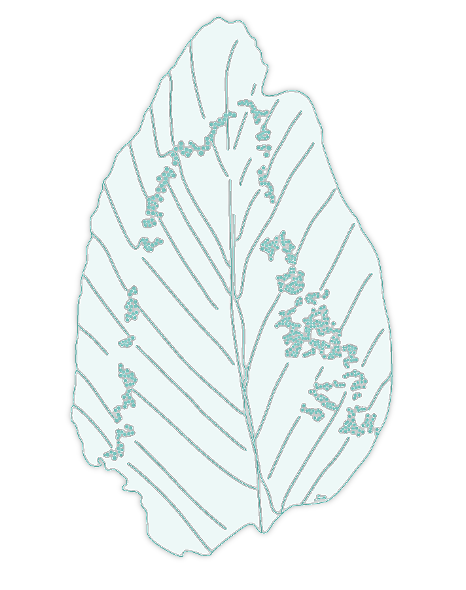
Determination of Active Muscles

- Initial extension and then flexion
- Rotation to left
- No obvious shoulder elevation
- Very active Levator Scapulae
Levator Scapulae
Levator Scapulae
Planning Injections

Cervical Dystonia
Clinical Assessment
Determination of Active Muscles
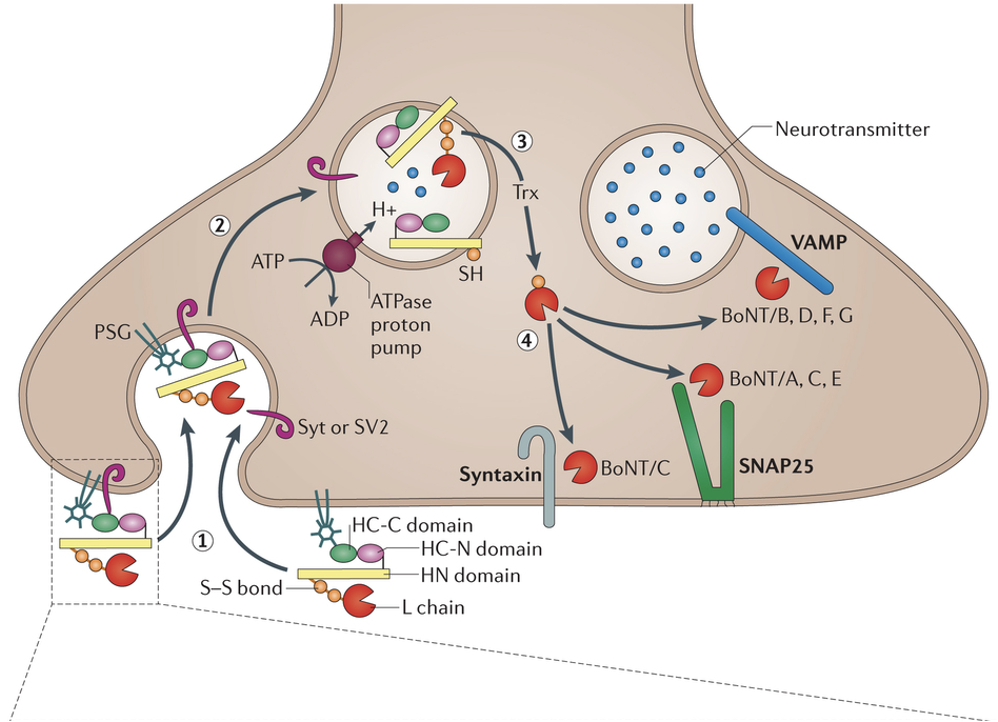
- Good evidence to suggest activity increases the acceptor protein turnover and determines the amount of toxin that enters the presynaptic terminal and ultimately the degree of saturation with toxin affects the time taken for reinnervation and the duration of the effect of the toxin
- i.e. Degree of weakness and duration of effect are both affected by injecting into an active muscle
Endplates

Cervical Dystonia
Clinical Assessment
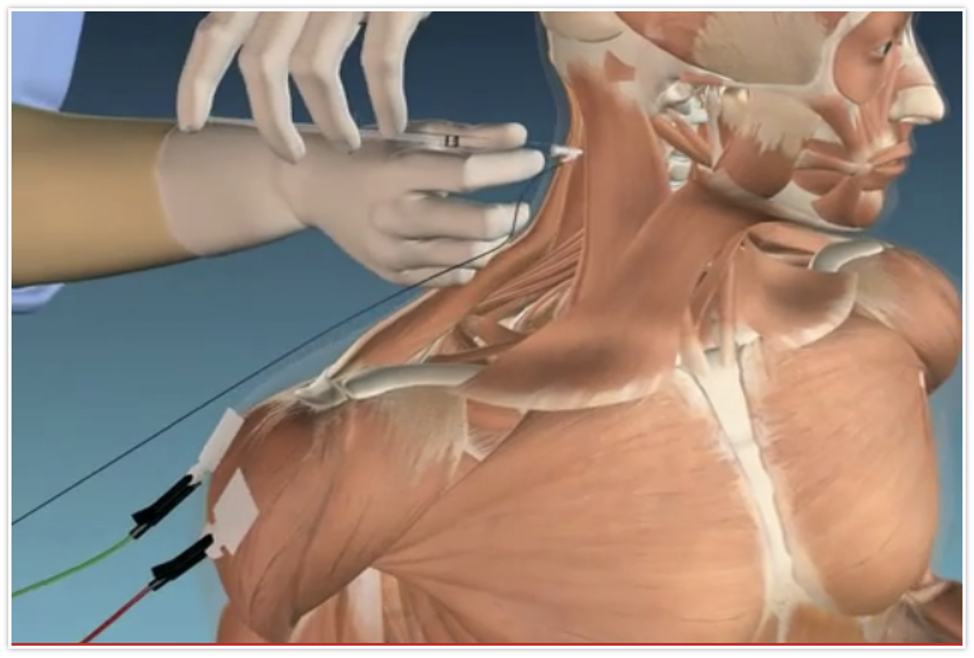
EMG for Localisation
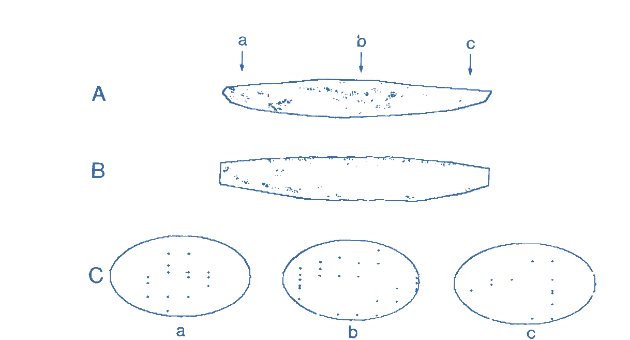
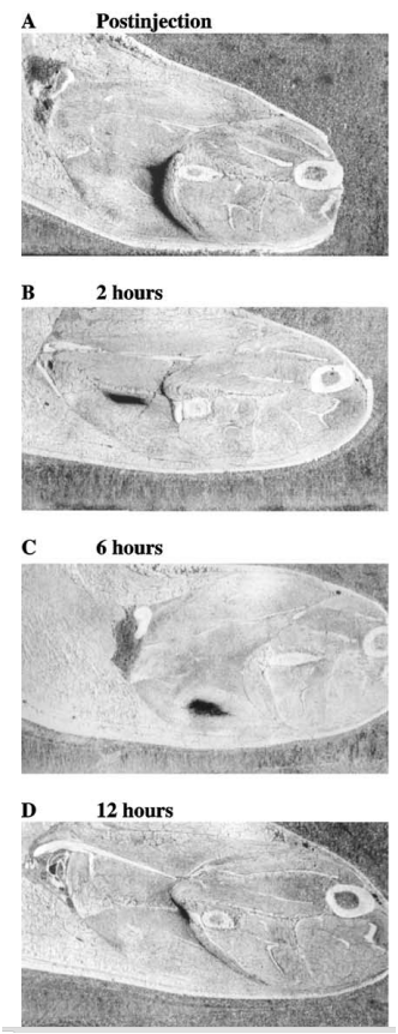
- The importance of targeting the motor endplate has been emphasised in animal models.
- Proximity to endplate will increase the speed of uptake and degree of terminal saturation and the ultimate effectiveness of the toxin.
- Using rat anterior tibialis muscle, Shaari and Sanders demonstrated that toxin injection into the motor endplate region produces the greatest paralysis. Injections only 0.5 cm away from the region resulted in a 50% decrease in paralysis.
Endplates

Cervical Dystonia
Clinical Assessment
Rat Tibialis Anterior
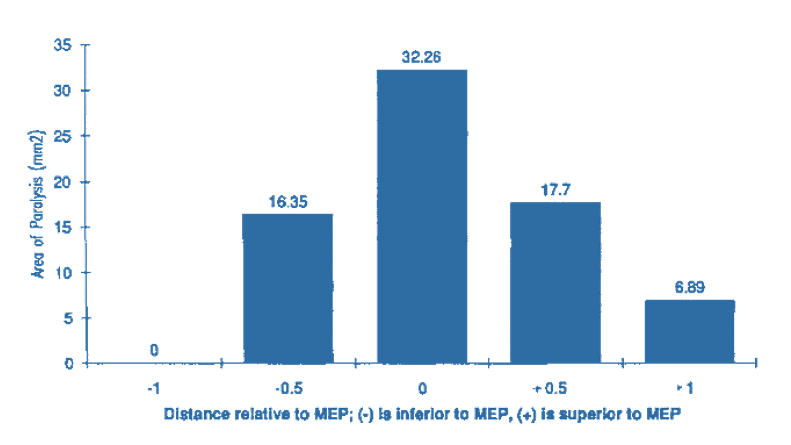

Normal
1 cm

MEP
0.5 cm
Area of paralysis
Distribution of Endplates

Cervical Dystonia
Clinical Assessment
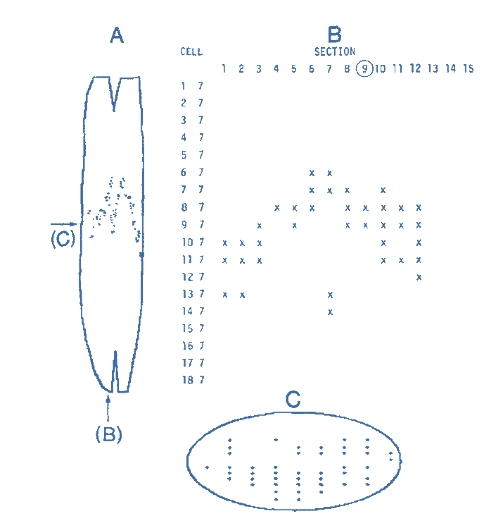
Tibialis Anterior
Biceps
Distribution of Endplates

Cervical Dystonia
Clinical Assessment
Gastrocnemius

Distribution of Endplates

Cervical Dystonia
Clinical Assessment
Sternocleidomastoid
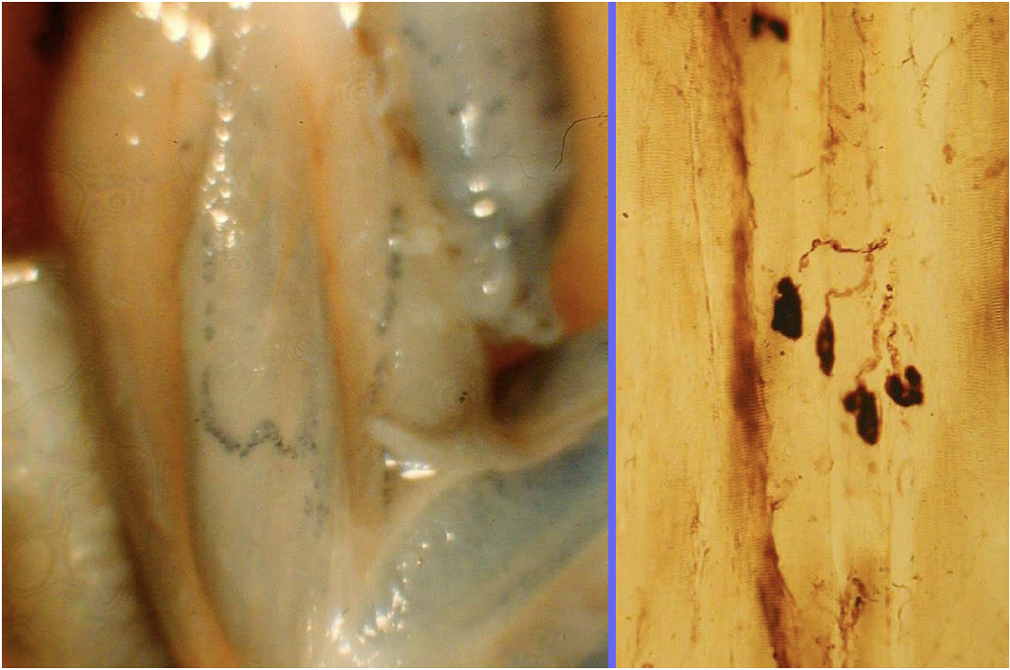
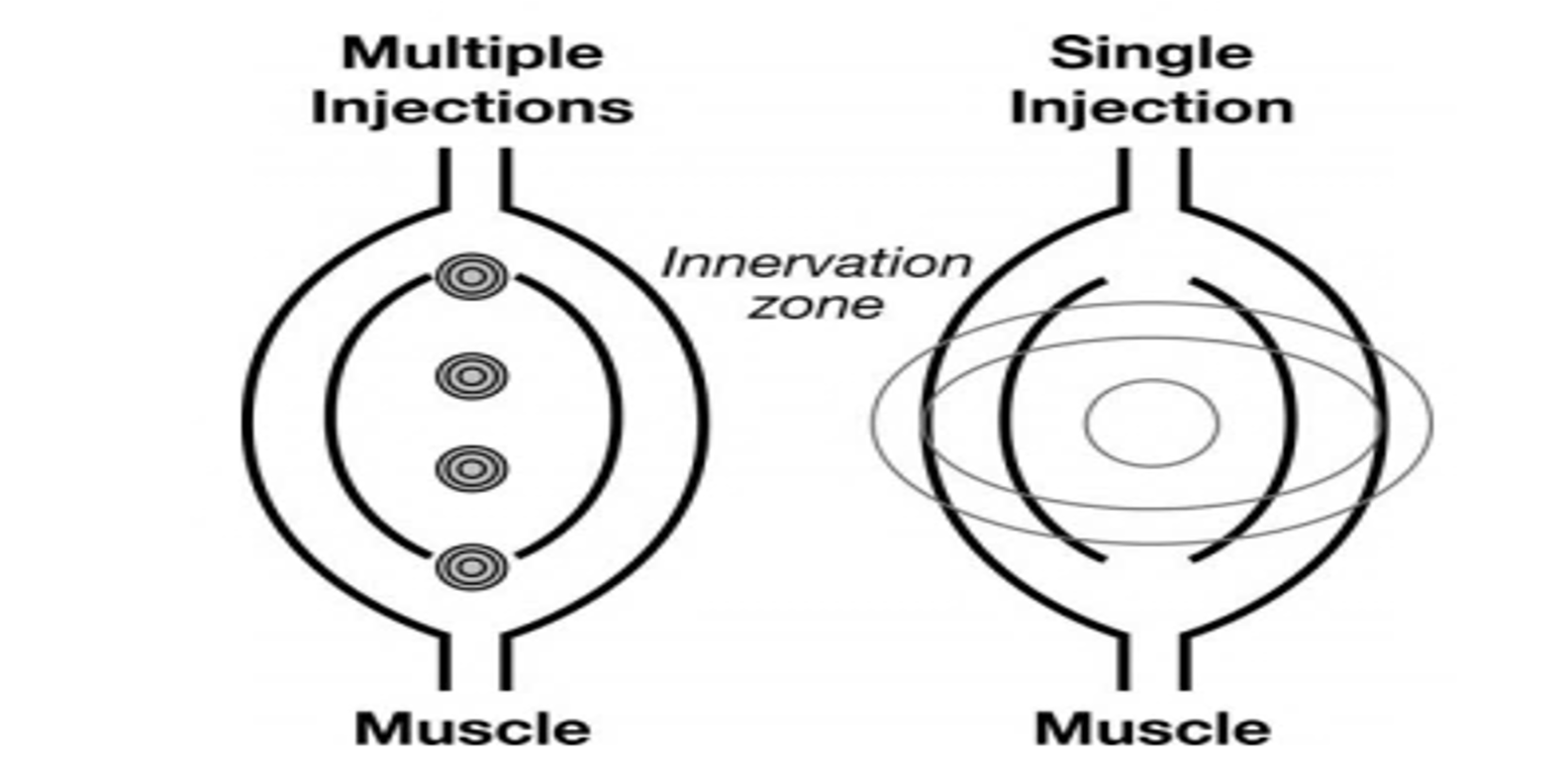
Diffusion

Cervical Dystonia
Clinical Assessment
-
If muscle injection not near endplate BTX more likley to diffuse outside of target muscles.
-
Spread is estimated to be 2.5–4.5 cm, with the size of the diffusion field being proportional to the amount of toxin delivered.
-
Can occur across fascial planes.
-
Series of patients with upper limb dystonia, weakness of uninjected muscles adjacent to those injected was found in 63% of patients.
-
Non EMG injections rely on diffusion but may weaken non dystonic muscles
Diffusion

Cervical Dystonia
Clinical Assessment
-
Diffusion may be limited by muscle architecture and therefore if you are in the wrong area it may be ineffective. (Rosales 2006)
Affect of Muscle Architecture
Botulinum Toxin Studies

Cervical Dystonia
Clinical Assessment
Botulinum toxin injection for spasmodic torticollis: Increased magnitude of benefit with electromyographic assistance
Cynthia L. Comella et al. Neurology 1992
-
52 patients – 28 clinical and EMG, 24 clinical.
-
Patients with retrocollis, head tilt, and shoulder elevation demonstrated additional benefit with EMG-assisted BOTOX injection
-
Significantly greater magnitude of improvement was present in the EMG group
-
The percentage of patients showing any improvement after BOTOX was similar in both
Botulinum Toxin Studies

Cervical Dystonia
Clinical Assessment
Secondary Nonresponsiveness to Botulinum Toxin A in Cervical Dystonia: The Role of Electromyogram-Guided Injections, Botulinum Toxin A Antibody Assay, and the EDBTest
Carla Cordivari et al. 2006
-
20 patients with cervical dystonia who had started to respond poorly to botulinum toxin A (BTXA)
-
11 patients, there was a poor clinical response to EMG-guided BTXA injections. Seven of these 11 had small EDB decrement and BTXA antibodies using IPA, suggesting resistance to BTXA.
-
Nine patients had a good clinical response to EMG-guided injections and all of these patients showed an obvious decrement on the EDB test.

Botulinum Toxin Studies

Cervical Dystonia
Clinical Assessment
Botulinum toxin in cervical dystonia:
low dosage with electromyographic guidance
J. W. M. Brans et al 1995
-
60 patients with cervical dystonia
-
Dosage of 200-400 mouse units BTA (Dysport) effective with fewer side effects. EMG guidance and application of BTA into deep cervical muscles may improve the clinical effect.

Occasional Surprises

Cervical Dystonia
Clinical Assessment
Conclusions

Cervical Dystonia
Clinical Assessment
-
It is known that BTX diffuses outside of target muscles.
-
Toxin should be delivered to the target muscle; the further off-target the injection, the more that uninvolved, non-dystonic muscles will be weakened.
-
Cervical dystonia involves superficial muscles that may be readily palpated. However, needle EMG exploration of the dystonic neck often reveals involvement of deeper muscles that would be difficult to access.
-
Report in patients with cervical dystonia demonstrated the safety of needle EMG guidance and that there was no substantial increase in the time required for injection.
-
Fewer side effects, such as neck weakness and dysphagia, compared with prior studies, which the investigators attributed to the accuracy afforded by needle EMG guidance.
-
Exact localization of toxin allows for a lower dose to produce an equivalent effect.
Injection Sites

Cervical Dystonia
Clinical Assessment
Dilution / Dose

Cervical Dystonia
Clinical Assessment
-
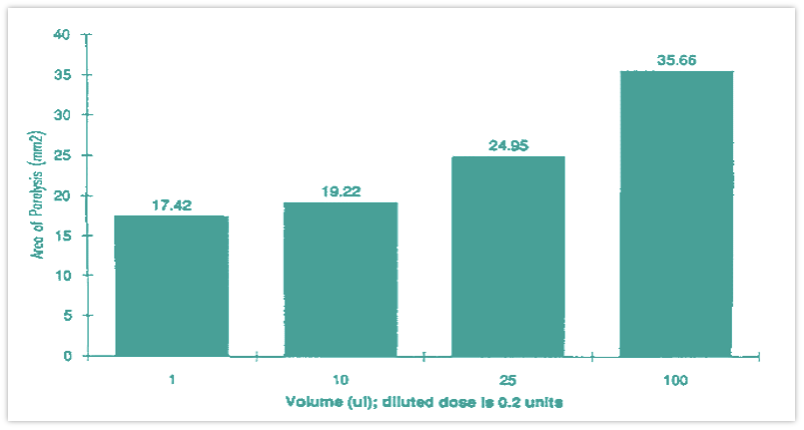
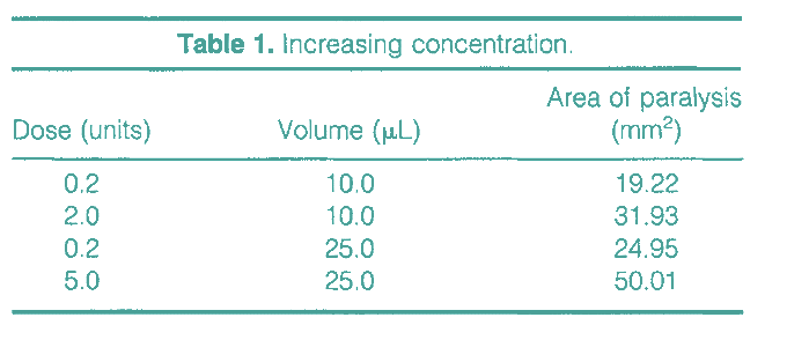
Paralysis doubles with a 25-fold increase in dose (constant volume), whereas a 100-fold increase in volume (constant dose) is needed to double paralysis