Fibroblastic Reticular Cells in Secondary Lymphoid Organs
Mechthild Lütge
PhD Defense, 22.03.2023
University of Zurich
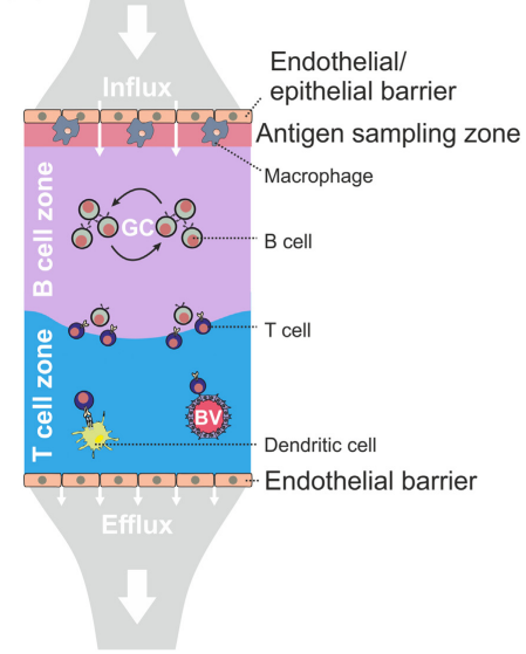
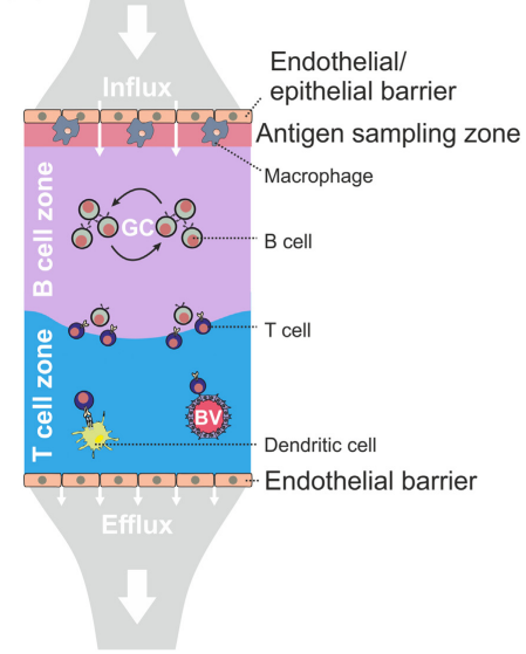
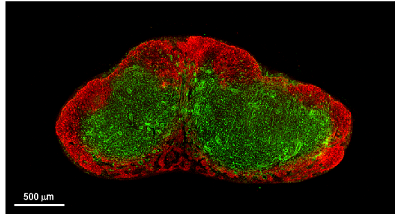
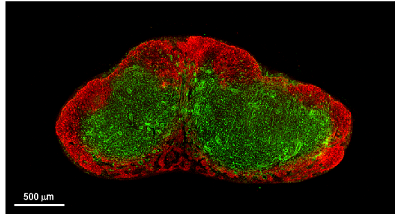
Lymph Nodes
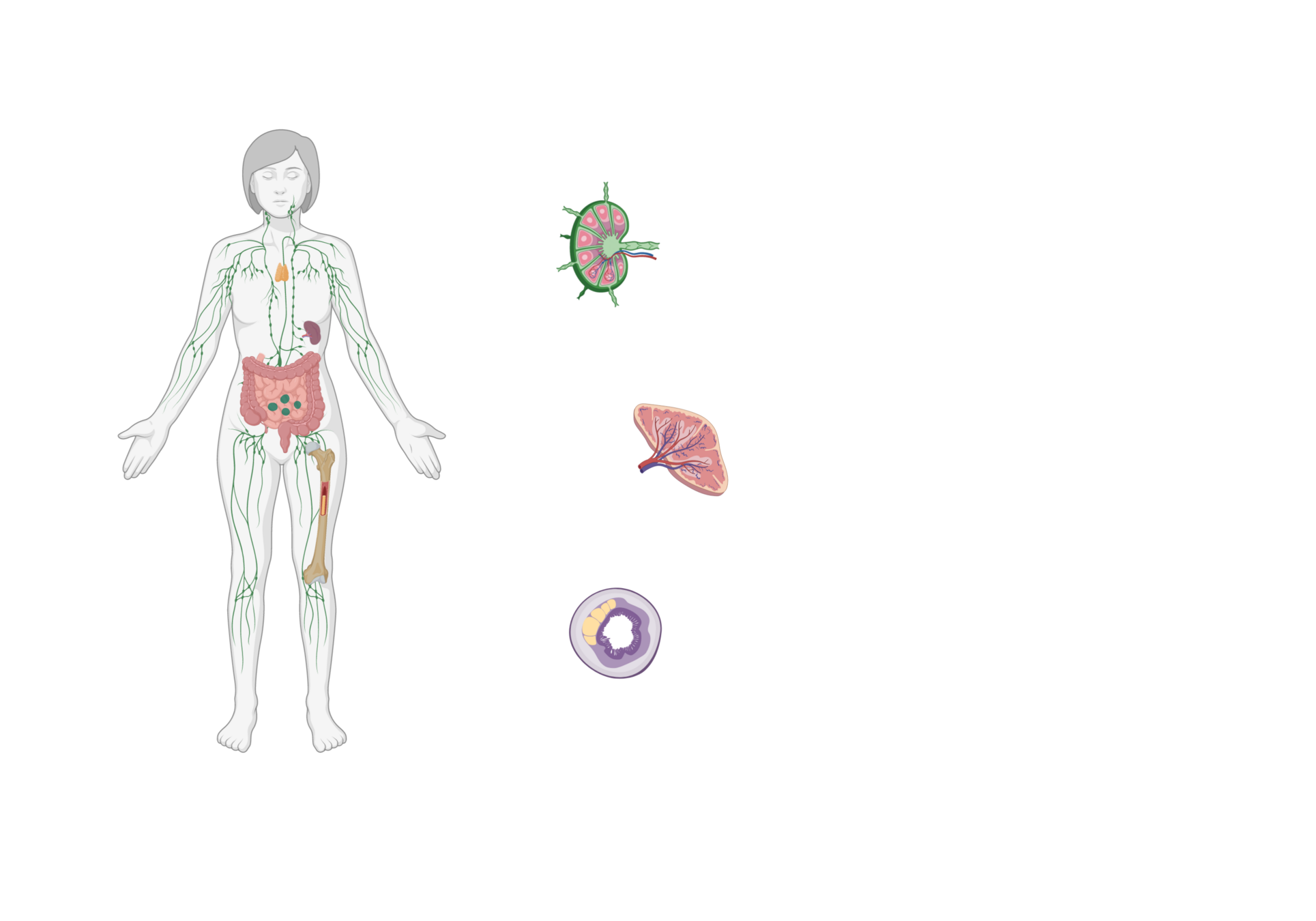
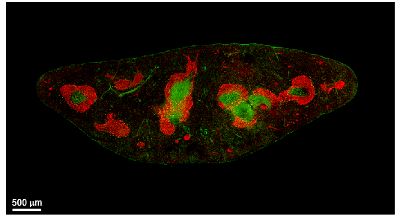
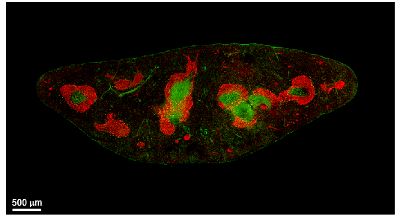
Spleen
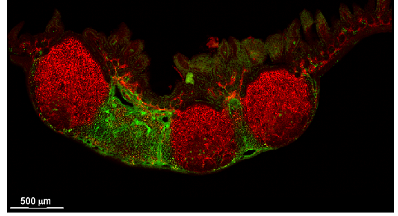
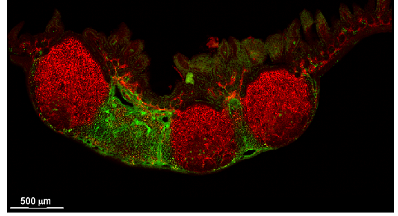
Peyer's patches
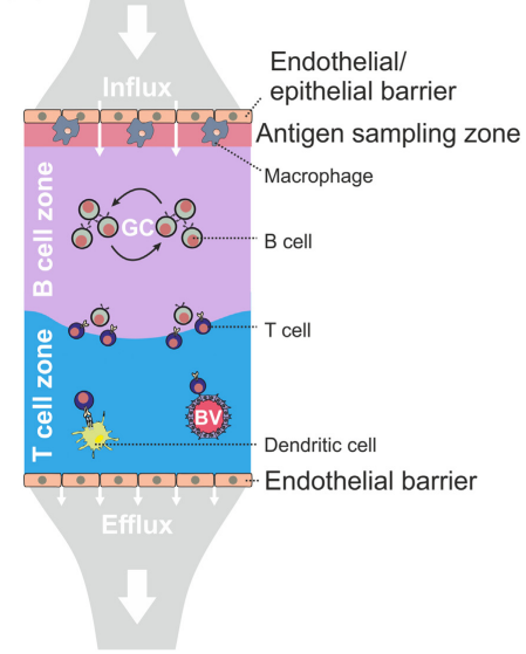
Secondary Lymphoid organs (SLO)
Dedicated sites where adaptive immunity is mounted to pathogens in the lymph, blood or intestine
Fibroblastic reticular cells orchestrate SLO organization
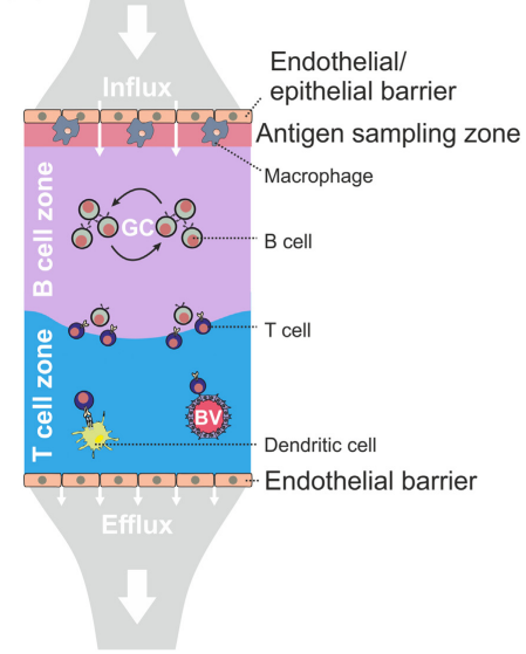
Acton et al. Trends in Immunology, 2021
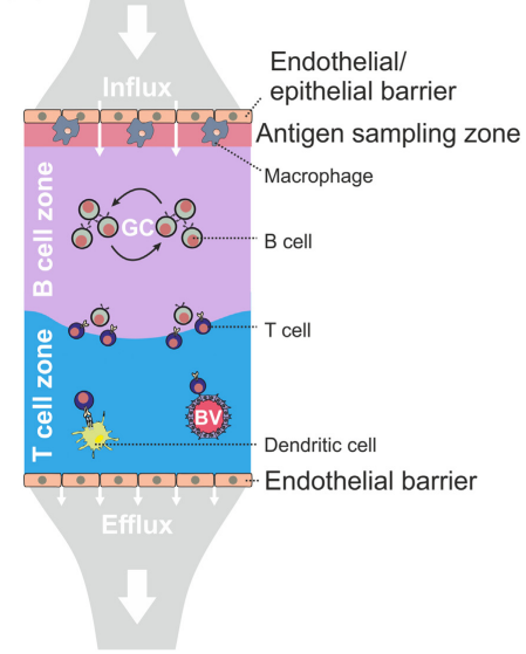
Acton et al. Trends in Immunology, 2021
Fibroblastic reticular cells (FRC) form specialized immune cell niches to support adaptive immune responses
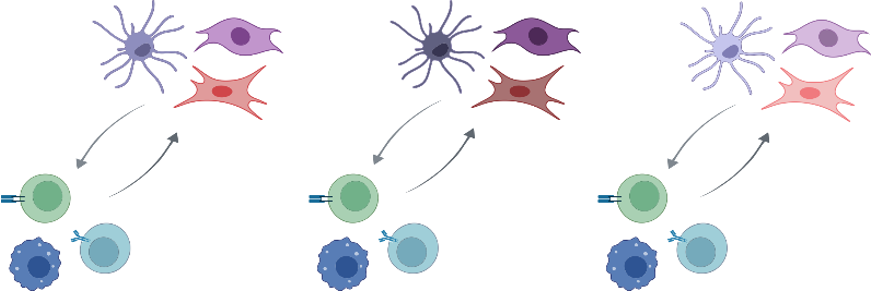
Fibroblastic reticular cells orchestrate SLO organization
Fibroblastic reticular cells orchestrate SLO organization

created with biorender.com
Fibroblastic reticular cells orchestrate SLO organization

Migration
created with biorender.com
Fibroblastic reticular cells orchestrate SLO organization

Migration
Activation
and survival
created with biorender.com
Fibroblastic reticular cells orchestrate SLO organization

Migration
Activation
and survival
Extracellular matrix
created with biorender.com
Fibroblastic reticular cells orchestrate SLO organization

Migration
Activation
and survival
Extracellular matrix
Antigen presentation
and immune cell interaction
created with biorender.com
Fibroblastic reticular cells orchestrate SLO organization

Migration
Activation
and survival
Extracellular matrix
Antigen presentation
and immune cell interaction
created with biorender.com
→ Modulators of immune responses:
Strength and specificity of immune response
Fibroblastic reticular cells orchestrate SLO organization

Migration
Activation
and survival
Extracellular matrix
Antigen presentation
and immune cell interaction
created with biorender.com
→ Modulators of immune responses:
Strength and specificity of immune response
→ Prototypic immune-interacting fibroblast

Migration
Activation
and survival
Extracellular matrix
Antigen presentation
and immune cell interaction
created with biorender.com
Fibroblastic reticular cells as prototypic immune-interacting fibroblasts
→ Modulators of immune responses:
- Vaccine efficacy

Migration
Activation
and survival
Extracellular matrix
Antigen presentation
and immune cell interaction
created with biorender.com
Fibroblastic reticular cells as prototypic immune-interacting fibroblasts
→ Modulators of immune responses:
- Autoimmunity and inflammatory disorders
- Vaccine efficacy

Migration
Activation
and survival
Extracellular matrix
Antigen presentation
and immune cell interaction
created with biorender.com
Fibroblastic reticular cells as prototypic immune-interacting fibroblasts
→ Modulators of immune responses:
- Autoimmunity and inflammatory disorders
- Antitumor immuntity
- Vaccine efficacy
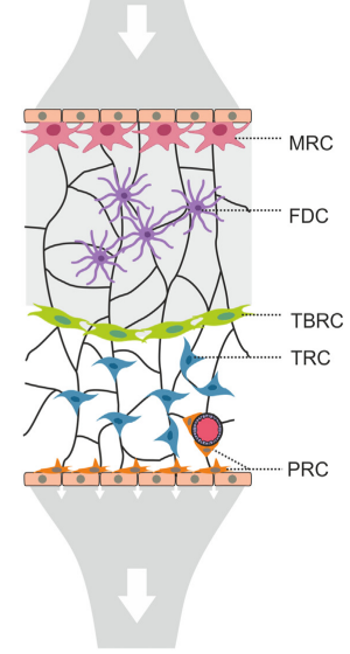
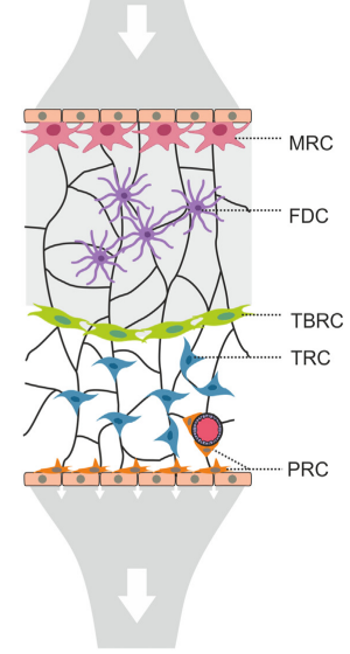
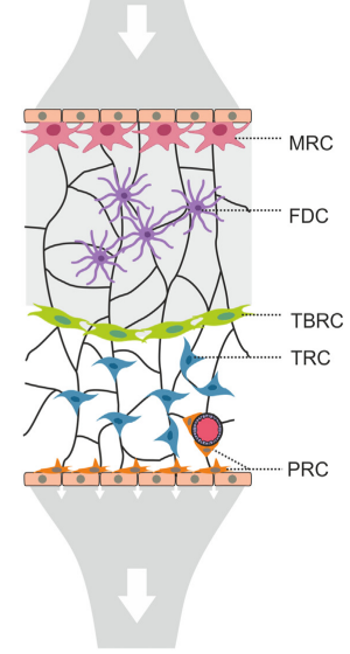
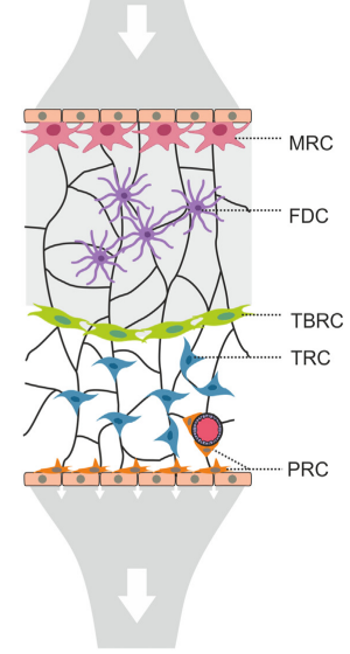
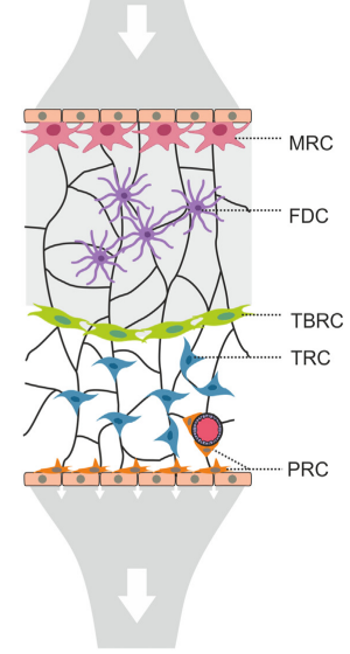
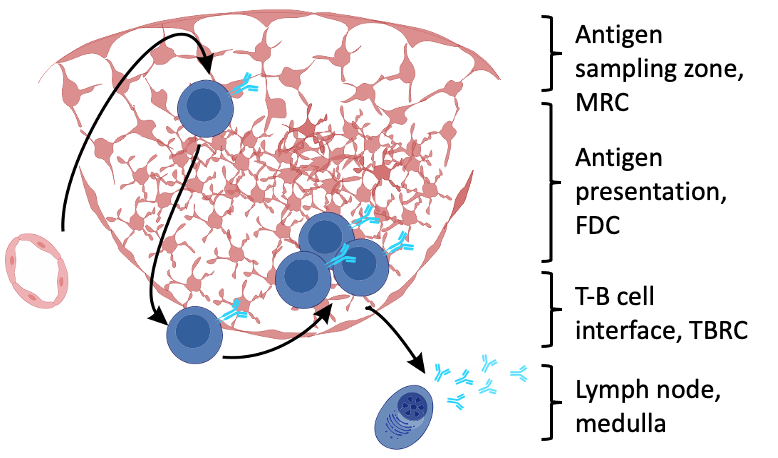
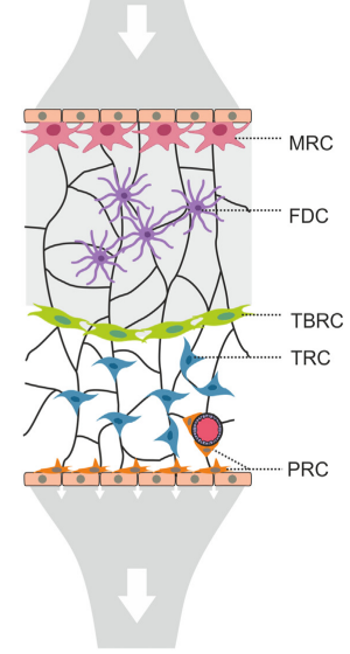
Fibroblastic reticular cells orchestrate SLO organization
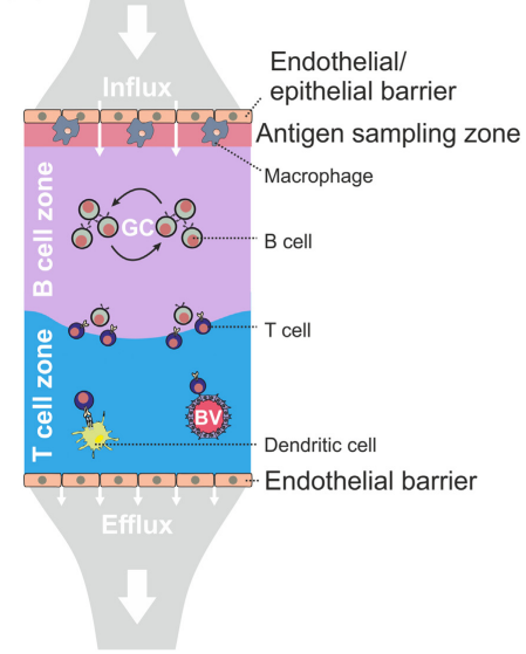
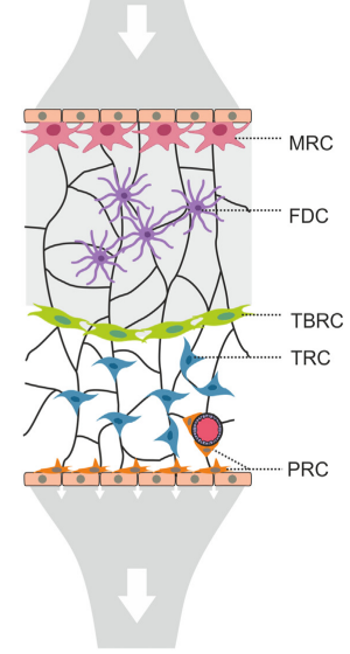
Acton et al. Trends in Immunology, 2021
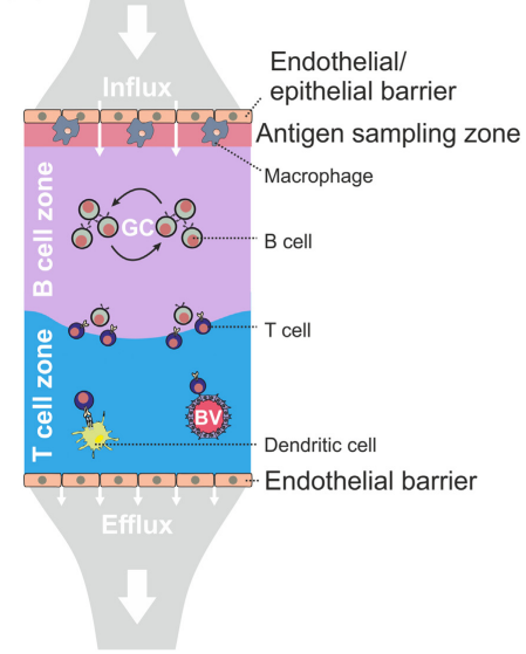
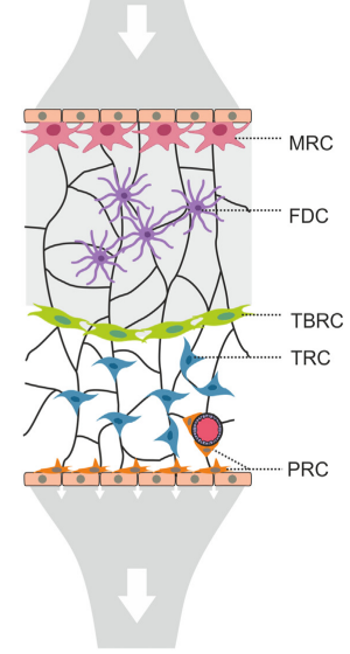
Acton et al. Trends in Immunology, 2021
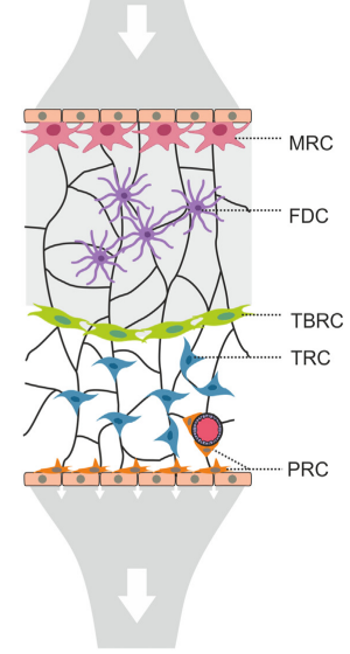
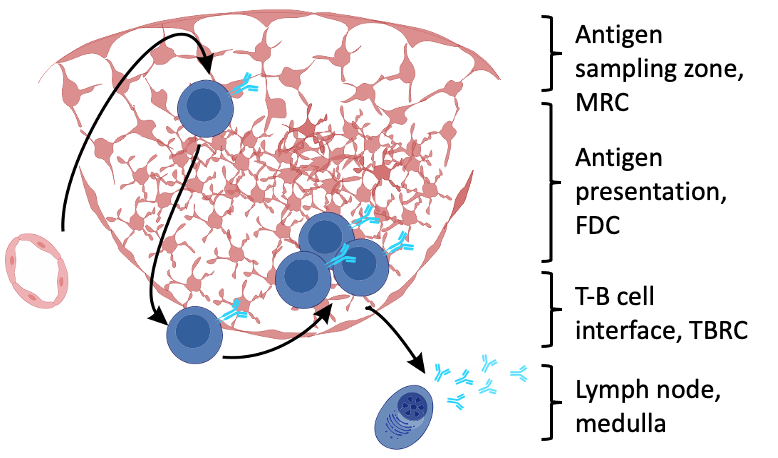
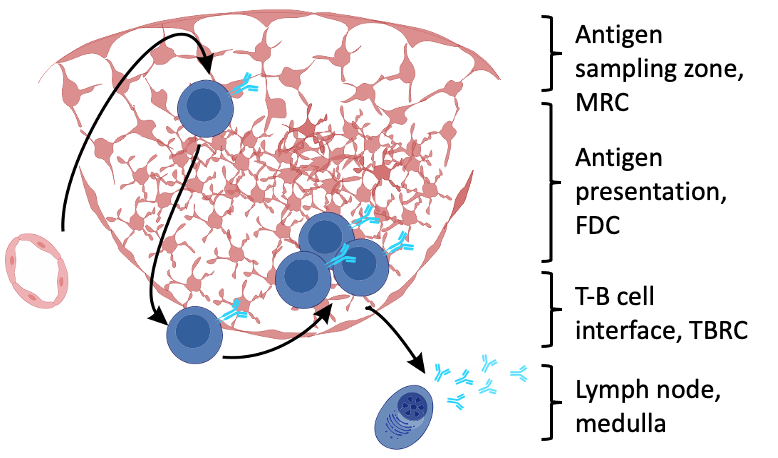
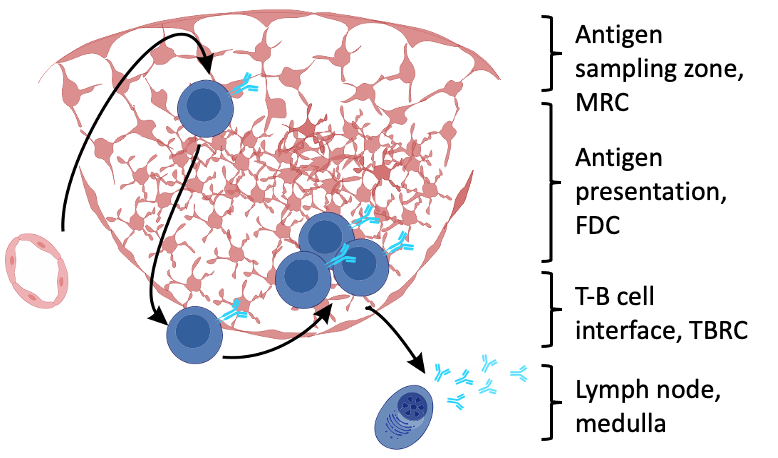
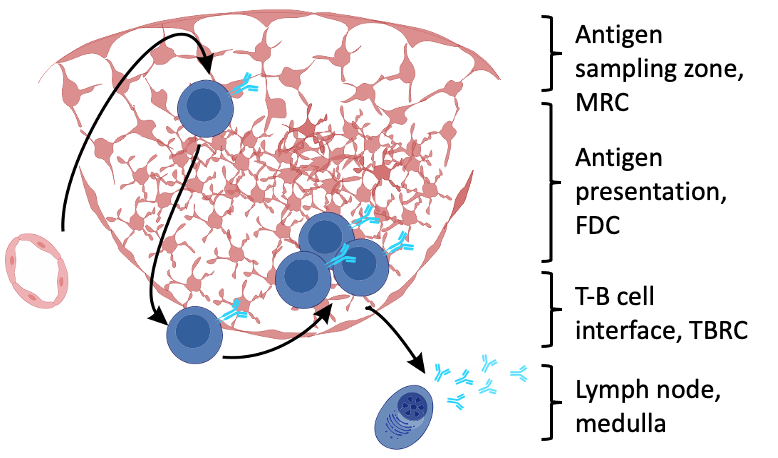
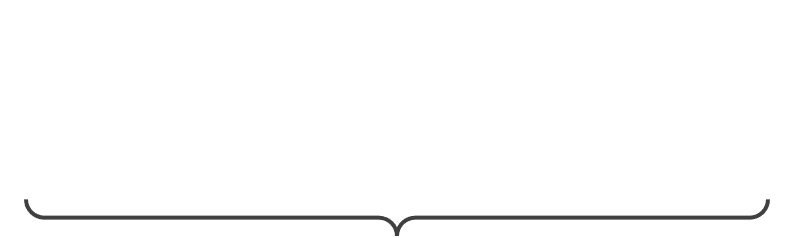
Fibroblastic reticular cells orchestrate SLO organization
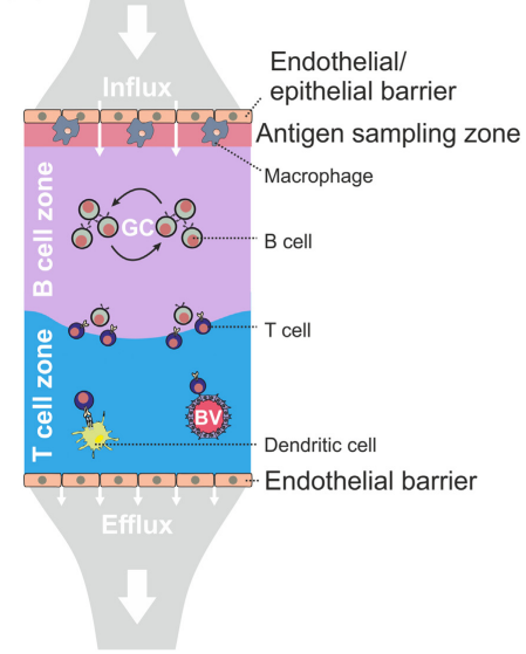
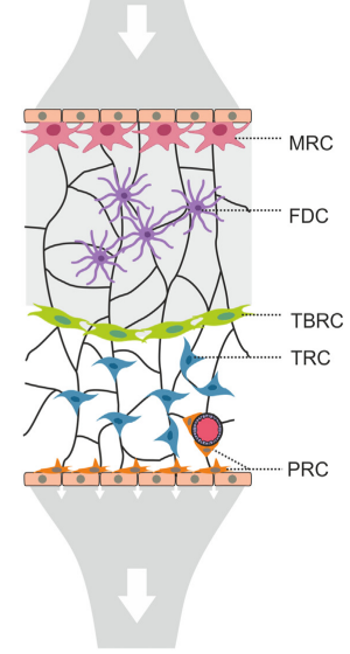
Antigen sampling zone:
- Marginal reticular cells (MRCs)
Acton et al. Trends in Immunology, 2021
Fibroblastic reticular cells orchestrate SLO organization
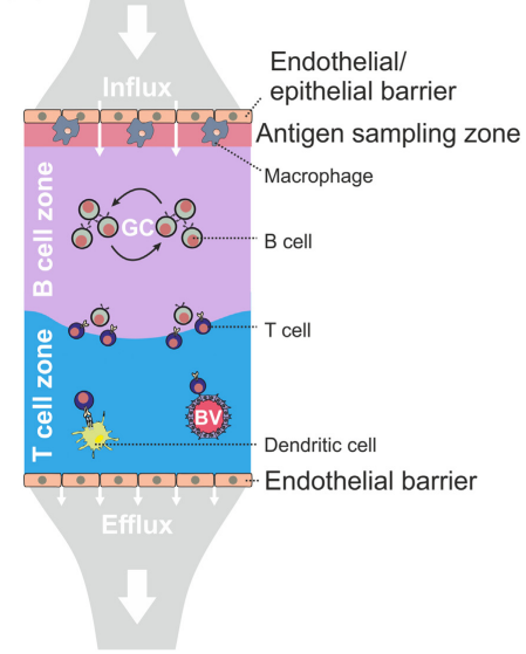
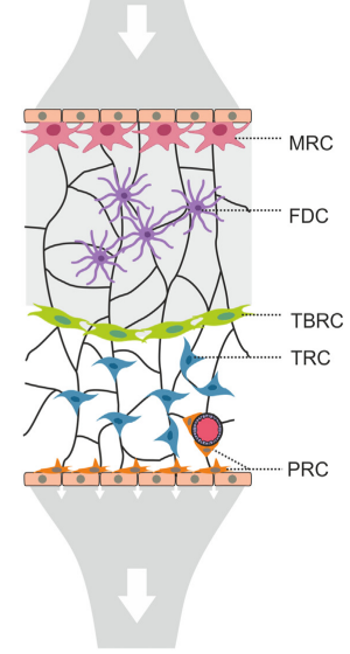
Antigen sampling zone:
- Marginal reticular cells (MRCs)
Acton et al. Trends in Immunology, 2021
B cell follicle:
- Follicular dendritic cells (FDCs)
Fibroblastic reticular cells orchestrate SLO organization
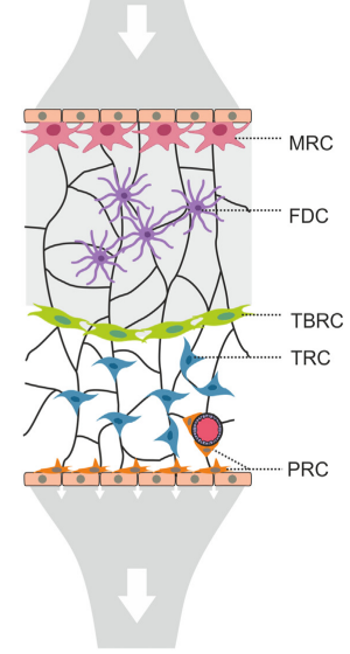
Antigen sampling zone:
- Marginal reticular cells (MRCs)
Acton et al. Trends in Immunology, 2021
B cell follicle:
- Follicular dendritic cells (FDCs)
T-B border region:
- T-B border reticular cells (TBRCs)
Fibroblastic reticular cells orchestrate SLO organization
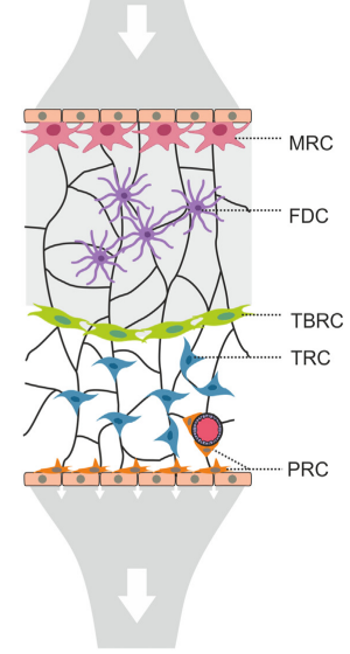
Antigen sampling zone:
- Marginal reticular cells (MRCs)
Acton et al. Trends in Immunology, 2021
B cell follicle:
- Follicular dendritic cells (FDCs)
T-B border region:
- T-B border reticular cells (TBRCs)
T cell zone:
- T cell zone reticular cells (TRCs)
Fibroblastic reticular cells orchestrate SLO organization
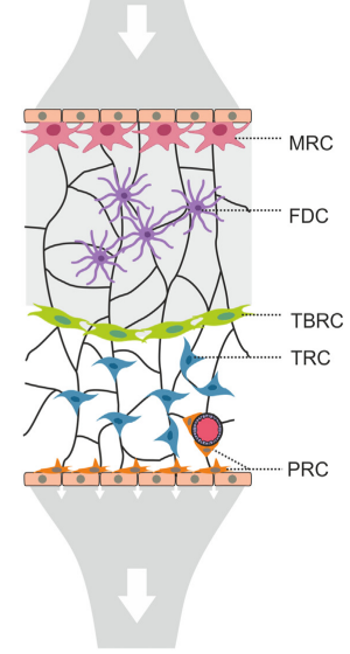
Antigen sampling zone:
- Marginal reticular cells (MRCs)
Acton et al. Trends in Immunology, 2021
B cell follicle:
- Follicular dendritic cells (FDCs)
T-B border region:
- T-B border reticular cells (TBRCs)
T cell zone:
- T cell zone reticular cells (TRCs)
Perivascular space:
- Perivascular reticular cells (PRCs)
Fibroblastic reticular cells orchestrate SLO organization
To what extend are FRC underpinned niches functionally conserved across:
Fibroblastic reticular cells orchestrate SLO organization
To what extend are FRC underpinned niches functionally conserved across:
(1.) SLOs?
Fibroblastic reticular cells orchestrate SLO organization
To what extend are FRC underpinned niches functionally conserved across:
(1.) SLOs?
(2.) Species?
Fibroblastic reticular cells orchestrate SLO organization

To what extend are FRC underpinned niches functionally conserved across:
(1.) SLOs?
(2.) Species?
(3.) Activation?
Fibroblastic reticular cells orchestrate SLO organization

To what extend are FRC underpinned niches functionally conserved across:
(1.) SLOs?
(2.) Species?
(3.) Activation?
→ What factors shape FRC subset identity and function?
Fibroblastic reticular cells orchestrate SLO organization
- Conserved stromal–immune cell circuits secure B cell homeostasis and function
- PI16+ reticular cells form reactive immune cell niches in human lymph nodes
Fibroblastic reticular cells orchestrate SLO organization
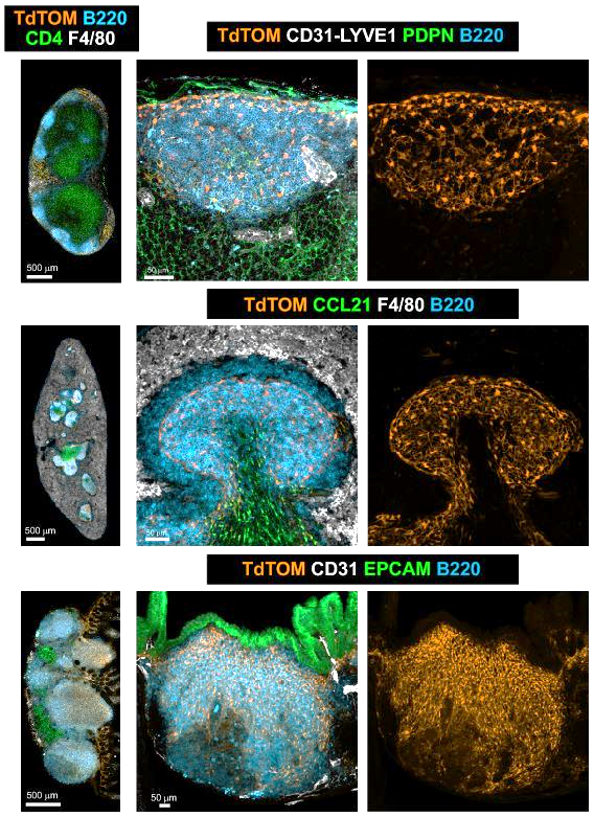
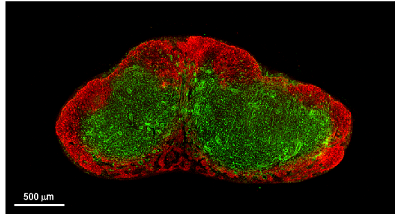
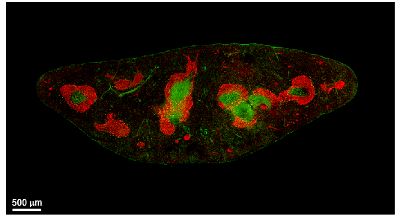
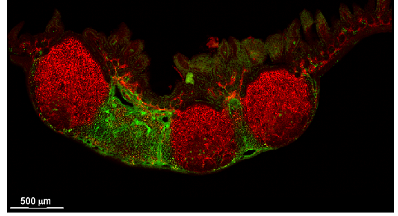
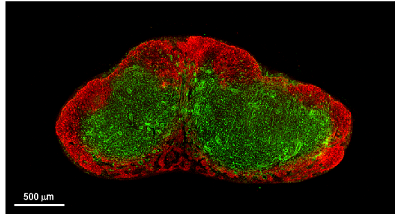
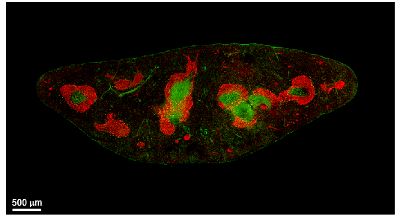
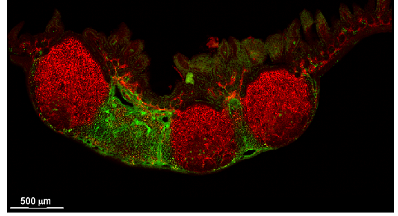
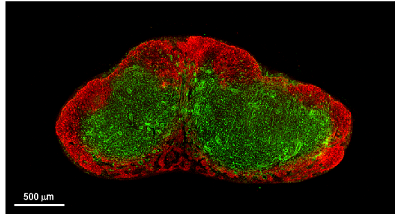
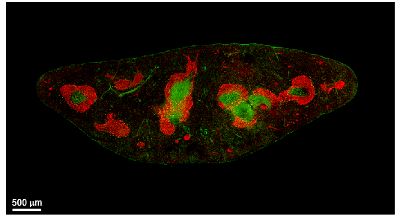
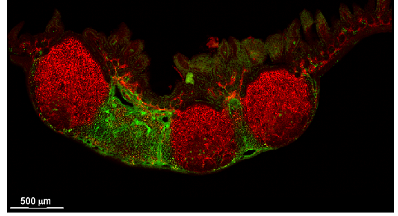
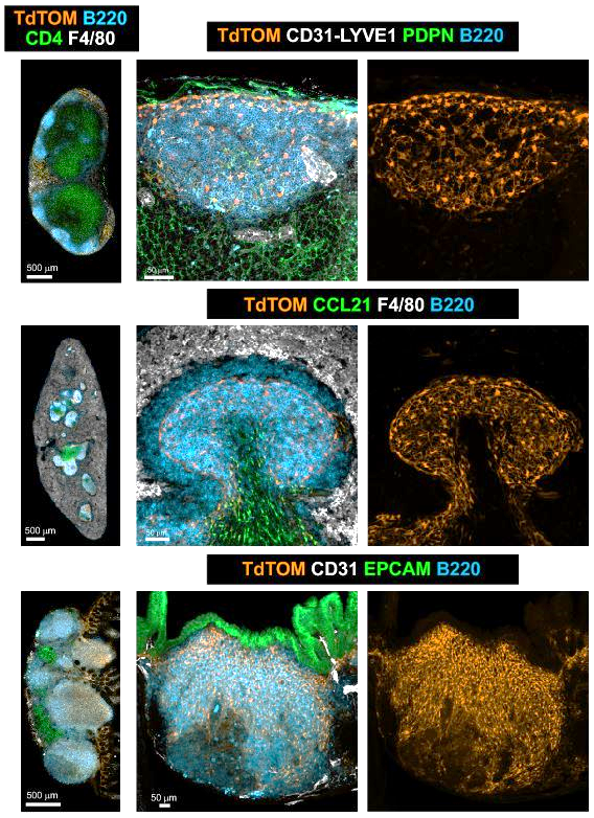
B cell zone reticular cells direct efficient humoral immunity
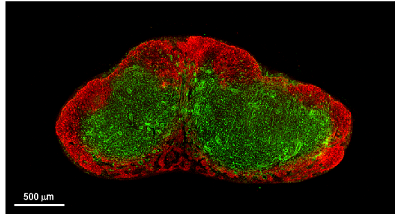
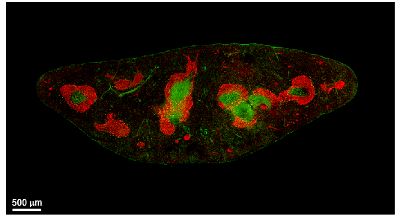
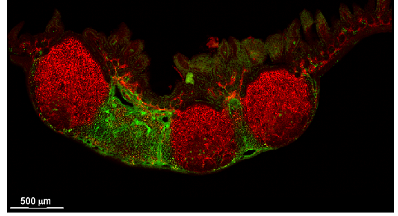
CXCL13 CCL19/CCL21
Peyer's patch
Spleen
Lymph node
CXCL13+ FRC = B cell zone reticular cells (BRCs)
B cell zone reticular cells direct efficient humoral immunity
CXCL13 CCL19/CCL21
Peyer's patch
Spleen
Lymph node
CXCL13+ FRC = B cell zone reticular cells (BRCs)
B cell zone reticular cells direct efficient humoral immunity
-
to what extend are BRC underpinned niches functionally conserved across SLO?
CXCL13 CCL19/CCL21
Peyer's patch
Spleen
Lymph node
CXCL13+ FRC = B cell zone reticular cells (BRCs)
B cell zone reticular cells direct efficient humoral immunity
-
to what extend are BRC underpinned niches functionally conserved across SLO?
-
Systemic humoral immunity?
CXCL13 CCL19/CCL21
Peyer's patch
Spleen
Lymph node
CXCL13+ FRC = B cell zone reticular cells (BRCs)
B cell zone reticular cells direct efficient humoral immunity
-
to what extend are BRC underpinned niches functionally conserved across SLO?
-
Systemic humoral immunity?
-
What are major pathways controlling BRC-immune cell interactions?
CXCL13 CCL19/CCL21
Peyer's patch
Spleen
Lymph node
CXCL13+ FRC = B cell zone reticular cells (BRCs)
B cell zone reticular cells direct efficient humoral immunity
-
to what extend are BRC underpinned niches functionally conserved across SLO?
-
Systemic humoral immunity?
-
What are major pathways controlling BRC-immune cell interactions?
-
Are these interactions functionally redundant across SLOs?
CXCL13 CCL19/CCL21
Peyer's patch
Spleen
Lymph node
CXCL13+ FRC = B cell zone reticular cells (BRCs)
Shared B cell follicle and PI16+ BRC subset identity across SLOs
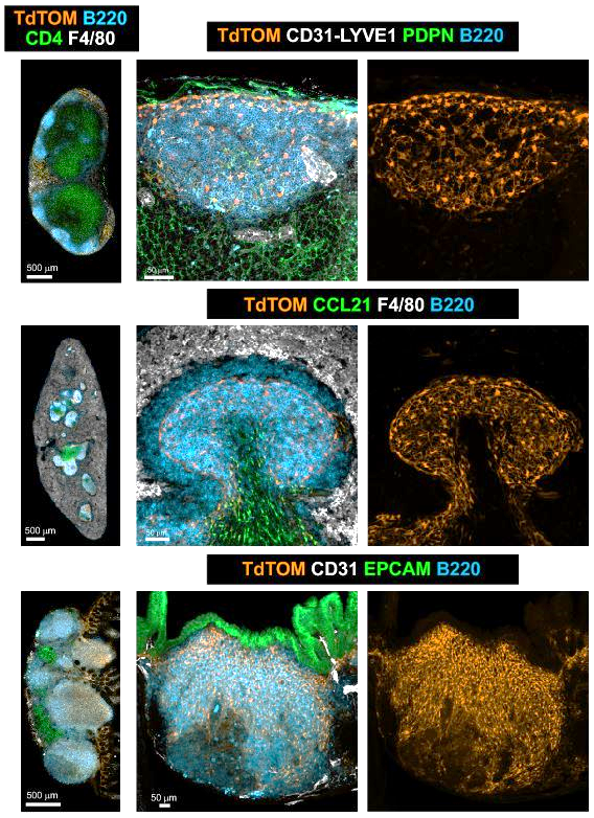
Onder L et al., Immunity, 2017
Lütge et al. Nat. Immunol., 2023
Shared B cell follicle and PI16+ BRC subset identity across SLOs
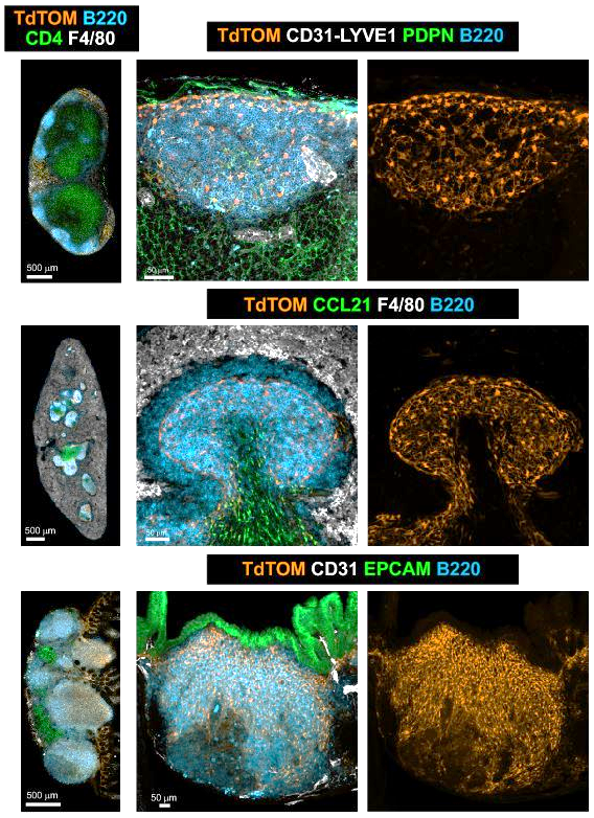
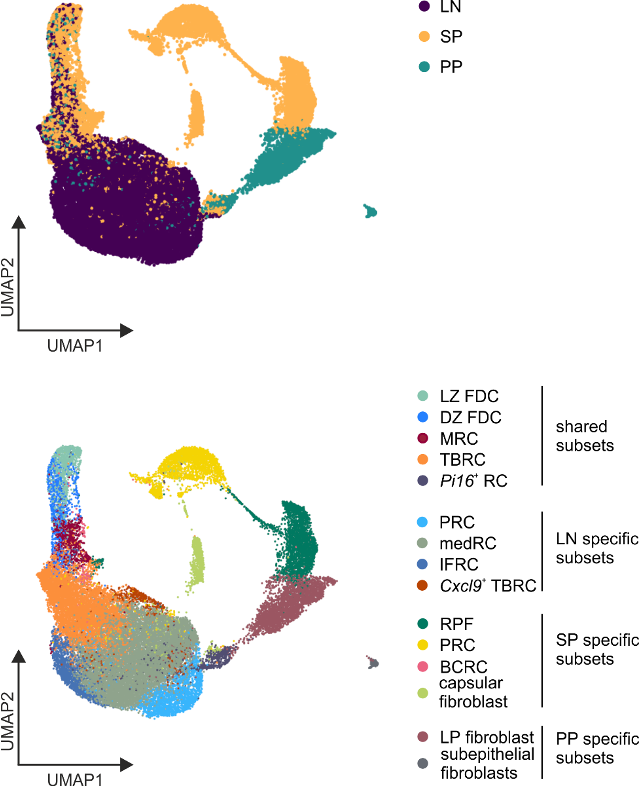
Onder L et al., Immunity, 2017
Lütge et al. Nat. Immunol., 2023
Shared B cell follicle and PI16+ BRC subset identity across SLOs
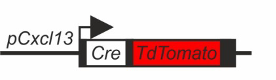
Onder L et al., Immunity, 2017
Lütge et al. Nat. Immunol., 2023
Developmental and anatomical gene sets imprint BRC identity
Lütge et al. Nat. Immunol., 2023
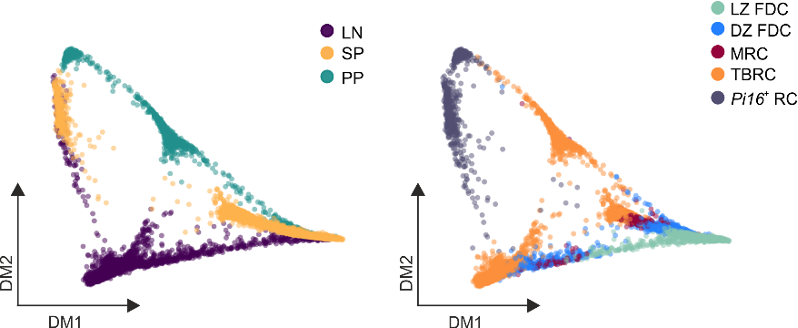
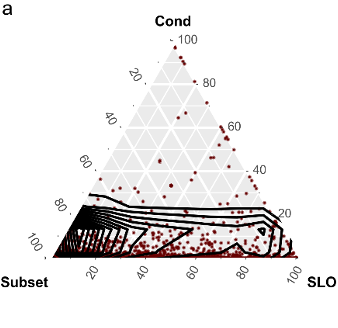
Developmental and anatomical gene sets imprint BRC identity
Lütge et al. Nat. Immunol., 2023
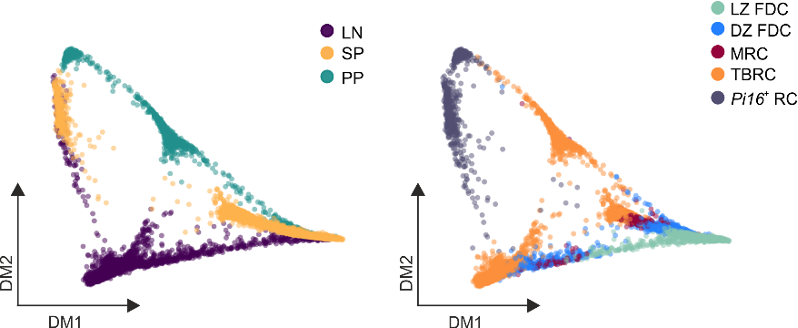
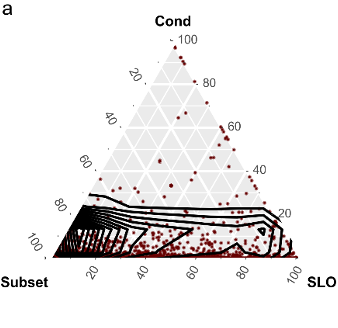
Organ
Developmental and anatomical gene sets imprint BRC identity
Lütge et al. Nat. Immunol., 2023
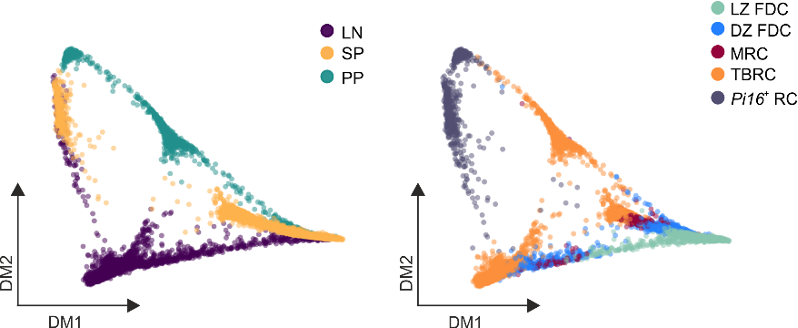
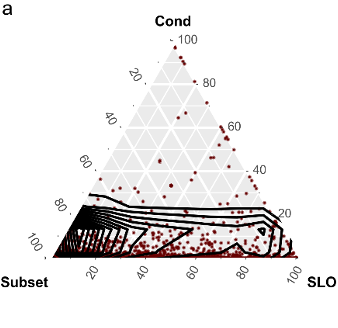
Organ
Subset identity
Developmental and anatomical gene sets imprint BRC identity
Lütge et al. Nat. Immunol., 2023
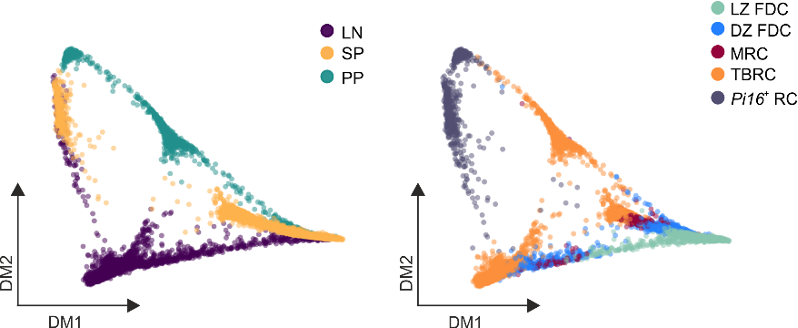
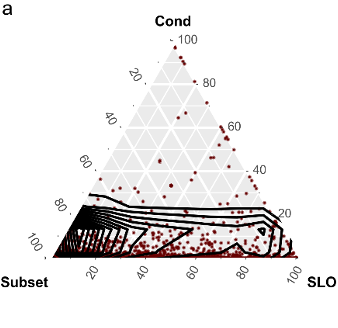
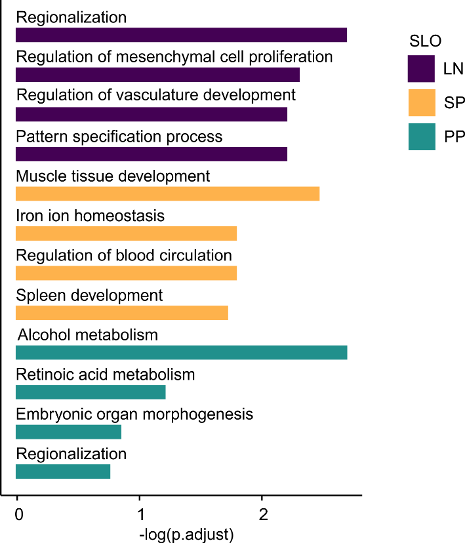
→ Organ-specific gene sets reflect developmental and anatomical imprints
Subset identity
Organ
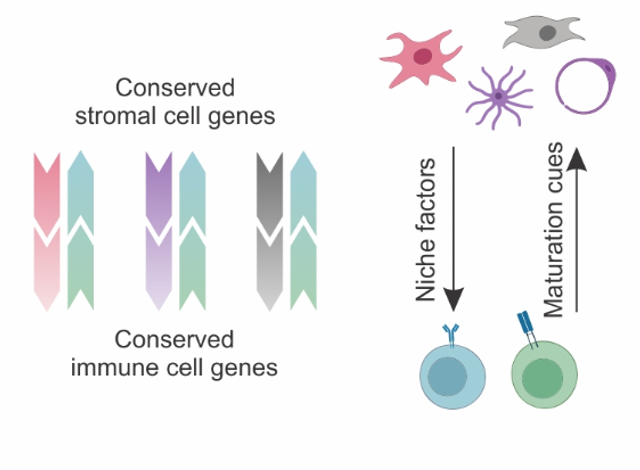
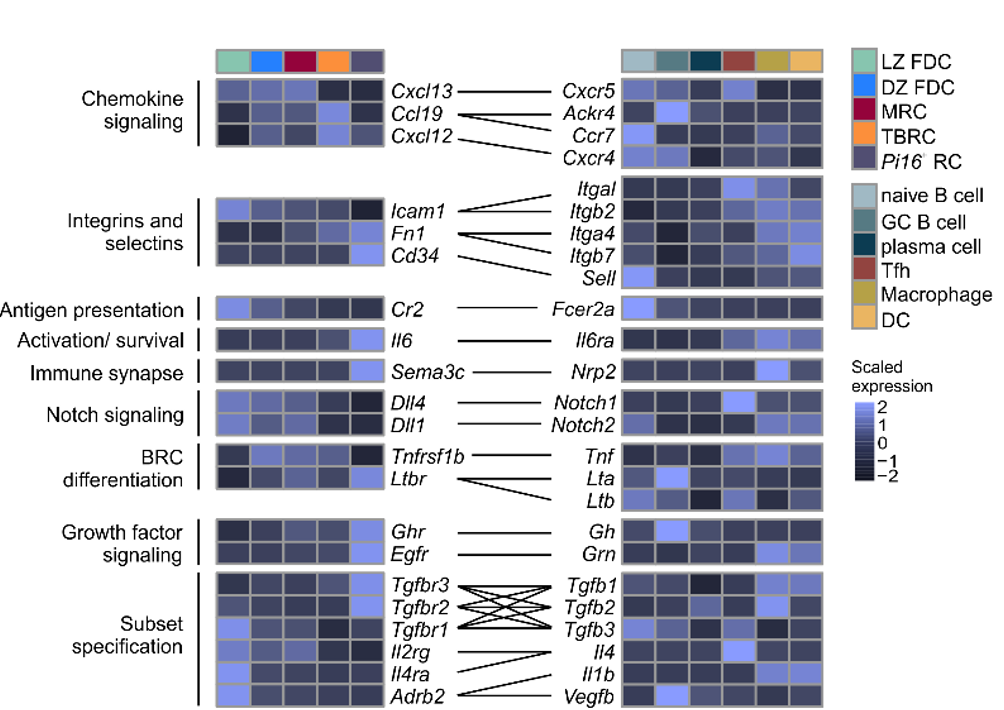
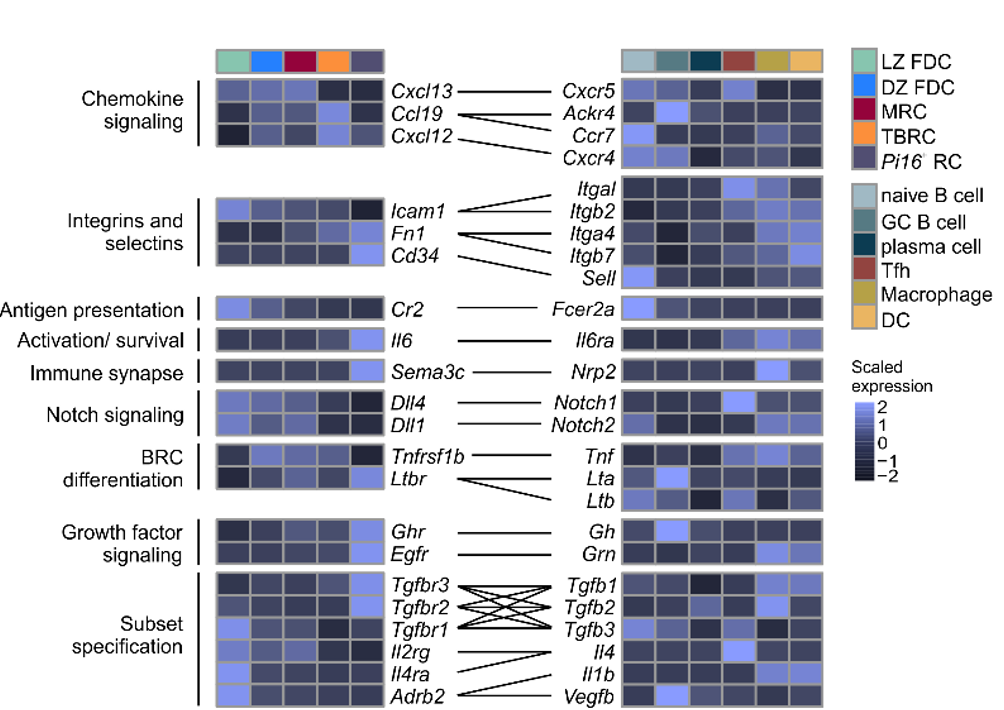
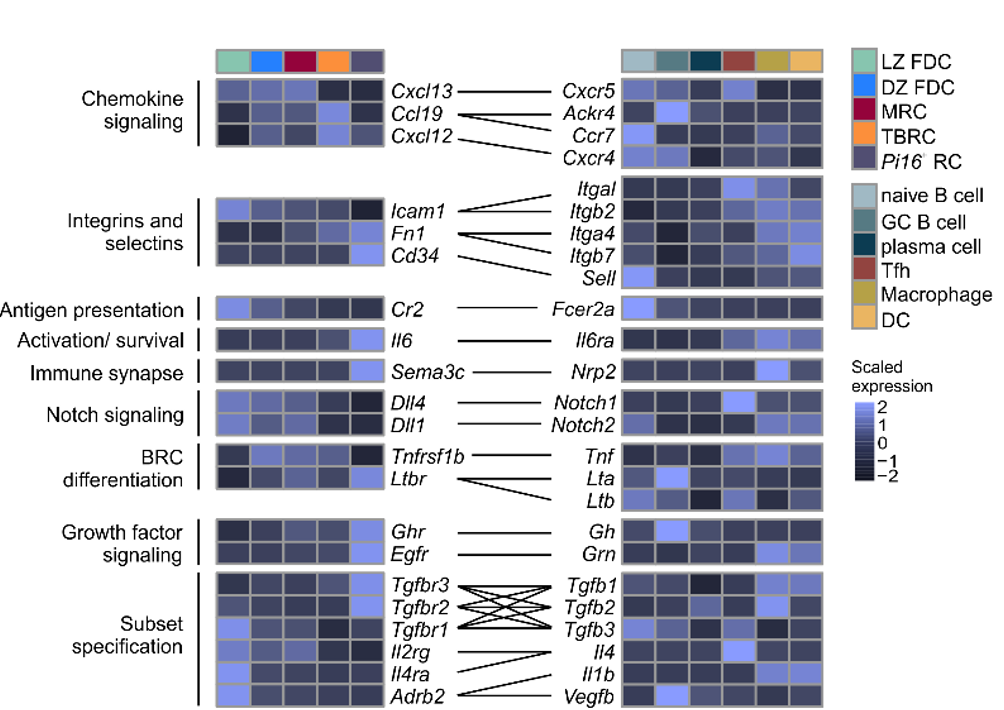
Niche factors and signaling pathways define subset identity and function
Lütge et al. Nat. Immunol., 2023
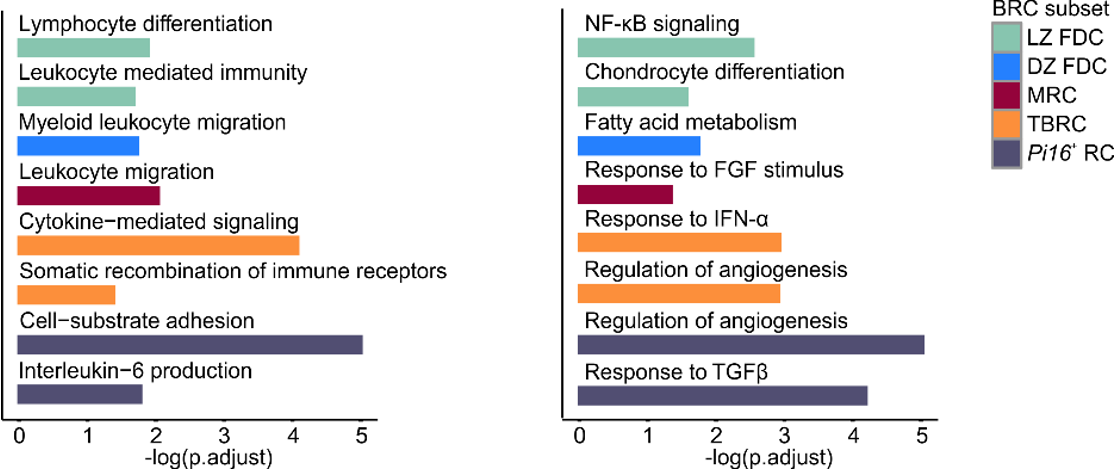
Subset-specific niche factors
Subset-specific signaling pathways
Niche factors and signaling pathways define subset identity and function
Lütge et al. Nat. Immunol., 2023
→ Subset-specific gene sets that are consistently found across SLOs point to BRC modulation by immune cells
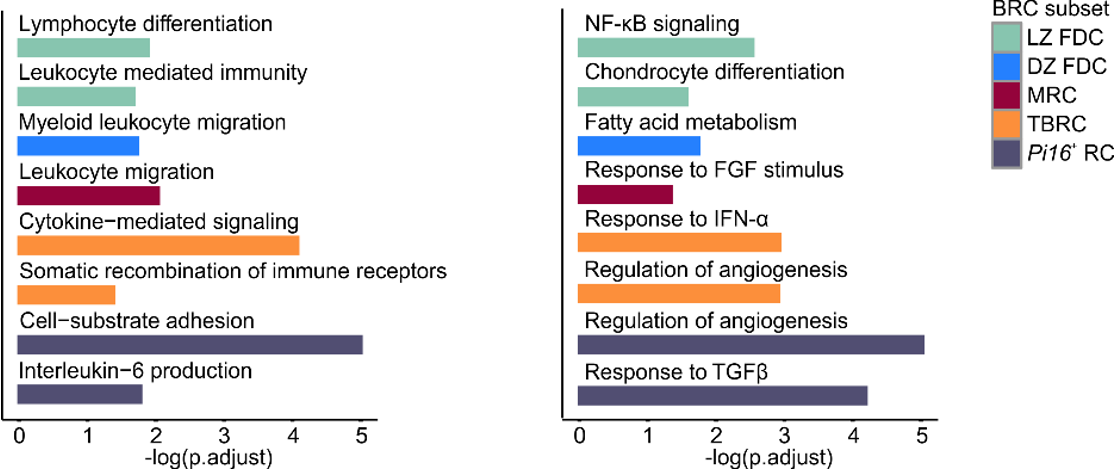
Subset-specific niche factors
Subset-specific signaling pathways
Conserved feedforward BRC-immune cell circuits sustain functional BRC niches
Lütge et al. Nat. Immunol., 2023
→ BRC-derived niche factors determine immune cell function
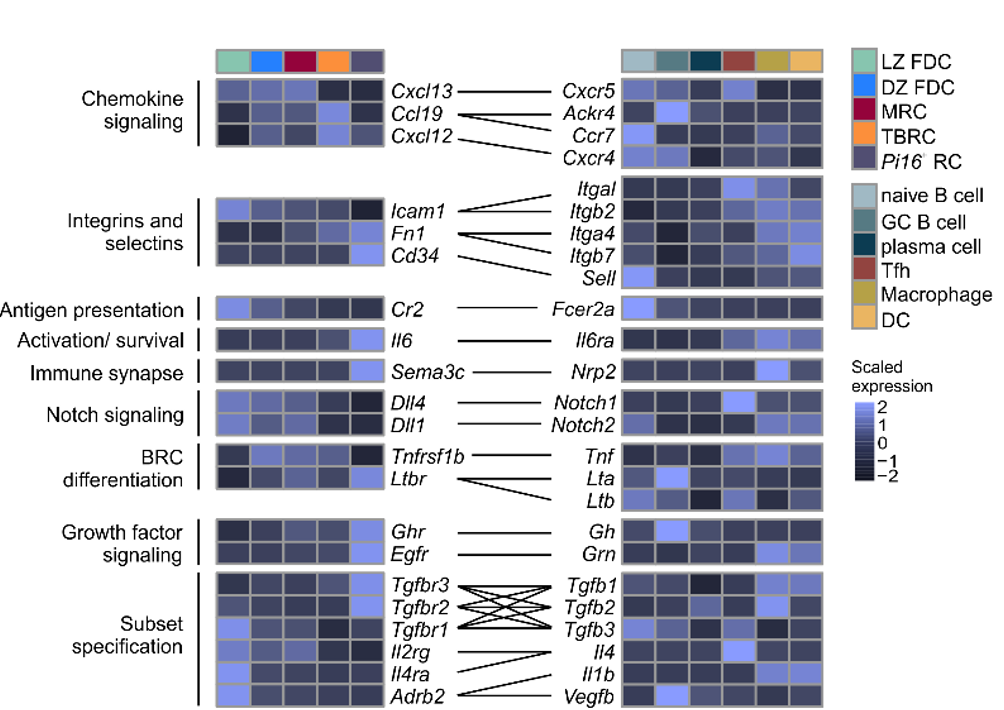
Conserved feedforward BRC-immune cell circuits sustain functional BRC niches
Lütge et al. Nat. Immunol., 2023
→ BRC-derived niche factors determine immune cell function
→ Leukocyte-derived maturation factors specify BRC subset identity
→ Conserved in humans
Conserved feedforward BRC-immune cell circuits sustain functional BRC niches
Lütge et al. Nat. Immunol., 2023
→ BRC-derived niche factors determine immune cell function
→ Leukocyte-derived maturation factors specify BRC subset identity
→ Conserved in humans
→ Validation?
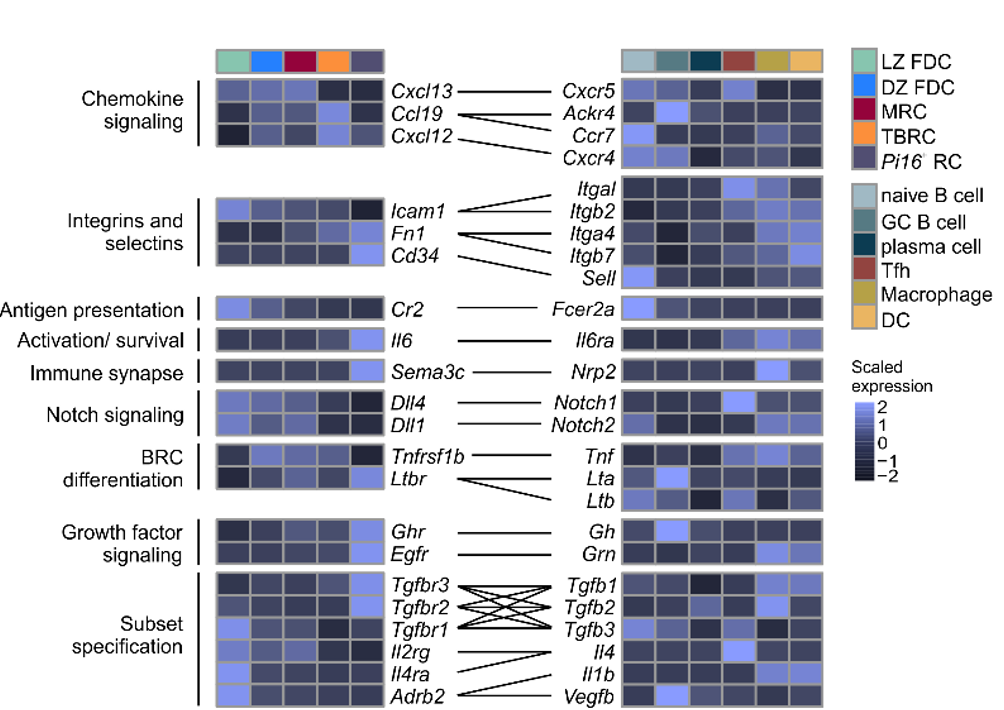
Immune cell-derived maturation cues drive BRC differentiation and activation
Lütge et al. Nat. Immunol., 2023
In-vitro stimulation of CD45-CD31-EYFP+ cells:
→ PGRN, TGFb, IL-4 and VEGF-B drive BRC differentiation
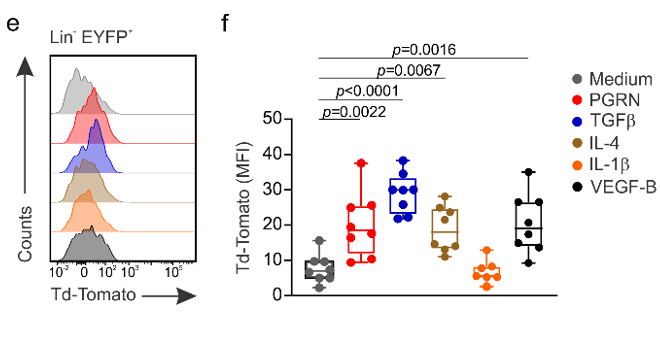
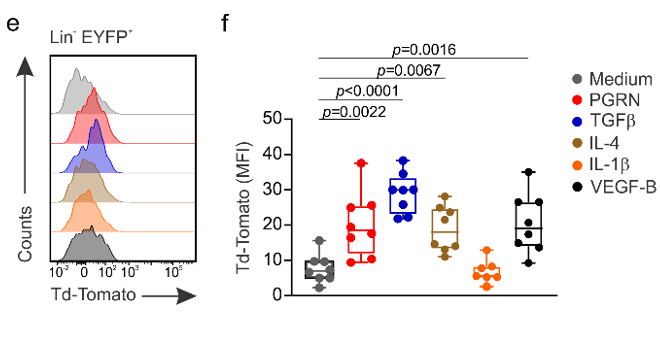
Immune cell-derived maturation cues drive BRC differentiation and activation
Lütge et al. Nat. Immunol., 2023
In-vivo stimulation of lymph node FRC:
→ IL-1b drives FDC subset specification
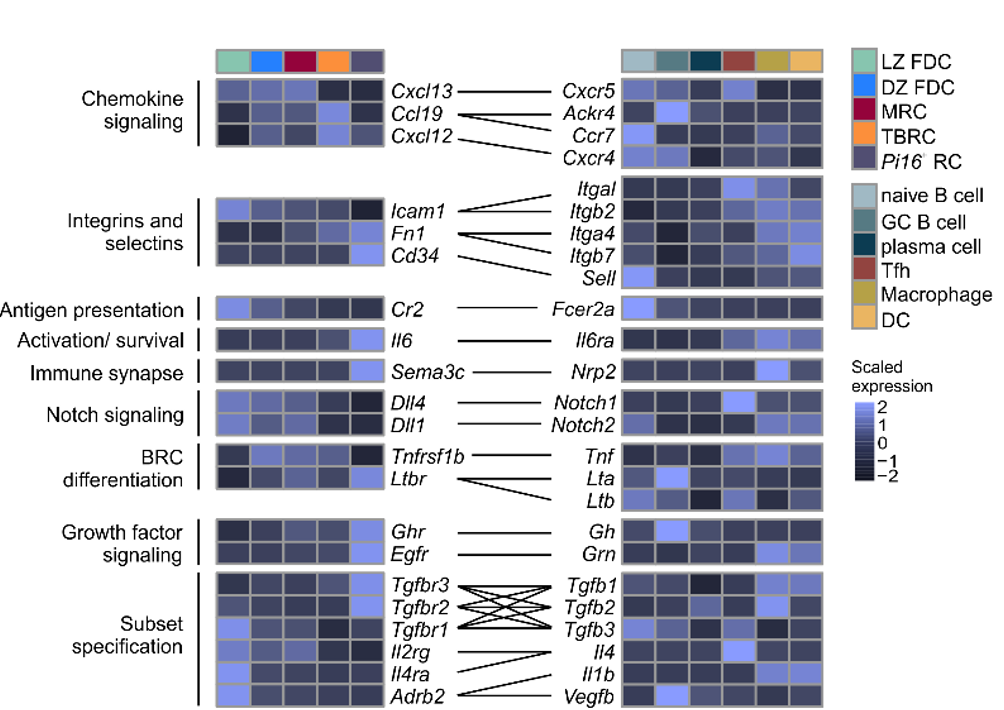
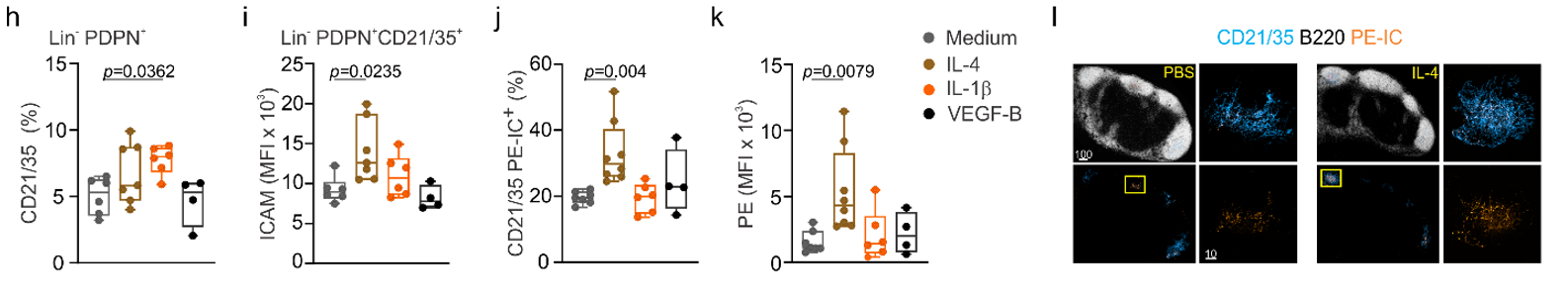
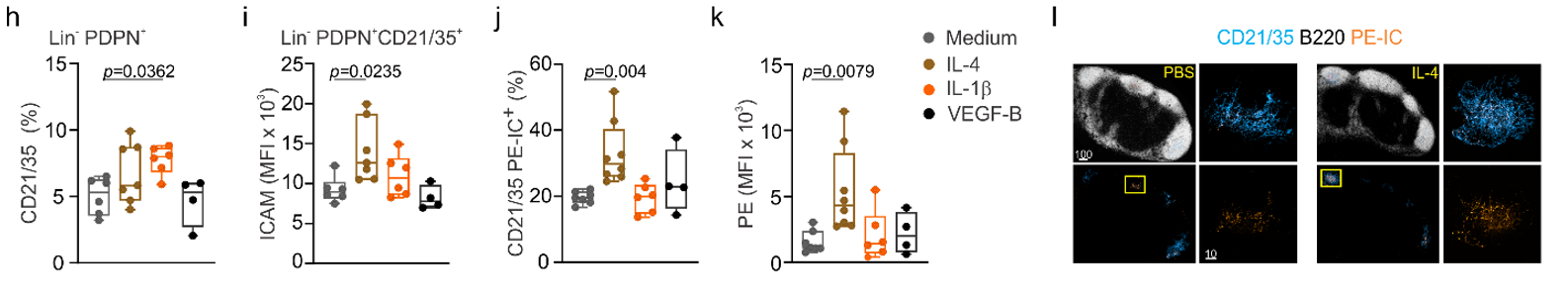
Immune cell-derived maturation cues drive BRC differentiation and activation
Lütge et al. Nat. Immunol., 2023
In-vivo stimulation of lymph node FRC:
→ IL-1b drives FDC subset specification
→ IL-4 shapes FDC function and activation
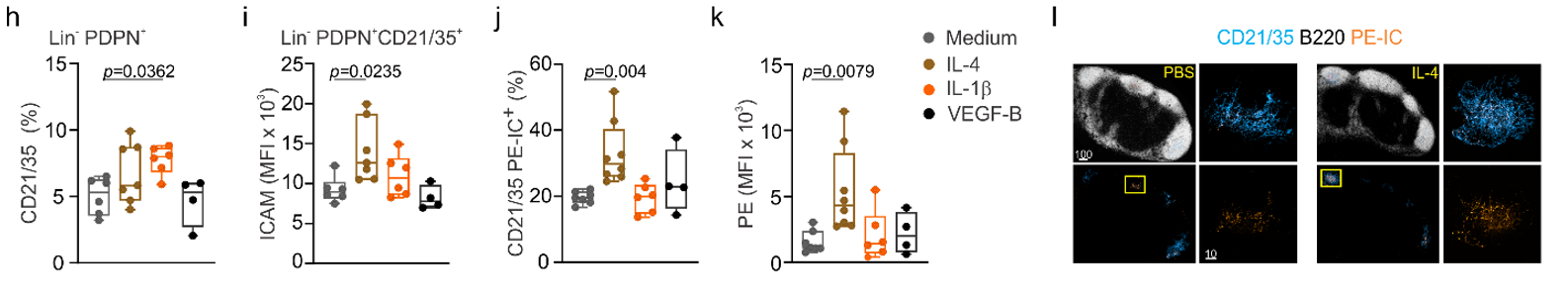
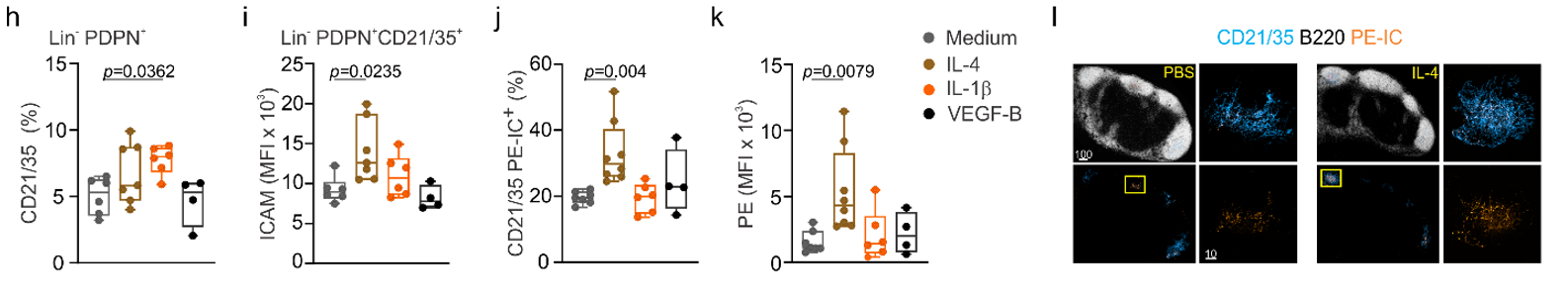
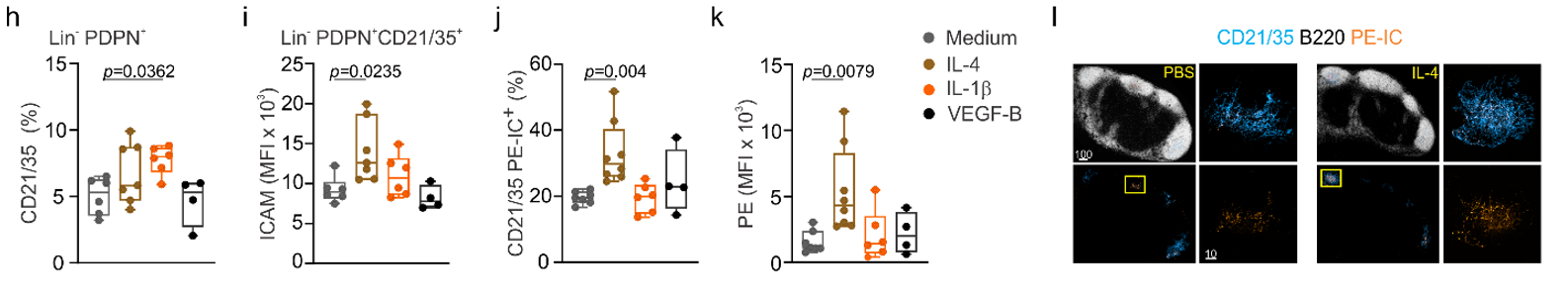
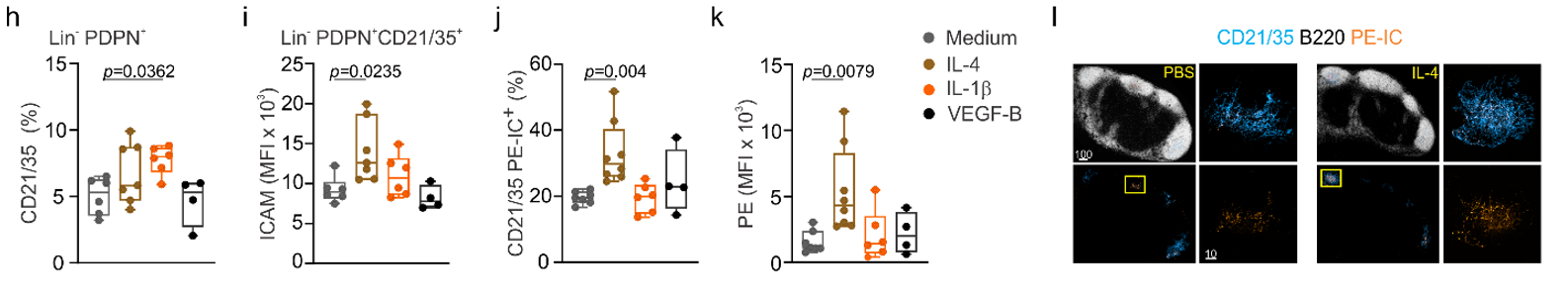
Immune cell-derived maturation cues drive BRC differentiation and activation
Lütge et al. Nat. Immunol., 2023
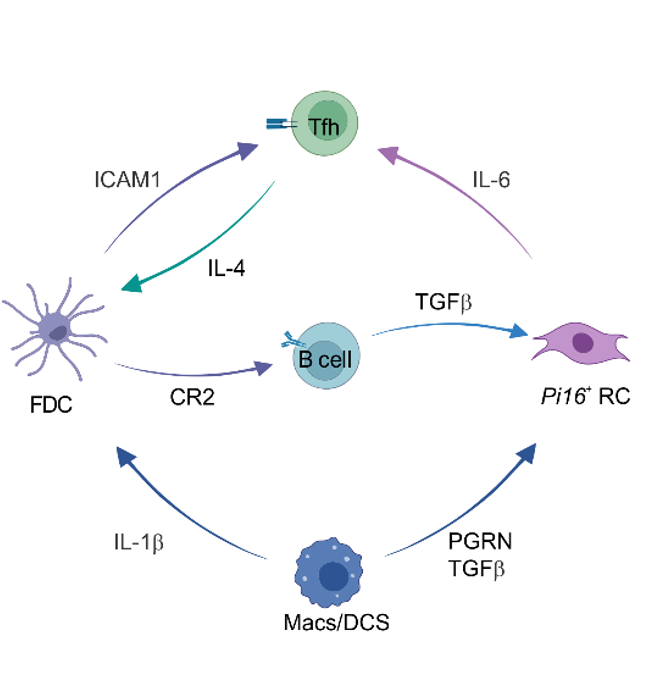
FDC
B cell
PI16+RC
Mph/DC
T cell
Immune cell-derived maturation cues drive BRC differentiation and activation
Lütge et al. Nat. Immunol., 2023
FDC
B cell
PI16+RC
Mph/DC
T cell
CR2
ICAM1
IL6
Immune cell-derived maturation cues drive BRC differentiation and activation
Lütge et al. Nat. Immunol., 2023
CR2
IL1b
IL4
ICAM1
TGFb
PGRN
TGFb
FDC
B cell
PI16+RC
Mph/DC
T cell
IL6
Immune cell-derived maturation cues drive BRC differentiation and activation
Lütge et al. Nat. Immunol., 2023
Summary - 1: Advanced understanding of systemic humoral immunity
Lütge et al. Nat. Immunol., 2023
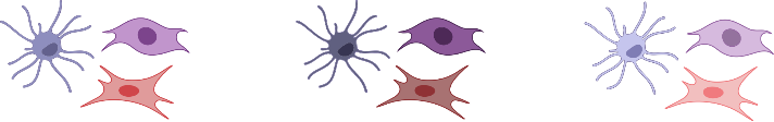
Lymph node
Spleen
Peyer's patch
Organ-specific imprints
Summary - 1: Advanced understanding of systemic humoral immunity
Lütge et al. Nat. Immunol., 2023
Lymph node
Spleen
Peyer's patch
Organ-specific imprints
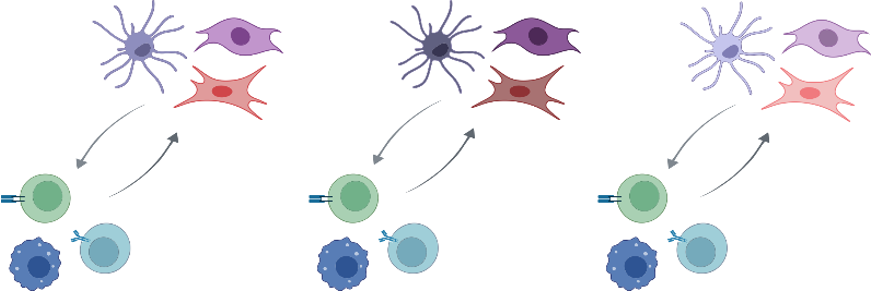
Functional convergence
Summary - 1: Advanced understanding of systemic humoral immunity
Lütge et al. Nat. Immunol., 2023
Lymph node
Spleen
Peyer's patch
Organ-specific imprints
Functional convergence
Feedforward paradigm: circulating immune cell imprint B cell follicle niches in an organ indiscriminate manner thereby securing efficient systemic humoral immunity
Fibroblastic reticular cells orchestrate SLO organization

To what extend are FRC underpinned niches functionally conserved across:
(1.) SLOs?
(2.) Species?
(3.) Activation?
→ What factors shape FRC subset identity and function?
Fibroblastic reticular cells orchestrate SLO organization

To what extend are FRC underpinned niches functionally conserved across:
(1.) SLOs?
(2.) Species?
(3.) Activation?
→ What factors shape FRC subset identity and function?
Fibroblastic reticular cells orchestrate SLO organization
- Conserved stromal–immune cell circuits secure B cell homeostasis and function
- PI16+ reticular cells form reactive immune cell niches in human lymph nodes
Repeated lymph node expansion and contraction throughout life
- Rapid expansion allows massive lymphocyte entry and proliferation
- Structural and functional tissue integrity is preserved
- FRC stretching and proliferation regulate network tension
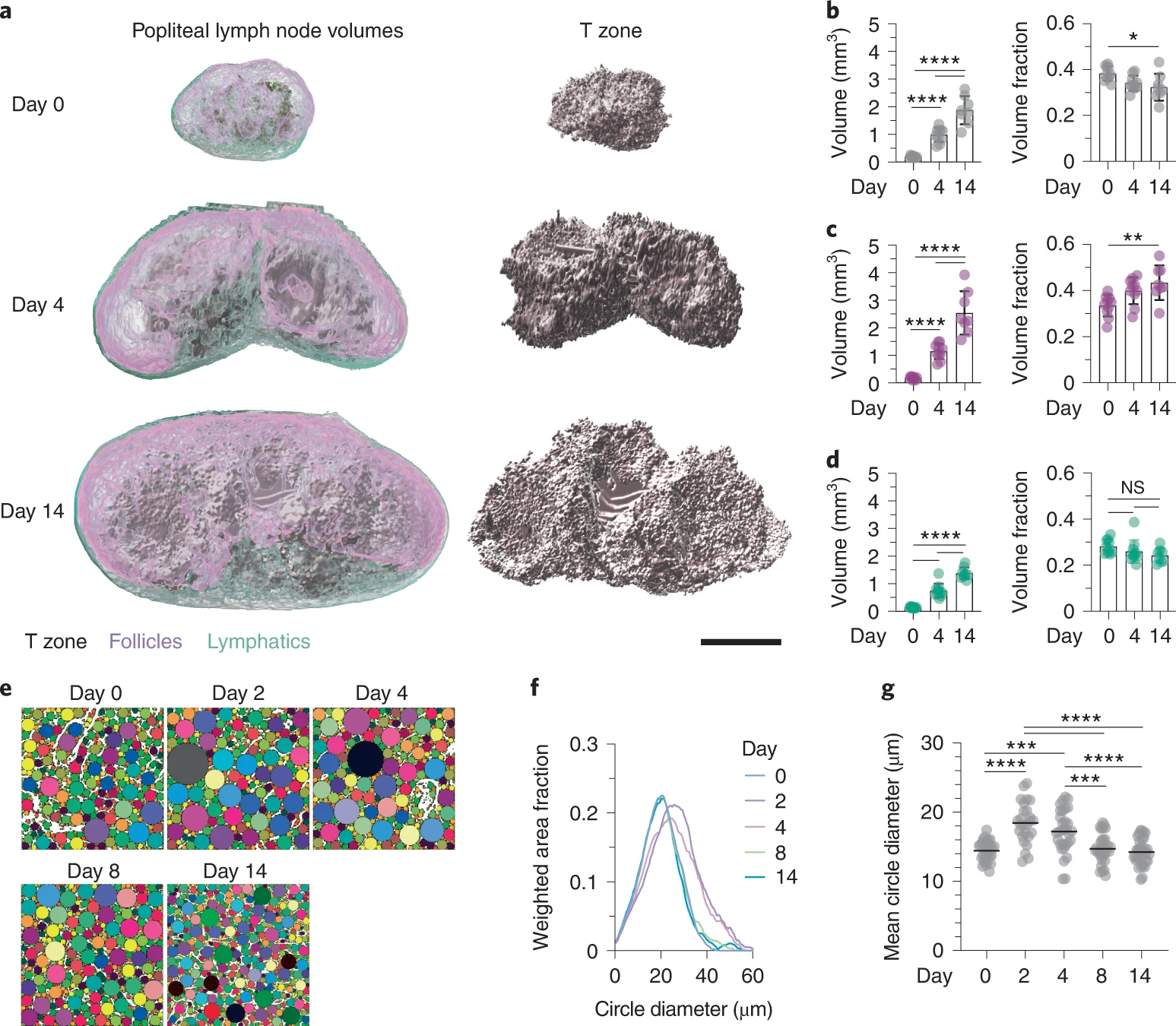
Assen et al. Nat. Immunol., 2022
Repeated lymph node expansion and contraction throughout life
- Rapid expansion allows massive lymphocyte entry and proliferation
- Structural and functional tissue integrity is preserved
- FRC stretching and proliferation regulate network tension
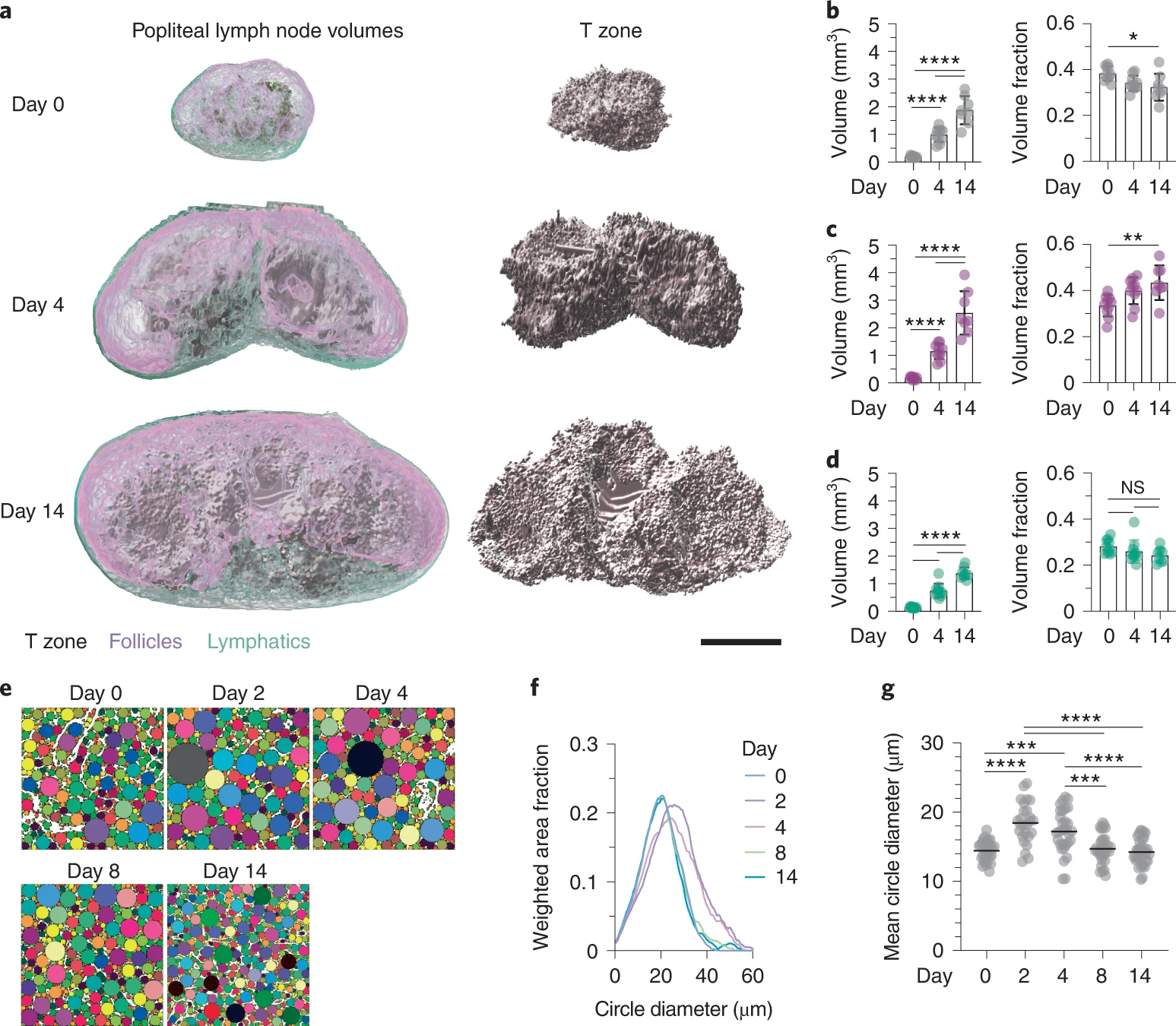
Assen et al. Nat. Immunol., 2022
→ How does repeated expansion and contraction in response to immunological stimuli shape the FRC network in human lymph nodes?
The FRC landscape in human palatine tonsils
-
No marginal zone reticular cells (MRCs) in palatine tonsils; antigen sampling occurs in the “reticulated” epithelium
De Martin et al. Nat. Immunol., 2023
The FRC landscape in human palatine tonsils
-
No marginal zone reticular cells (MRCs) in palatine tonsils; antigen sampling occurs in the “reticulated” epithelium
-
Subepithelial PI16+ reticular cells form a distinct niche show the strongest inflammation induced remodeling
-
PI16+ reticular cells integrate immune cell-derived signals and govern T cell activation
De Martin et al. Nat. Immunol., 2023
The FRC landscape in human palatine tonsils
-
No marginal zone reticular cells (MRCs) in palatine tonsils; antigen sampling occurs in the “reticulated” epithelium
-
Subepithelial PI16+ reticular cells form a distinct niche show the strongest inflammation induced remodeling
-
PI16+ reticular cells integrate immune cell-derived signals and govern T cell activation
De Martin et al. Nat. Immunol., 2023
→ How does inflammatory activation affect the human lymph node FRC landscape? Are PI16+ RCs involved in inflammatory reactions of human lymph nodes?
Repeated lymph node expansion and contraction throughout life
- Rapid expansion allows massive lymphocyte entry and proliferation
- Structural and functional tissue integrity is preserved
- FRC stretching and proliferation regulate network tension
→ How does repeated expansion and contraction in response to immunological stimuli shape the FRC network in human lymph nodes?
→ Stereotypic "resting" lymph node?
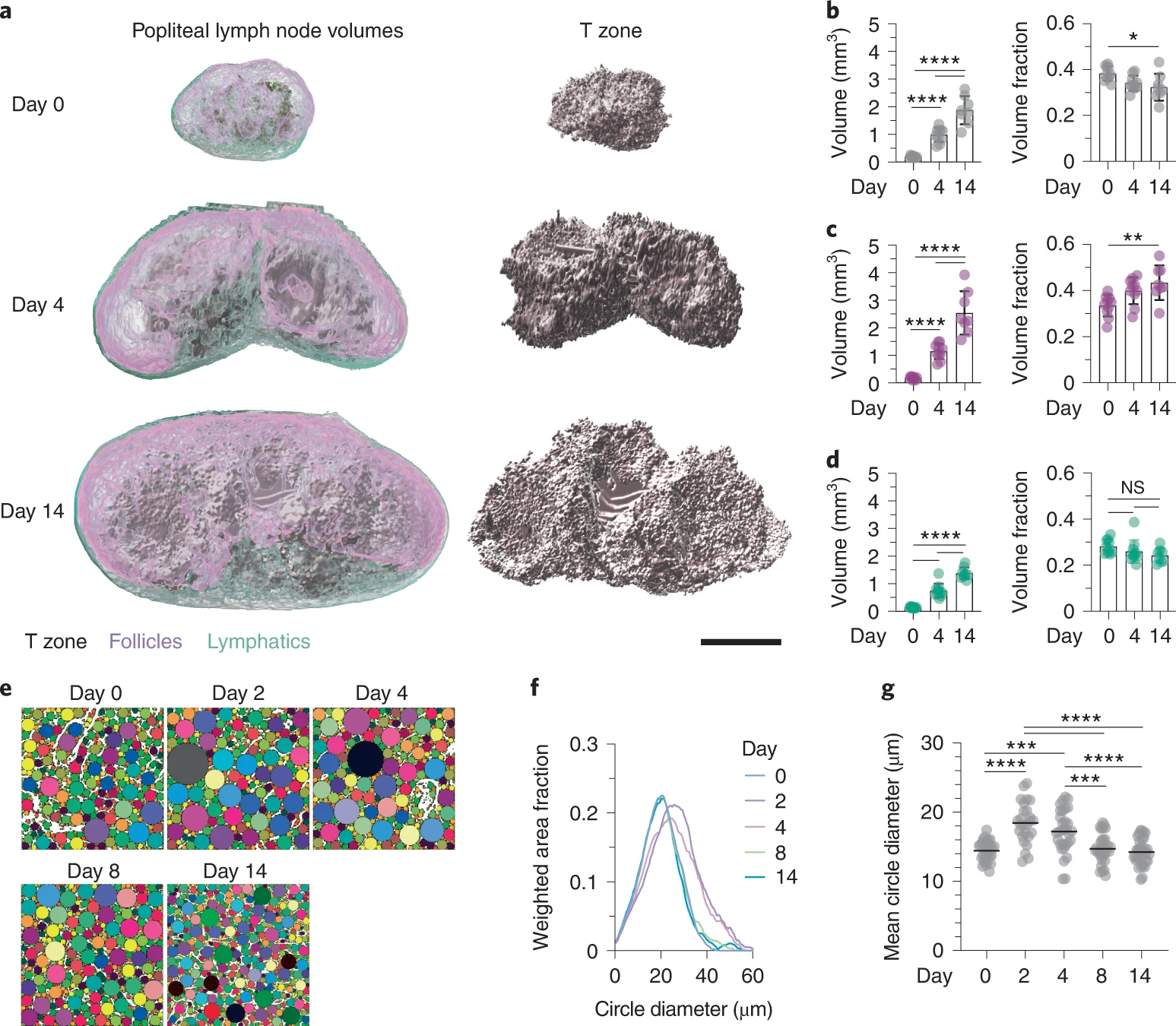
Assen et al. Nat. Immunol., 2022
The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023
The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023
-
Distinct FRC subsets similar to murine SLOs (except MRCs)
The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023

-
Distinct FRC subsets similar to murine SLOs (except MRCs)
-
Antigen sampling occurs in the “reticulated” epithelium
De Martin et al. J Exp Med., 2024
The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023

-
Distinct FRC subsets similar to murine SLOs (except MRCs)
-
Antigen sampling occurs in the “reticulated” epithelium
-
Subepithelial PI16+ reticular cells form a distinct niche show the strongest inflammation induced remodeling
De Martin et al. J Exp Med., 2024
The FRC landscape in human palatine tonsils

-
Distinct FRC subsets similar to murine SLOs (except MRCs)
-
Antigen sampling occurs in the “reticulated” epithelium
-
Subepithelial PI16+ reticular cells form a distinct niche show the strongest inflammation induced remodeling
-
PI16+ reticular cells integrate immune cell-derived signals and govern T cell activation
De Martin et al. J Exp Med., 2024

The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023

The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023

The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023
-
Distinct FRC subsets similar to murine SLOs (except MRCs)

The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023
-
Distinct FRC subsets similar to murine SLOs (except MRCs)
-
Antigen sampling occurs in the “reticulated” epithelium

The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023
-
Distinct FRC subsets similar to murine SLOs (except MRCs)
-
Antigen sampling occurs in the “reticulated” epithelium

The FRC landscape in human palatine tonsils
De Martin et al. Nat. Immunol., 2023
-
Distinct FRC subsets similar to murine SLOs (except MRCs)
-
Antigen sampling occurs in the “reticulated” epithelium
-
Subepithelial PI16+ reticular cells form a distinct niche show the strongest inflammation induced remodeling

De Martin et al. J Exp Med., 2024
The FRC landscape in human palatine tonsils

De Martin et al. J Exp Med., 2024

-
Distinct FRC subsets similar to murine SLOs (except MRCs)
-
Antigen sampling occurs in the “reticulated” epithelium
-
Subepithelial PI16+ reticular cells form a distinct niche show the strongest inflammation induced remodeling
-
PI16+ reticular cells integrate immune cell-derived signals and govern T cell activation
Objectives
→ Characterization of the FRC landscape in a stereotypic "resting" human lymph node
Objectives
→ Characterization of the FRC landscape in a stereotypic "resting" human lymph node
→ How does inflammatory activation affect the human lymph node FRC landscape?
Objectives
→ Characterization of the FRC landscape in a stereotypic "resting" human lymph node
→ How does inflammatory activation affect the human lymph node FRC landscape?
→ Are PI16+ RCs involved in inflammatory reactions of human lymph nodes?
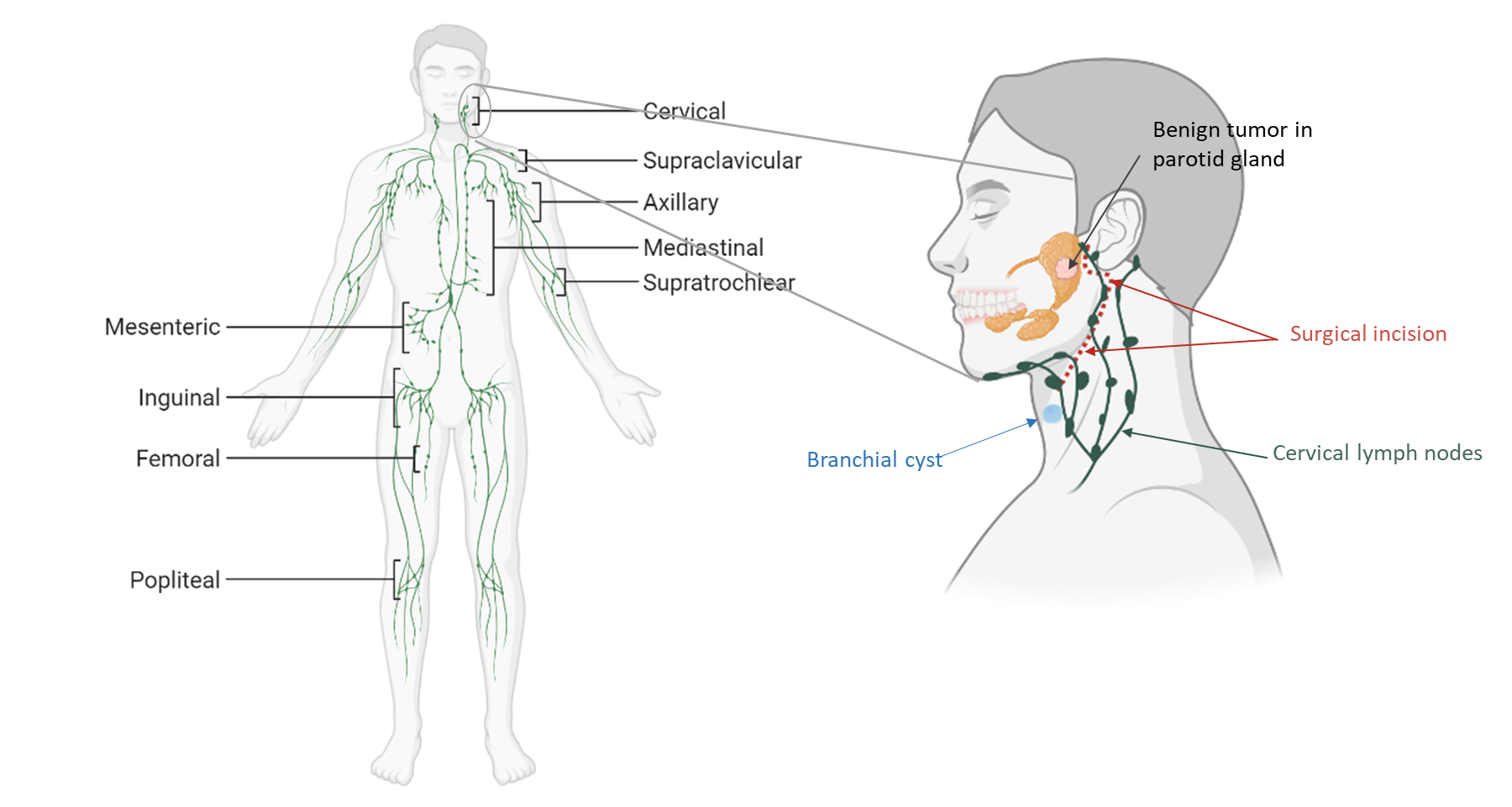
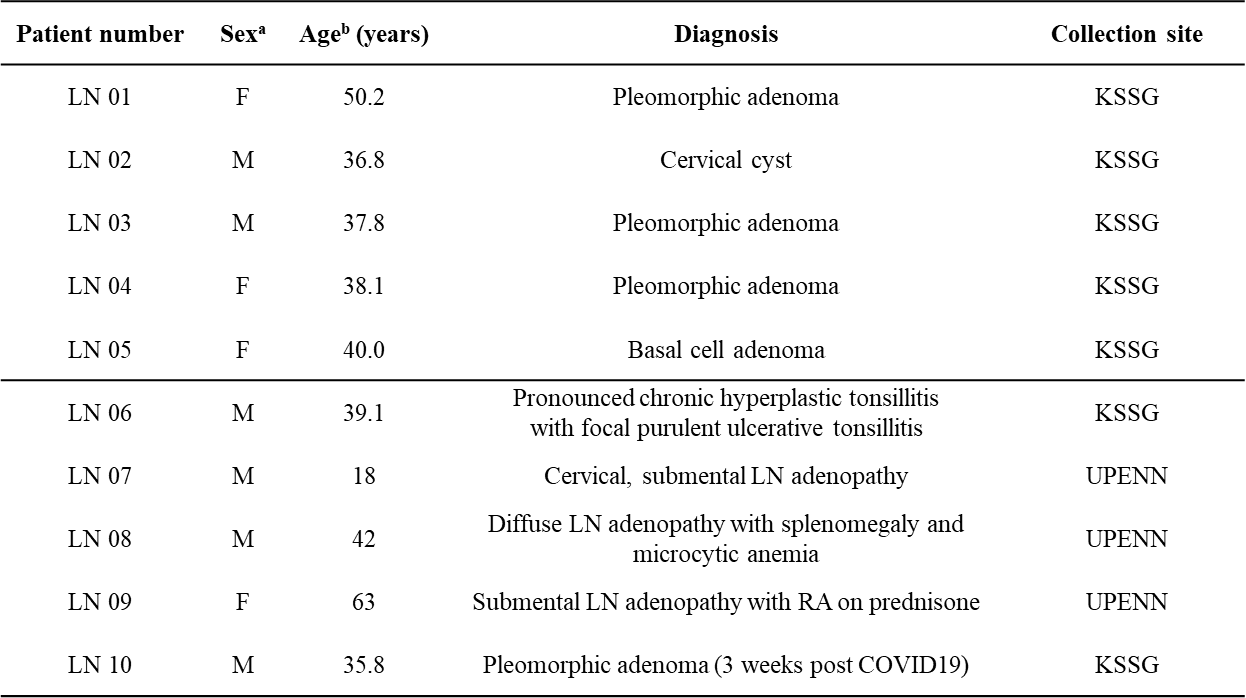
Patient cohort – clinically non-inflamed ("resting") cervical lymph nodes
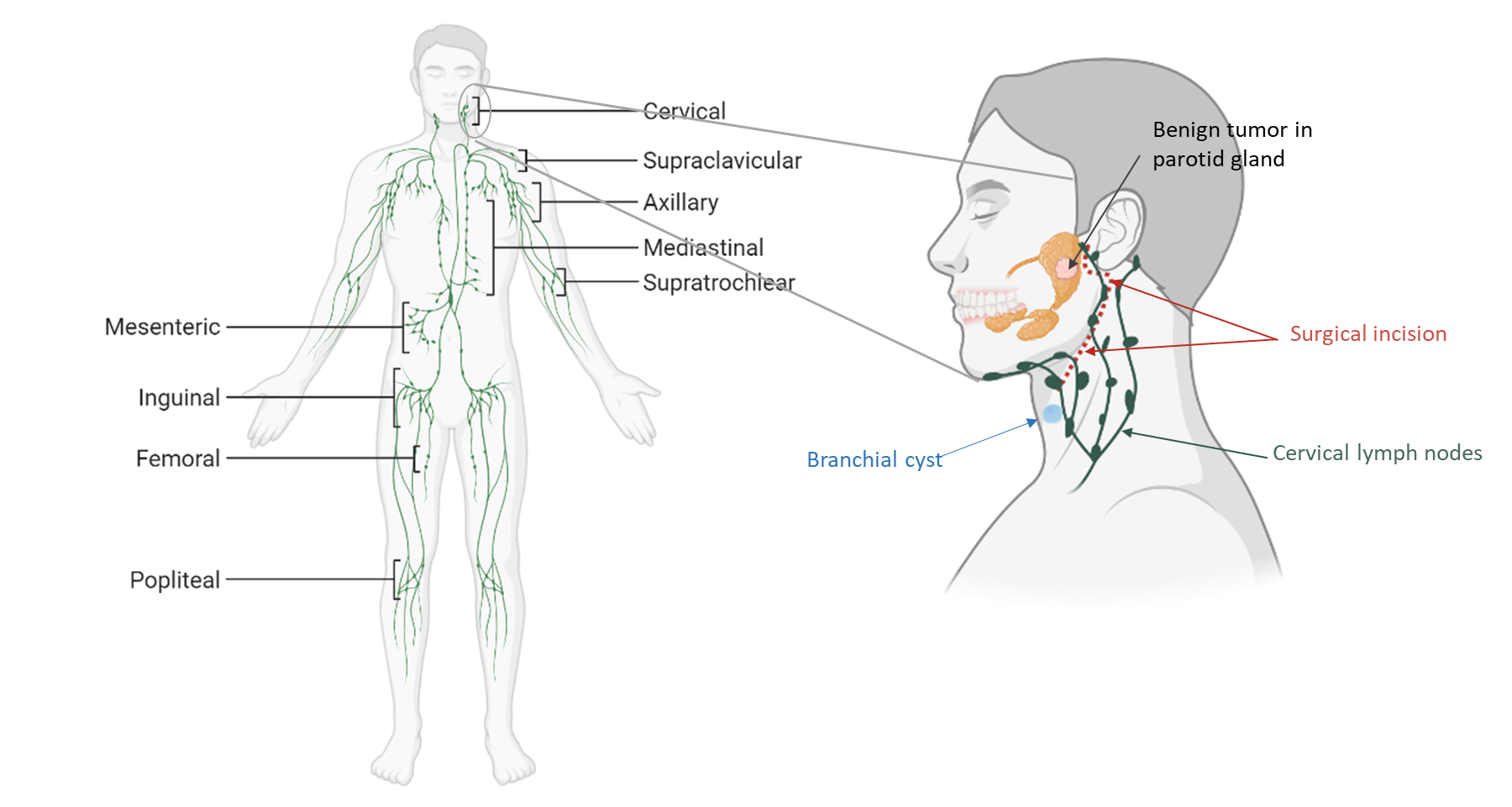
Objectives
→ Characterization of the FRC landscape in a stereotypic "resting" human lymph node
→ How does inflammatory activation affect the human lymph node FRC landscape?
→ Are PI16+ RCs involved in inflammatory reactions of human lymph nodes?
Objectives
→ Characterization of the FRC landscape in a stereotypic "resting" human lymph node
→ How does inflammatory activation affect the human lymph node FRC landscape?
→ Are PI16+ RCs involved in inflammatory reactions of human lymph nodes?
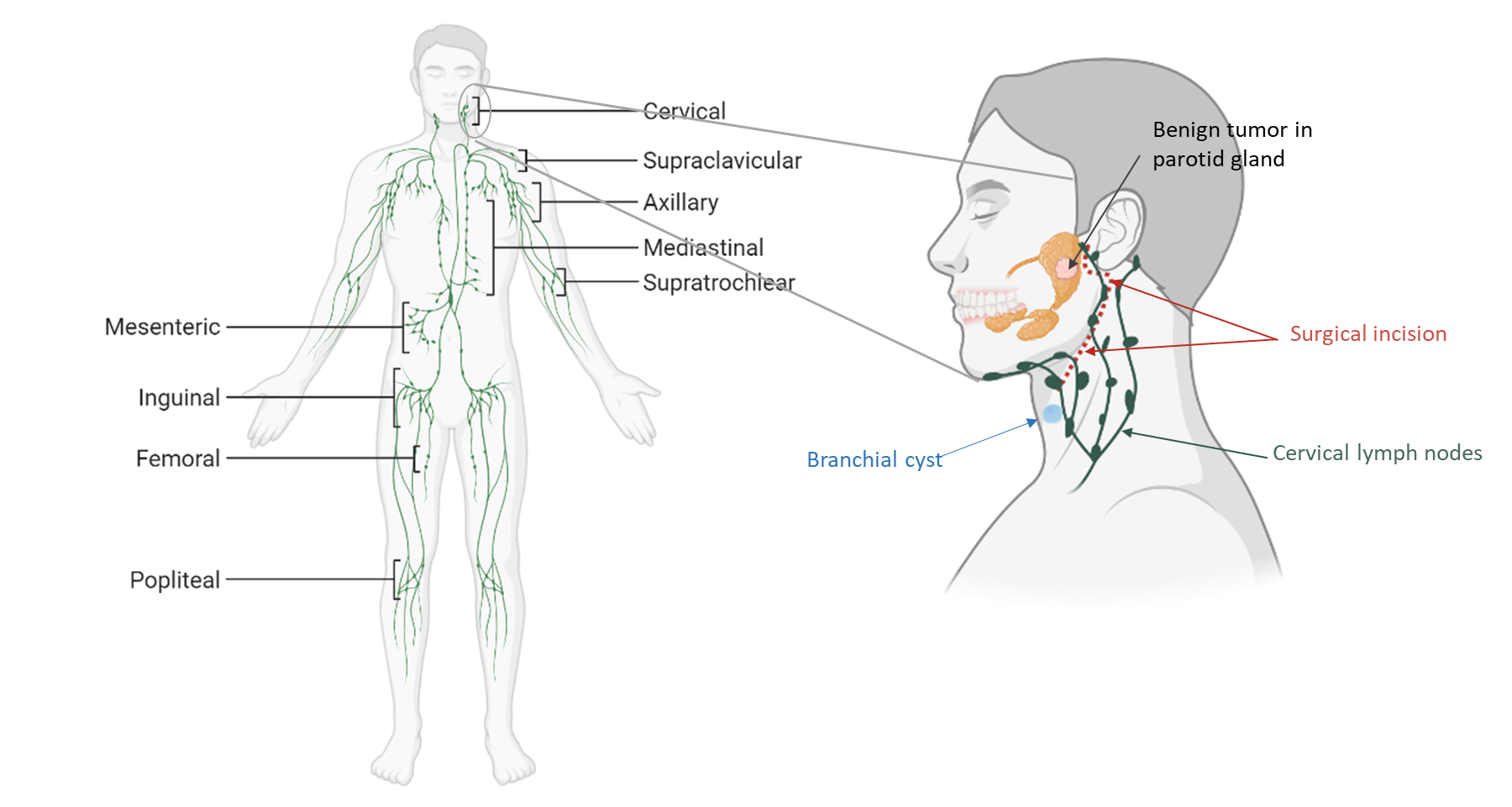
- Resting:
clinically not inflamed lymph nodes from patients with benign tumors
Objectives
→ Characterization of the FRC landscape in a stereotypic "resting" human lymph node
→ How does inflammatory activation affect the human lymph node FRC landscape?
→ Are PI16+ RCs involved in inflammatory reactions of human lymph nodes?
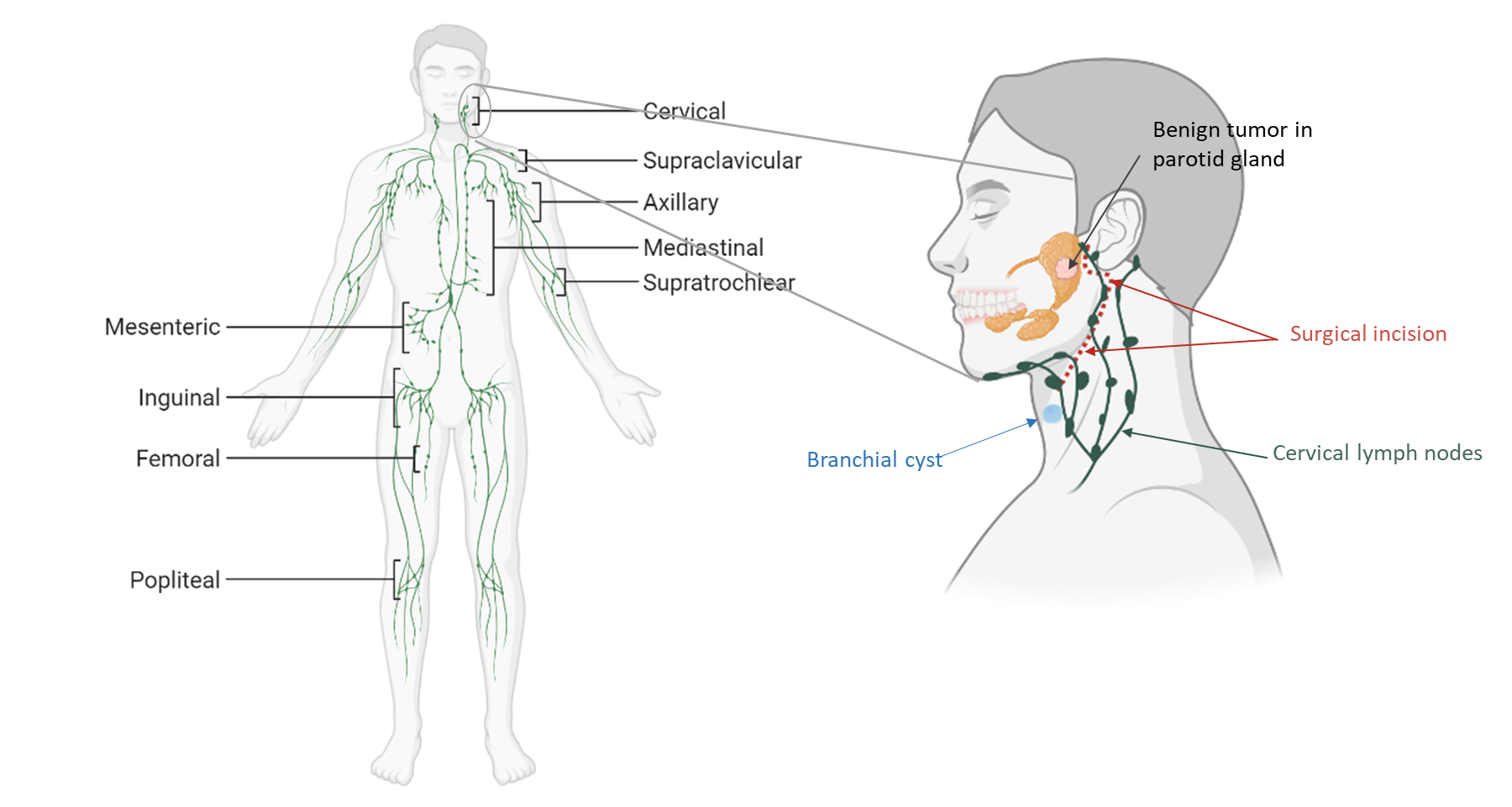
- Resting:
- Activated:
clinically not inflamed lymph nodes from patients with benign tumors
acute or chronically inflamed lymph nodes
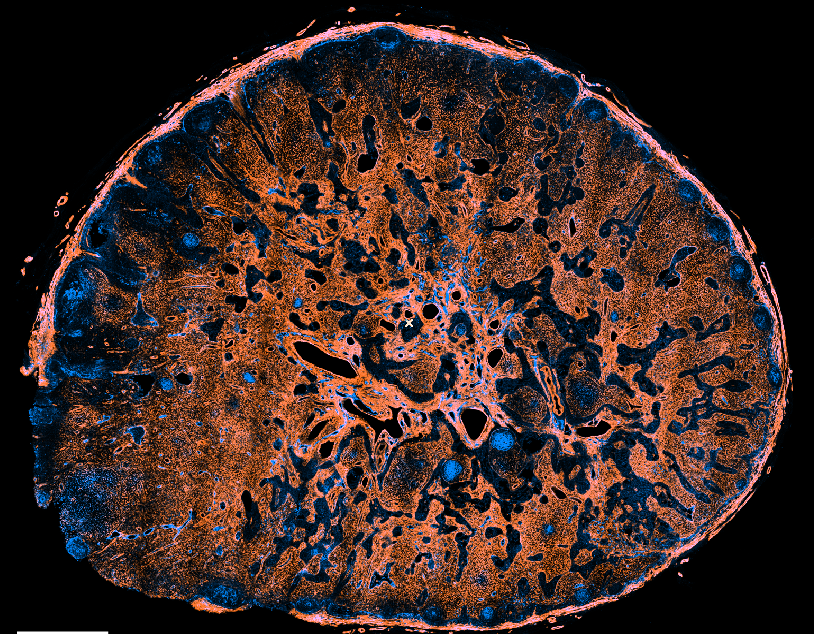
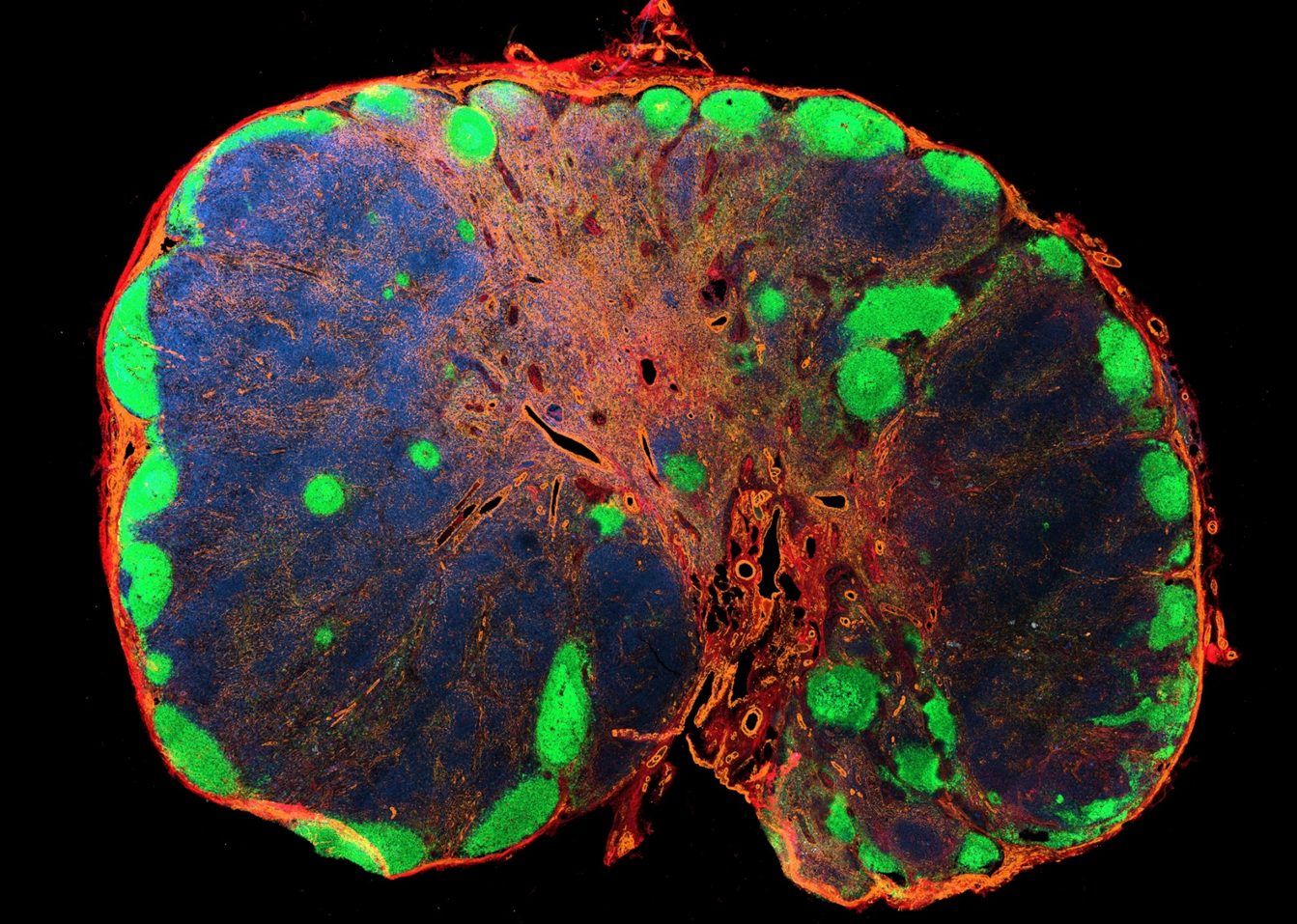
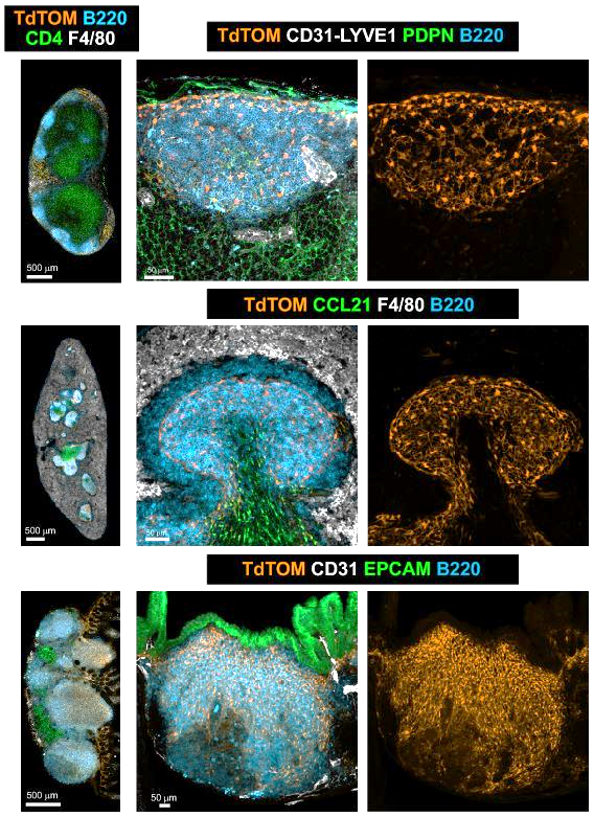
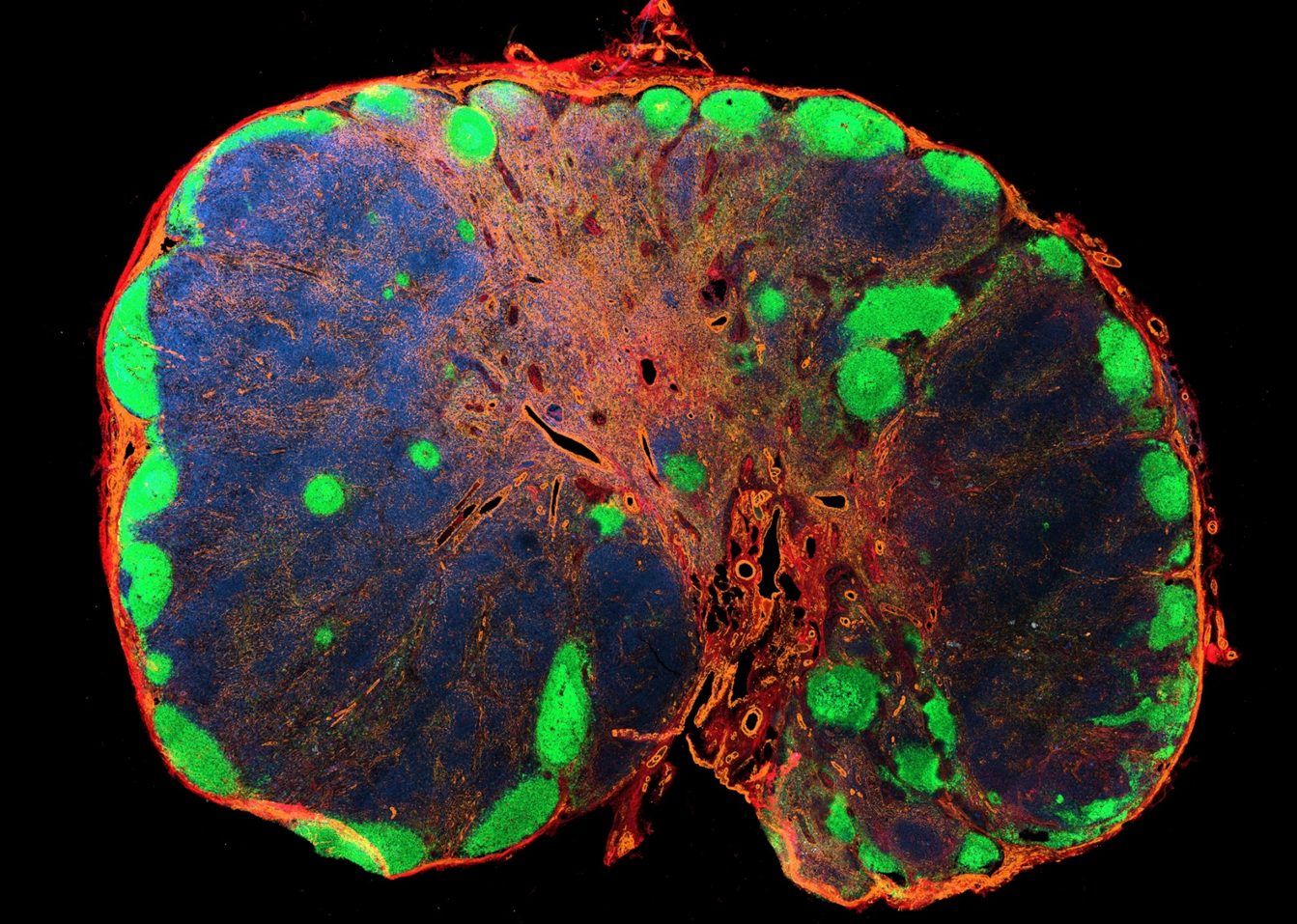
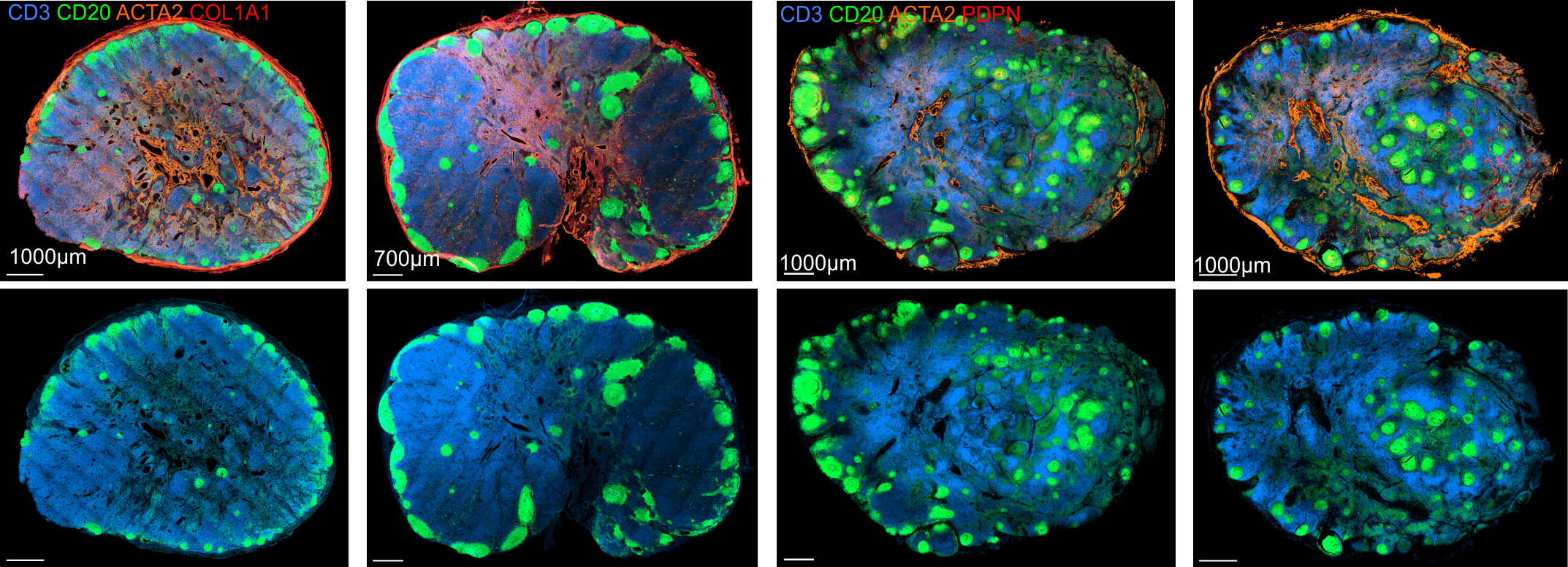
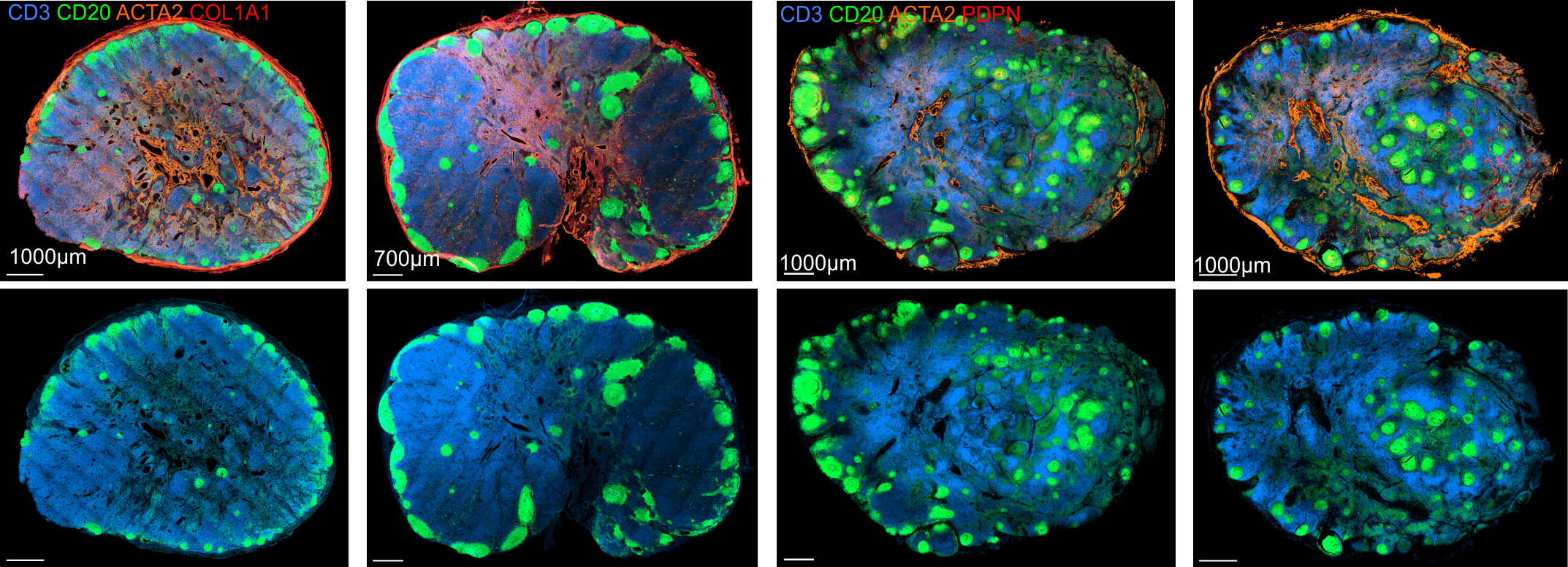
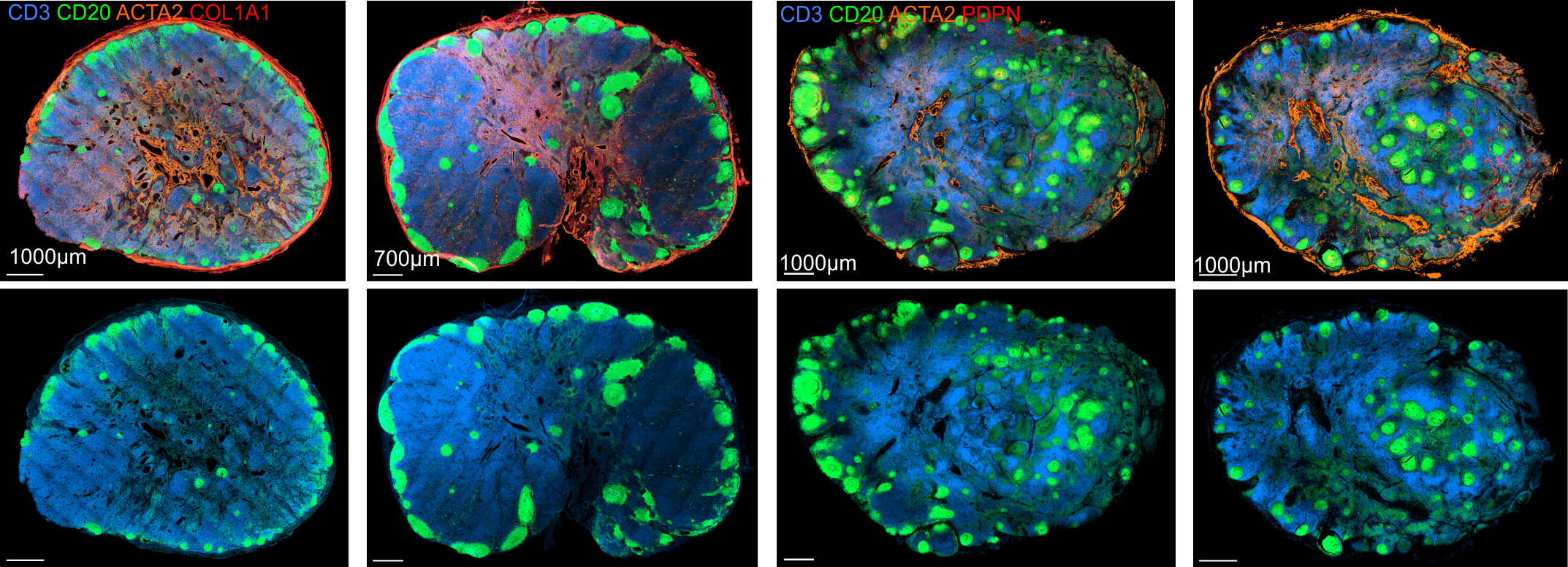
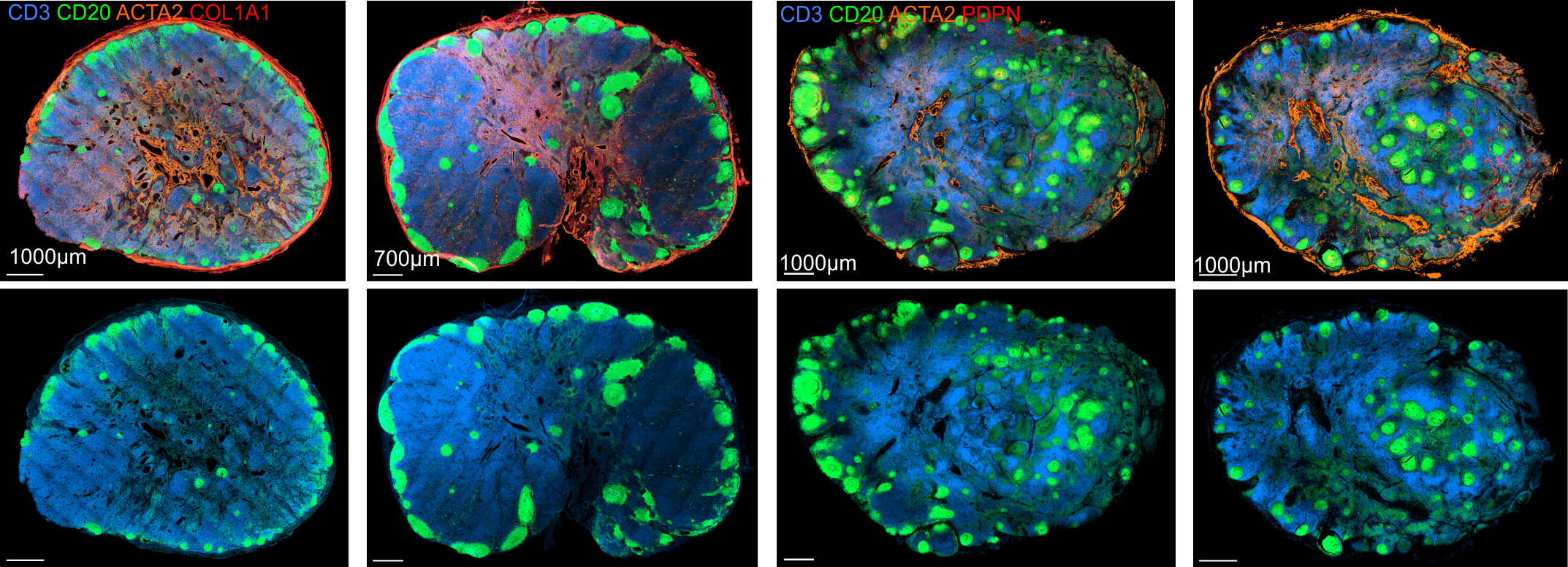
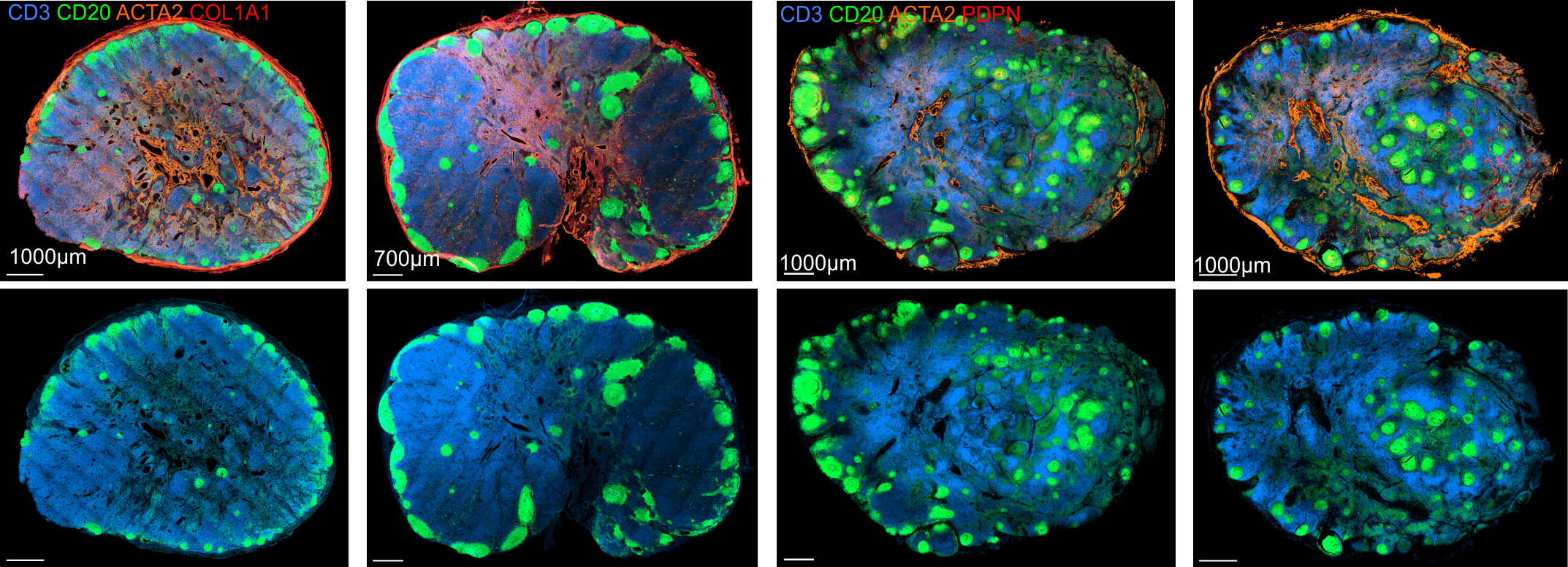
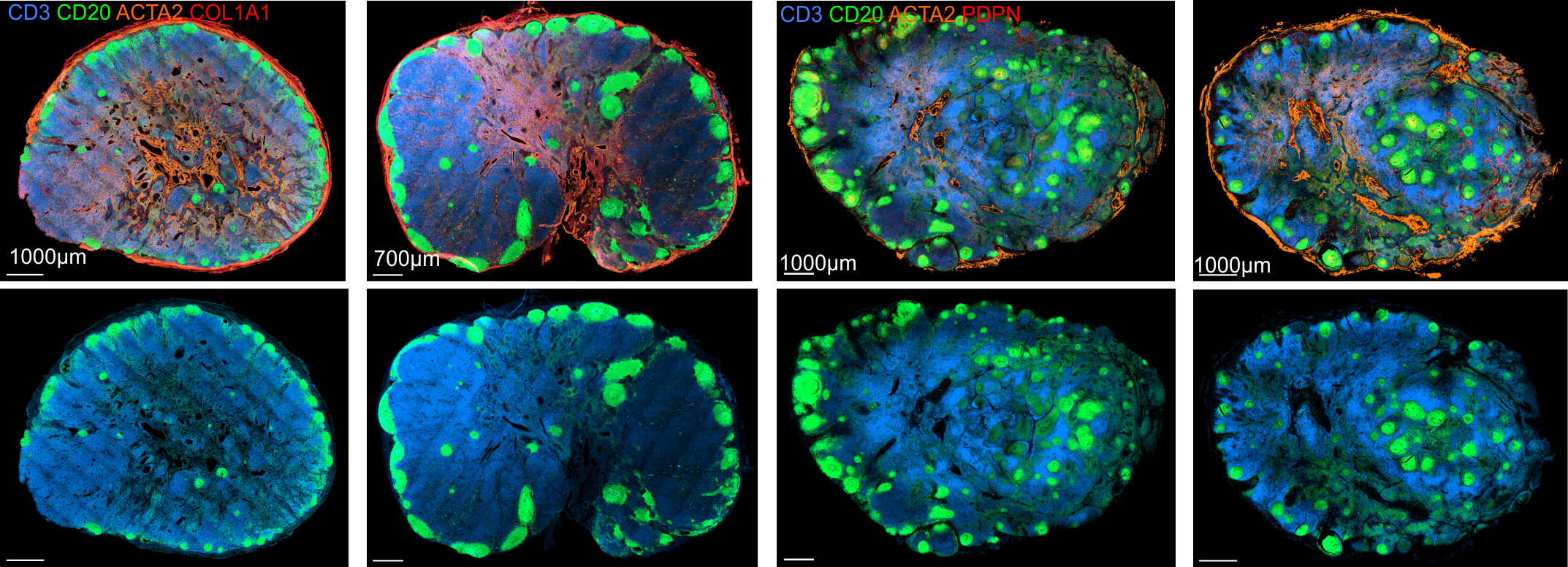
Immunoanatomy of resting human lymph nodes

CD20: B cells
CD3: T cells
ACTA2: Vascular smooth muscle cells/FRCs
-
large T cell zone
Immunoanatomy of resting human lymph nodes

CD20: B cells
CD3: T cells
ACTA2: Vascular smooth muscle cells/FRCs
-
large T cell zone
-
multiple lymph node lobules
Immunoanatomy of resting human lymph nodes

CD20: B cells
CD3: T cells
ACTA2: Vascular smooth muscle cells/FRCs
-
large T cell zone
-
multiple lymph node lobules
-
atypical positioning of some B cell follicles
Immunoanatomy of resting human lymph nodes

CD20: B cells
CD3: T cells
ACTA2: Vascular smooth muscle cells/FRCs
-
large T cell zone
-
multiple lymph node lobules
-
atypical positioning of some B cell follicles
→ topological remnants of recurrent/baseline activation
Immunoanatomy of resting human lymph nodes
LYVE1: Lymphatic endothelium
CD31: Endothelium
ACTA2: Vascular smooth muscle cells/FRCs

-
Extensive vasculature with a large perivascular space
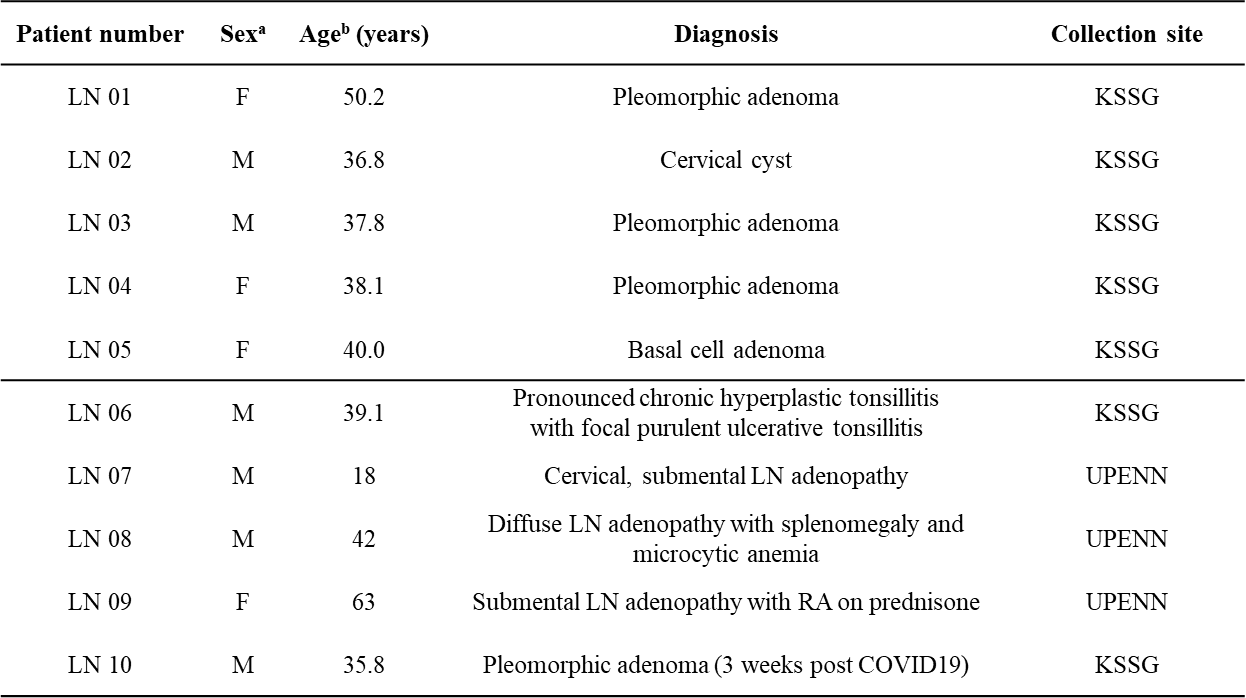
Transcriptome analyses - Patient characteristics


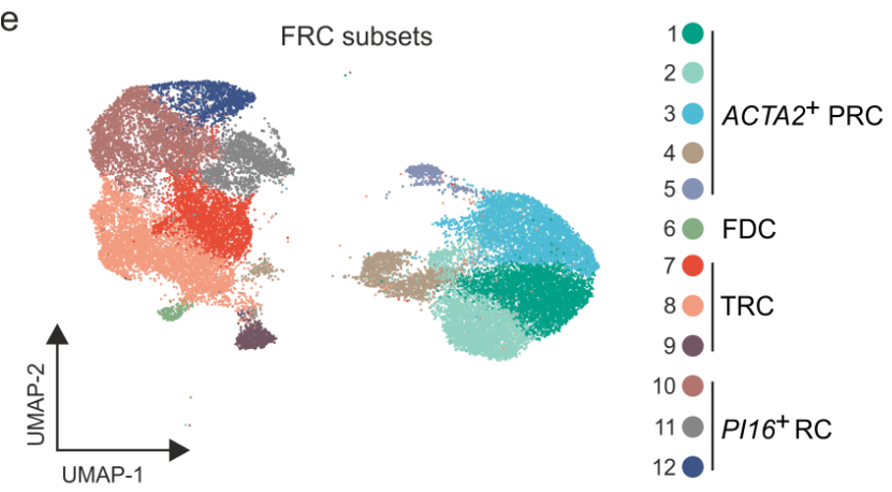
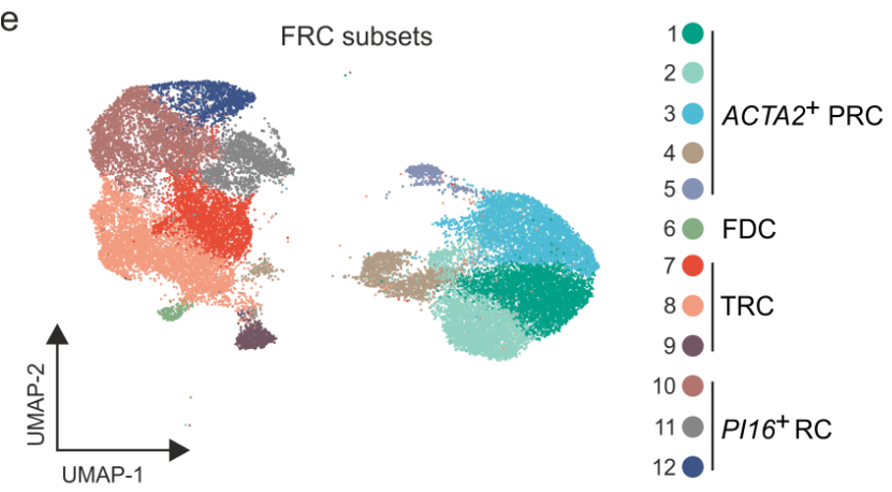
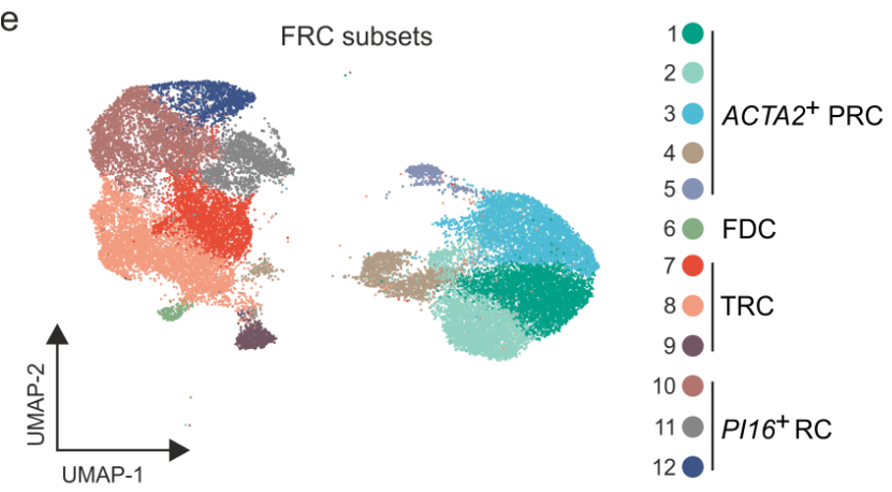
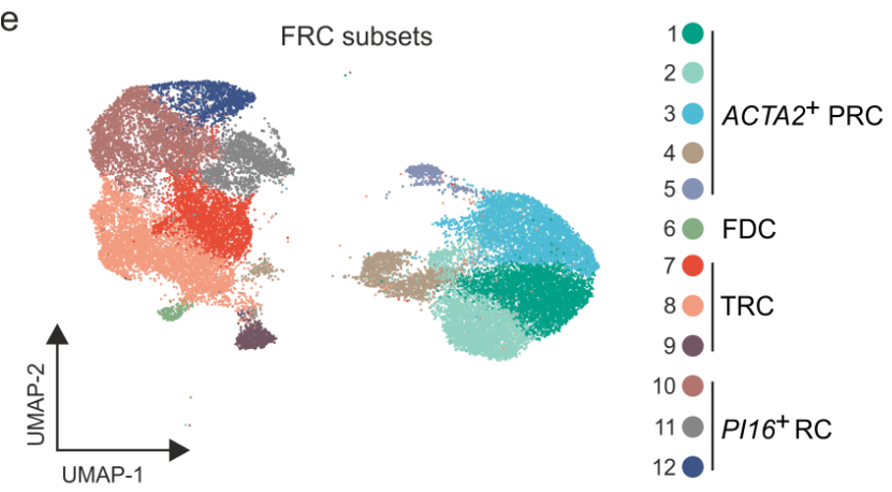
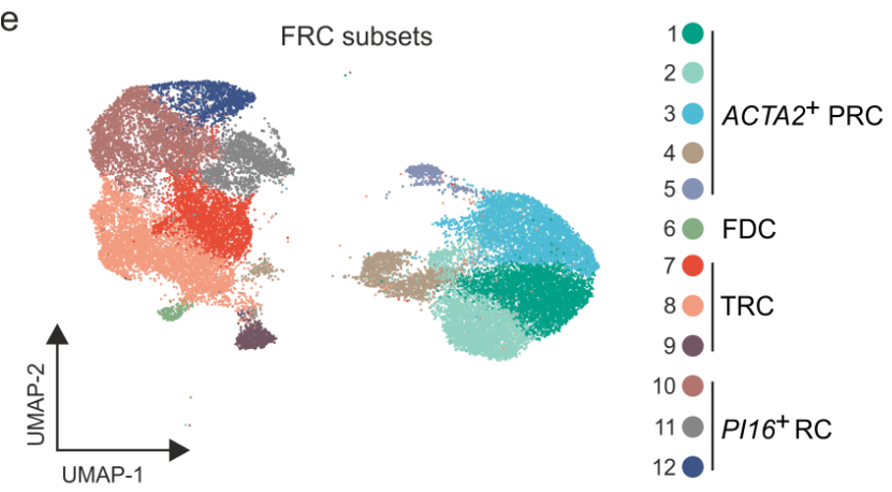
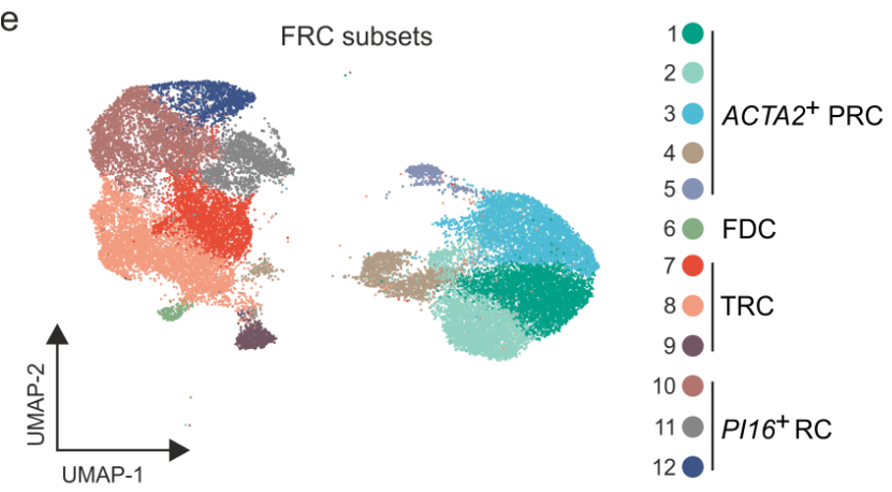
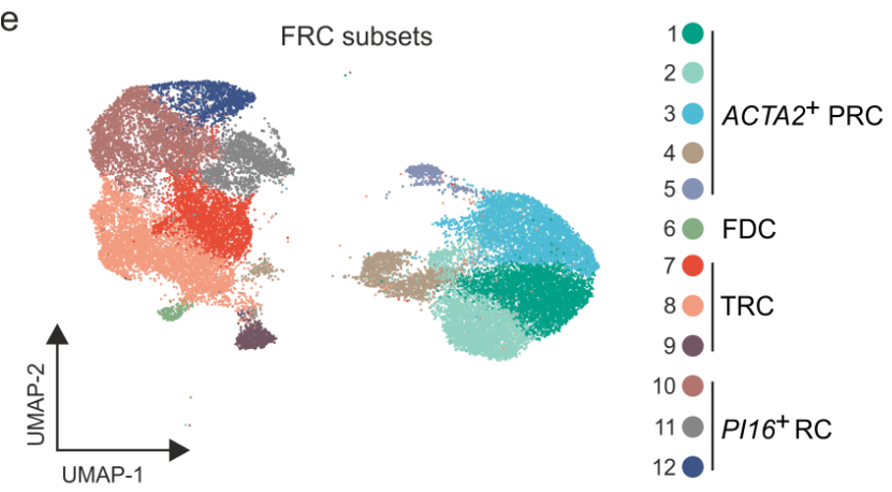
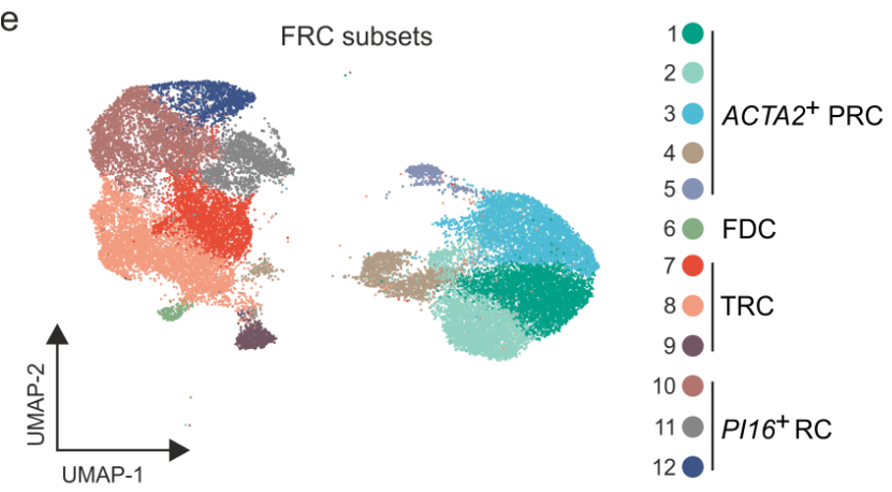
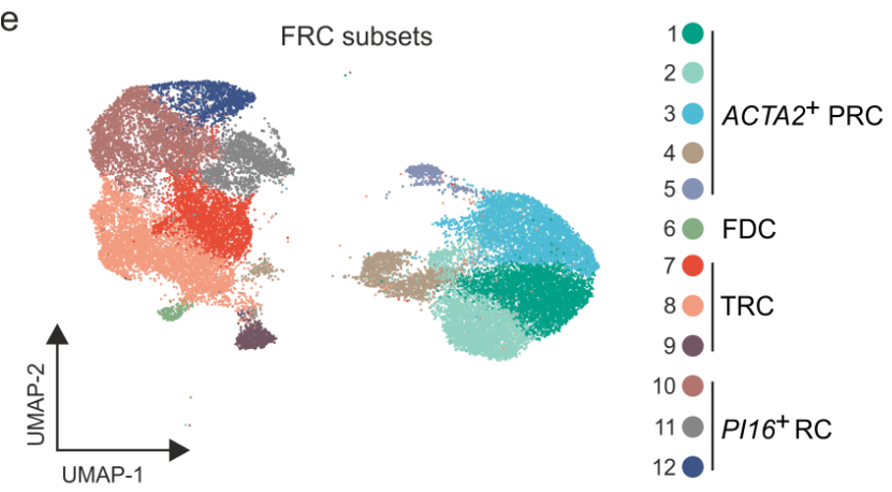
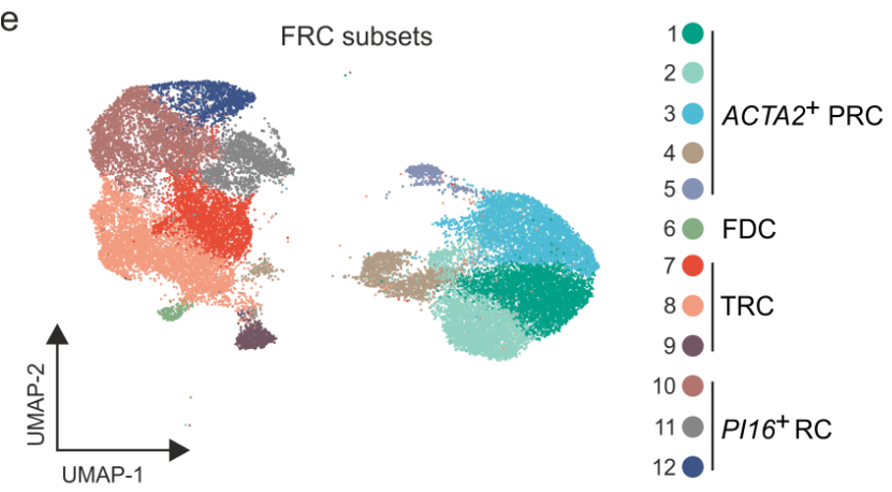
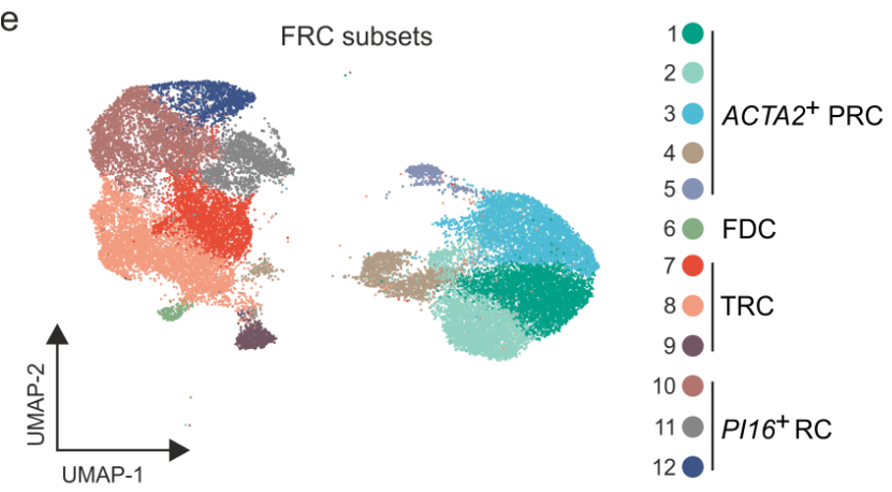
Distinct FRC subsets form the perivascular niche in human lymph nodes

Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils

Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils
-
Distinct perivascular FRC subsets

Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils
-
PI16+RCs, PRCs and VSMCs share the expression of genes involved in vascular support


Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils
-
Distinct perivascular FRC subsets


Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils
-
Distinct perivascular FRC subsets and VSMCs share the expression of genes involved in vascular support

Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils
-
Distinct perivascular FRC subsets and VSMCs share the expression of genes involved in vascular support

Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils
-
Distinct perivascular FRC subsets and VSMCs share the expression of genes involved in vascular support
→ Localization?
Distinct FRC subsets form the perivascular niche in human lymph nodes


Distinct FRC subsets form the perivascular niche in human lymph nodes


Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils


Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils
-
PI16+RCs, PRCs and VSMCs share the expression of genes involved in vascular support



Distinct FRC subsets form the perivascular niche in human lymph nodes
-
Strong overlap with FRC landscape in human tonsils
-
PI16+RCs, PRCs and VSMCs share the expression of genes involved in vascular support → Localization?


Distinct FRC subsets form the perivascular niche in human lymph nodes

Distinct FRC subsets form the perivascular niche in human lymph nodes

Distinct FRC subsets form the perivascular niche in human lymph nodes

Distinct FRC subsets form the perivascular niche in human lymph nodes

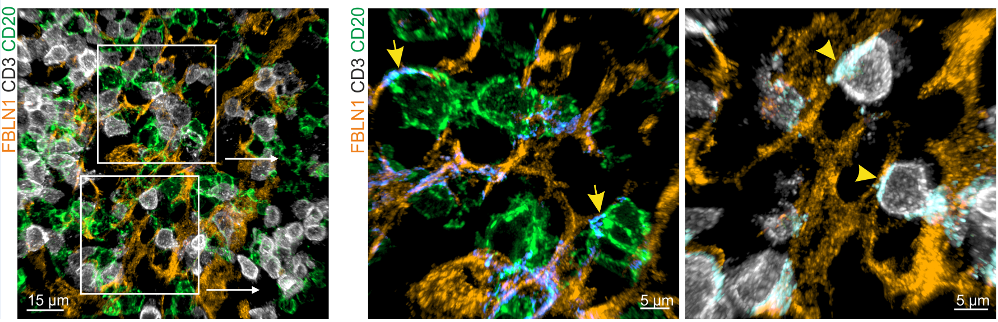
- PI16+RCs: subcapsular sinus and medulla
-
ACTA2+PRC: medulla and T cell zone
-
ADGRF5+PRC: subcapsular region
Distinct FRC subsets form the perivascular niche in human lymph nodes

- PI16+RCs: subcapsular sinus and medulla
-
ACTA2+PRC: medulla and T cell zone
-
ADGRF5+PRC: subcapsular region
→ Structured organization along the lymphatic and blood vasculature
A vascular zonation imprints FRC subset identities






A vascular zonation imprints FRC subset identities



A vascular zonation imprints FRC subset identities



A vascular zonation imprints FRC subset identities



A vascular zonation imprints FRC subset identities

A vascular zonation imprints FRC subset identities
Spatial transcriptomics to predict the localization of PI16+RCs

Spatial transcriptomics to predict the localization of PI16+RCs


Spatial transcriptomics to predict the localization of PI16+RCs


Spatial transcriptomics to predict the localization of PI16+RCs


Spatial transcriptomics to predict the localization of PI16+RCs

- PI16+RCs: subcapsular sinus and medulla

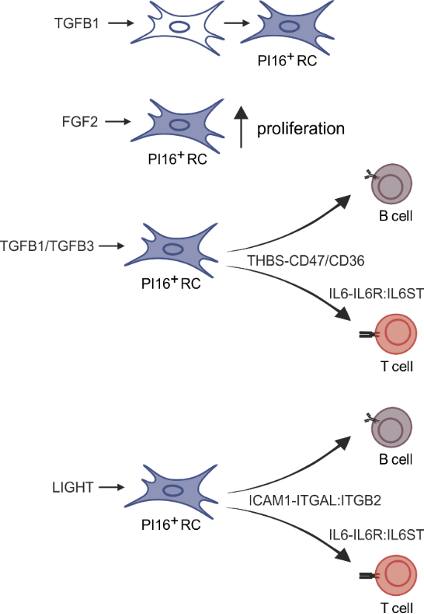
PI16+RCs support the subcapsular sinus and large arteries in the medulla

PI16+RCs support the subcapsular sinus and large arteries in the medulla


PI16+RCs support the subcapsular sinus and large arteries in the medulla


PI16+RCs support the subcapsular sinus and large arteries in the medulla








PI16+RCs support the subcapsular sinus and large arteries in the medulla
Transcriptome analyses - Patient characteristics

PI16+ RCs support inflammation-induced remodeling in human lymph nodes

PI16+ RCs support inflammation-induced remodeling in human lymph nodes


PI16+ RCs support inflammation-induced remodeling in human lymph nodes
- All FRC subset are conserved upon chronic activation


PI16+ RCs support inflammation-induced remodeling in human lymph nodes
- All FRC subset are conserved upon chronic activation


PI16+ RCs support inflammation-induced remodeling in human lymph nodes
- All FRC subset are conserved upon chronic activation
- PI16+RCs support tissue remodelling in inflamed human lymph nodes → immune cell interactions?


PI16+ RCs support inflammation-induced remodeling in human lymph nodes
- All FRC subset are conserved upon chronic activation
- PI16+RCs support tissue remodelling in inflamed human lymph nodes → immune cell interactions?



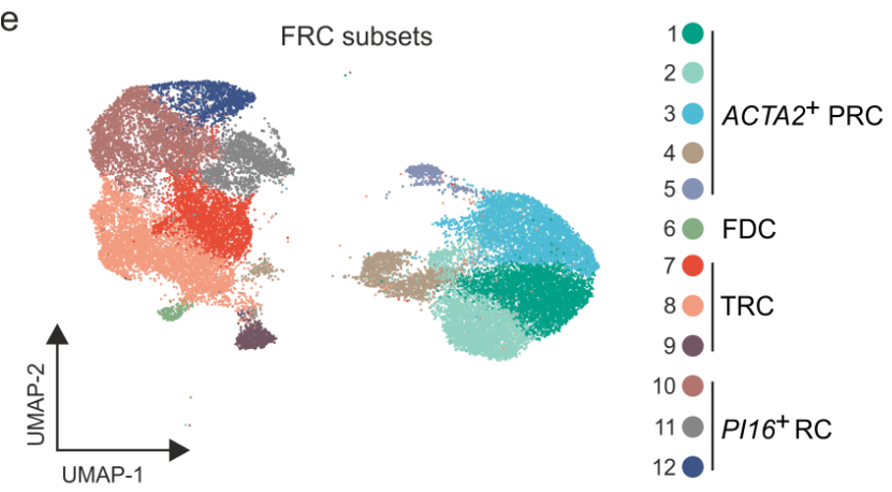
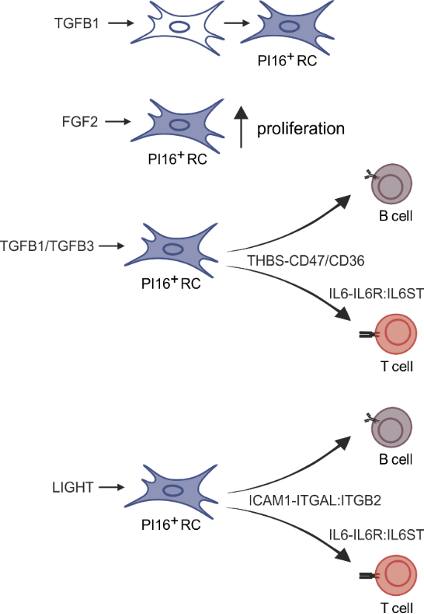
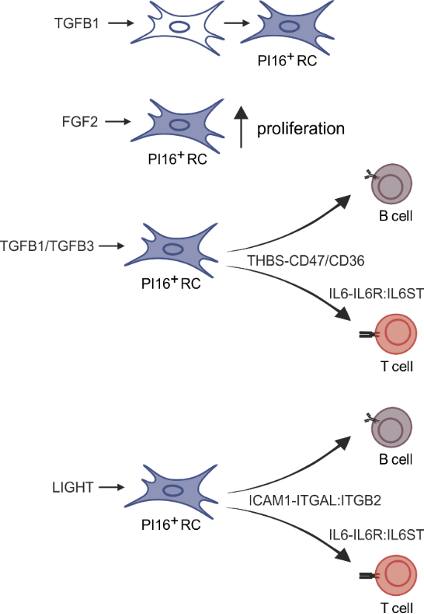
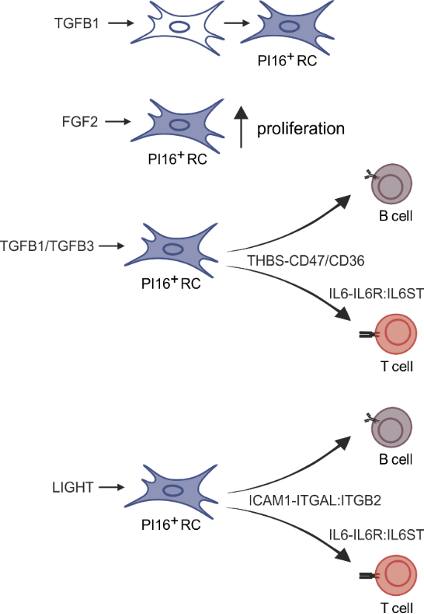
PI16+ RCs form reactive immune cell niches
- Bidirectional crosstalk between PI16+RCs and immune cells

- Bidirectional crosstalk between PI16+RCs and immune cells



Immune cell-provided activation cues
PI16+ RCs form reactive immune cell niches
- Bidirectional crosstalk between PI16+RCs and immune cells



Immune cell-provided activation cues
PI16+ RCs form reactive immune cell niches



Immune cell-provided activation cues
PI16+ RCs form reactive immune cell niches
Inferred interactions upon lymph node activation:
- PI16+RCs integrate activation cues from macrophages and dendritic cells



PI16+RC-provided immune-modulation cues

PI16+ RCs form reactive immune cell niches



PI16+RC-provided immune-modulation cues

PI16+ RCs form reactive immune cell niches



PI16+RC-provided immune-modulation cues

PI16+ RCs form reactive immune cell niches
Inferred interactions upon lymph node activation:
- PI16+RCs integrate activation cues from macrophages and dendritic cells
- PI16+RCs provide immune modulatory cues to macrophages and dendritic cells



PI16+RC-provided immune-modulation cues

→ Validation?
PI16+ RCs form reactive immune cell niches
Inferred interactions upon lymph node activation:
- PI16+RCs integrate activation cues from macrophages and dendritic cells
- PI16+RCs provide immune modulatory cues to macrophages and dendritic cells
Summary II: PI16+ reticular cells form reactive immune cell niches in human lymph nodes
Stereotypic «resting» human lymph node:
Summary II: PI16+ reticular cells form reactive immune cell niches in human lymph nodes
Stereotypic «resting» human lymph node:
- Baseline activation in single lobules and atypical positioning of B cell follicles likely reflecting topological remnants of recurrent activation
Summary II: PI16+ reticular cells form reactive immune cell niches in human lymph nodes
Stereotypic «resting» human lymph node:
- Baseline activation in single lobules and atypical positioning of B cell follicles likely reflecting topological remnants of recurrent activation
- Extensive vasculature with a large perivascular space formed by distinct FRC subsets including PI16+RCs
Summary II: PI16+ reticular cells form reactive immune cell niches in human lymph nodes
Stereotypic «resting» human lymph node:
- Baseline activation in single lobules and atypical positioning of B cell follicles likely reflecting topological remnants of recurrent activation
- Extensive vasculature with a large perivascular space formed by distinct FRC subsets including PI16+RCs
Inflammatory activation of human lymph nodes:

Summary II: PI16+ reticular cells form reactive immune cell niches in human lymph nodes
Stereotypic «resting» human lymph node:
- Baseline activation in single lobules and atypical positioning of B cell follicles likely reflecting topological remnants of recurrent activation
- Extensive vasculature with a large perivascular space formed by distinct FRC subsets including PI16+RCs
Inflammatory activation of human lymph nodes:
- PI16+ RCs support inflammation-induced tissue remodeling

Summary II: PI16+ reticular cells form reactive immune cell niches in human lymph nodes
Stereotypic «resting» human lymph node:
- Baseline activation in single lobules and atypical positioning of B cell follicles likely reflecting topological remnants of recurrent activation
- Extensive vasculature with a large perivascular space formed by distinct FRC subsets including PI16+RCs
Inflammatory activation of human lymph nodes:
- PI16+ RCs support inflammation-induced tissue remodeling
- Perivenous PI16+RCs engage with macrophages and dendritic cells and form reactive immune cell niches (validation ongoing)

Burkhard Ludewig Group
Angelina De Martin
Lisa Kurz
Samuel Meili
Nadine Cadosch
Christian Perez-Shibayama
Cristina Gil-Cruz
Hung-Wei Cheng
Lucas Onder
Natalia Pikor Group
Sarah Grabherr
Acknowledgements

Department of
Otorhinolarnygology (KSSG)
Sandro Stöckli
Yves Stanossek
Samuel Meili
PhD Committee
Burkhard Ludewig
Mark D. Robinson
Maries van den Broek
University of Zurich
Charlotte Soneson
Almut Lütge
University of Pennsylvania
Joshua Brandstadter
Ivan Maillard


