Oshtoran Syndrome
What do we know?
Facts:
- A heritable condition
- Autosomal dominant with incomplete penetrance
- Abnormal inert immune hyperactivity
- Multi organ dysfunction (brain, nervous system, liver, adrenal gland, etc.)
Symptom Clusters
- Immune system (hyperactivity of the inert segment)
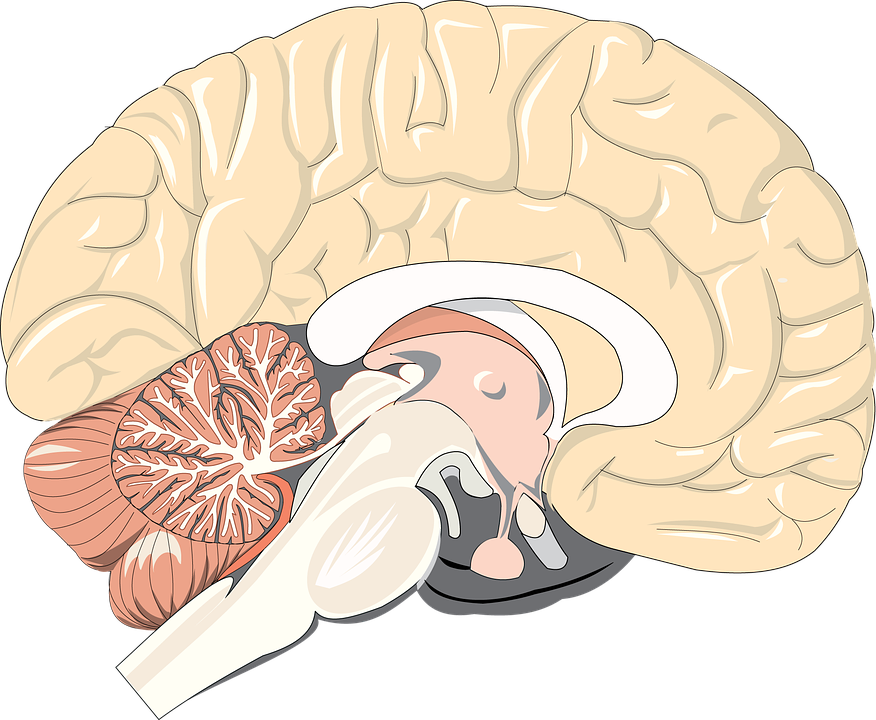
- Nervous system and brain (presumed cause: dysfunction of the kynurenine, glutamine, dopamine, serotonin etc. metabolisms/pathways & adrenal gland hyperfunction)
- Liver: Dysfunction of fat metabolism and hyperplastic nodules
What don't we know?
- The exact pathomechanism
- Triggers?
- The reason for the wide variability of phenotypes
A rare syndrome?
It may be that "Patient 0" and her 100+ descendants are the only affected population. As long as we do not have clear diagnostic standards and testing procedures, this remains a possibility.
A fairly common syndrom?
It may be a rather common syndrome which has been overlooked due to its multi organ affection and psychiatric symptom clusters. In this case we have to screen for misdiagnosed patients.
Where to look for possible Oshtoran patients?
- Psychiatric clinics (refractory and/or atypical cases of thought and mood disorders)
- Neurological clinics (atypical and/or movement disorders)
- Liver Clinics (hyperplastic nodules, fatty infiltrations, etc.)
- Family doctors/GPs (atypical symptom constellations liver-brain-behaviour-neurological-abnormally strong immune reactions)
What to screen for?
- A combination of psychiatric and/or neurological symptoms, fatty liver and/or hyperplastic nodules in the liver, signs (blood tests or clinical symptoms) of hyperactive type 1 immune reactions.
- Family clusters of such symptoms
Next steps:
- Ensure appropriate funding
- Establish contact with specialized clinicians
- Establish interdisciplinary cooperation