Rheumatoid Lung Disease
Jason Hostetter
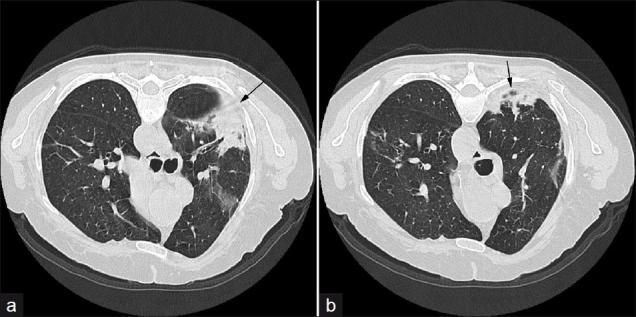
Patient 1 - 48 year old woman
Patient 1 - 48 year old woman
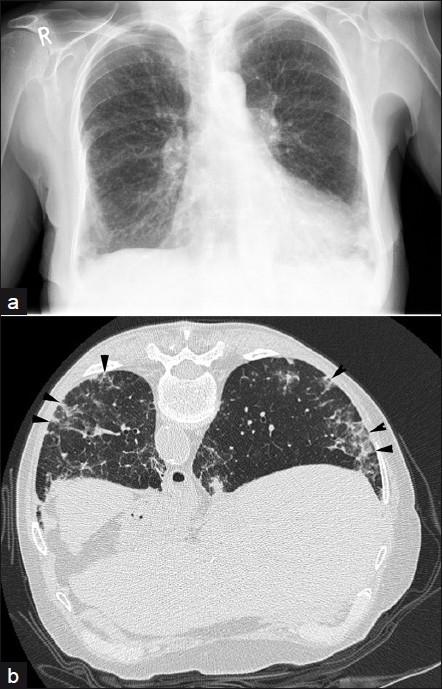
Patient 2 - 67 year old man
Patient 2 - 67 year old man
Patient 2 - 67 year old man
Epidemiology
- RA 1% prevalence
- more common in women (3:1)
- pleuropulmonary manifestations 40-75%
- more common in men (5:1)
- 2nd most common cause of death (18%) after infection
Pleural Disease
- pleural thickening or effusion most common thoracic manifestation
- effusions in 3-5% of pts, usually during flares, tend to resolve spontaneously
- 80% male, 80% had rheumatoid nodules
- almost all > 35 yrs old
Pneumothorax
- Uncommon
- possibly due to caviation of subpleural necrobiotic nodule
- may develop spontaneous sterile empyema, bronchopleural fistula (rare)
Large Airways
- Cricoarytenoid arthritis
- Bronchiectasis

Rheumatoid nodules
- increased incidence:
- men
- smokers
- high RF2 titers
Nodules
- well circumscribed
- in lung, pleura, or pericardium
- freq subpleural, usually multiple
- cavitation in 50%, rarely calcified
- identified in < 1% of chest x-rays
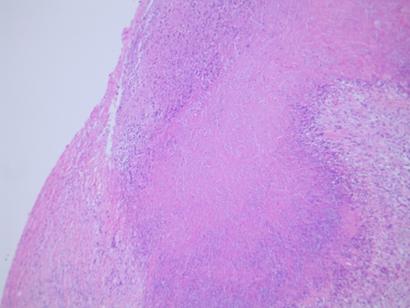
- histology:
- central zone of fibrinoid necrosis surrounded by palisading histiocytes
Rhematoid lung nodule
Nodules
- Usually benign
- Nonspecific, improvement during steroid treatment or regression with time may aid diagnosis
- may be active on PET
Caplan's syndrome
- assoc of rheumatoid nodules with pneumoconioses
- peripheral nodules appear with crops of subcutaneous nodules during RA flare
- biopsy shows inorganic dust within necrotic nodule
- no treatment necessary
Airway and interstitial disease
- strong assoc between RA and obstructive airway dz
- Most common radiographic finding:
- basal linear markings and focal infiltrate
- CT findings:
- bronchiectasis and bronchiolectasis in 30%
- tree-in-bud
Obliterative bronchiolitis
- rare
- women with well-established RA
-
dry cough and rapidly progressive dyspnea
- poor prognosis
- CXR may be normal
- HRCT shows geometric mosaic attenuation
- expiratory scans confirm air trapping
Obliterative bronchiolitis
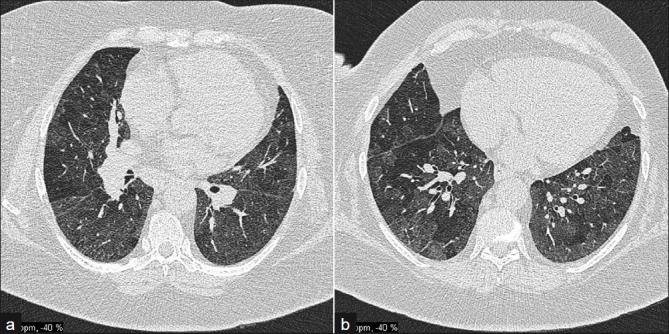
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3177462/
Interstitial lung disease
- Associated with three CT patterns:
- UIP
- NSIP
- organizing pneumonia
UIP
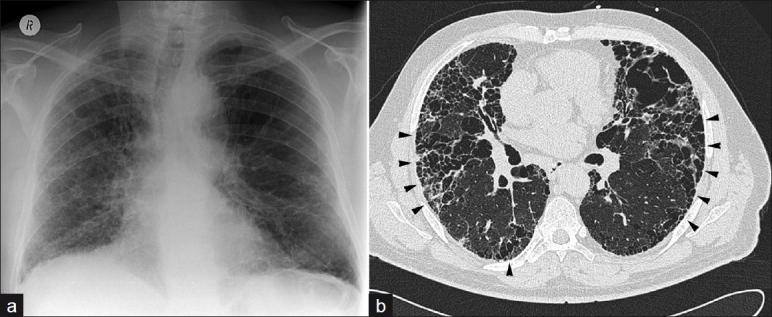
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3177462/
NSIP
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3177462/
Organizing pneumonia
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3177462/
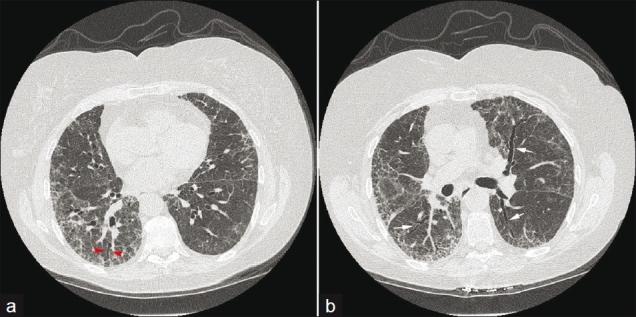
Drug induced lung disease
- Methotrexate induced acute interstitial pneumonitis
- 1-5% of patients
- subacute, progressive cough, dyspnea and fever
- CXR:
- diffuse bilateral, basal interstitial or alveolar infiltrate
- LA or pleural effusions may suggest this diagnosis
- CT:
- NSIP pattern
Methotrexate induced lung disease
References
- Sidhu HS, Bhatnagar G, Bhogal P, Riordan R. Imaging Features of the Pleuropulmonary Manifestations of Rheumatoid Arthritis: Pearls and Pitfalls. J Clin Imaging Sci 2011;1:32 (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3177462/)
- Joseph J. Chena, Barton F. Branstetter IV, Eugene N. Myers. Cricoarytenoid Rheumatoid Arthritis: An Important Consideration in Aggressive Lesions of the Larynx. AJNR 2005 26: 970-972 (http://www.ajnr.org/content/26/4/970.full)
- D.E. Hilling, P.M. van den Berg, A.C. Makkus, F. van der Straaten, P.W. Plaisier: Recurrent Pneumothorax In A Patient With Rheumatoid Arthritis On Leflunomide Treatment: Case Report And Overview Of The Literature. The Internet Journal of Rheumatology. 2007 Volume 3 Number 1. DOI: 10.5580/4c3
Rheumatoid Lung Disease
By Jason Hostetter
Rheumatoid Lung Disease
- 630



