Accessibility to health services in Iceland
Meeting between Nordregio and Byggðastofnun
Ryan Weber & Shinan Wang
Stockholm
1. Presentation of Maps and tables
2. Policy Findings
3. Methodology
The logical start
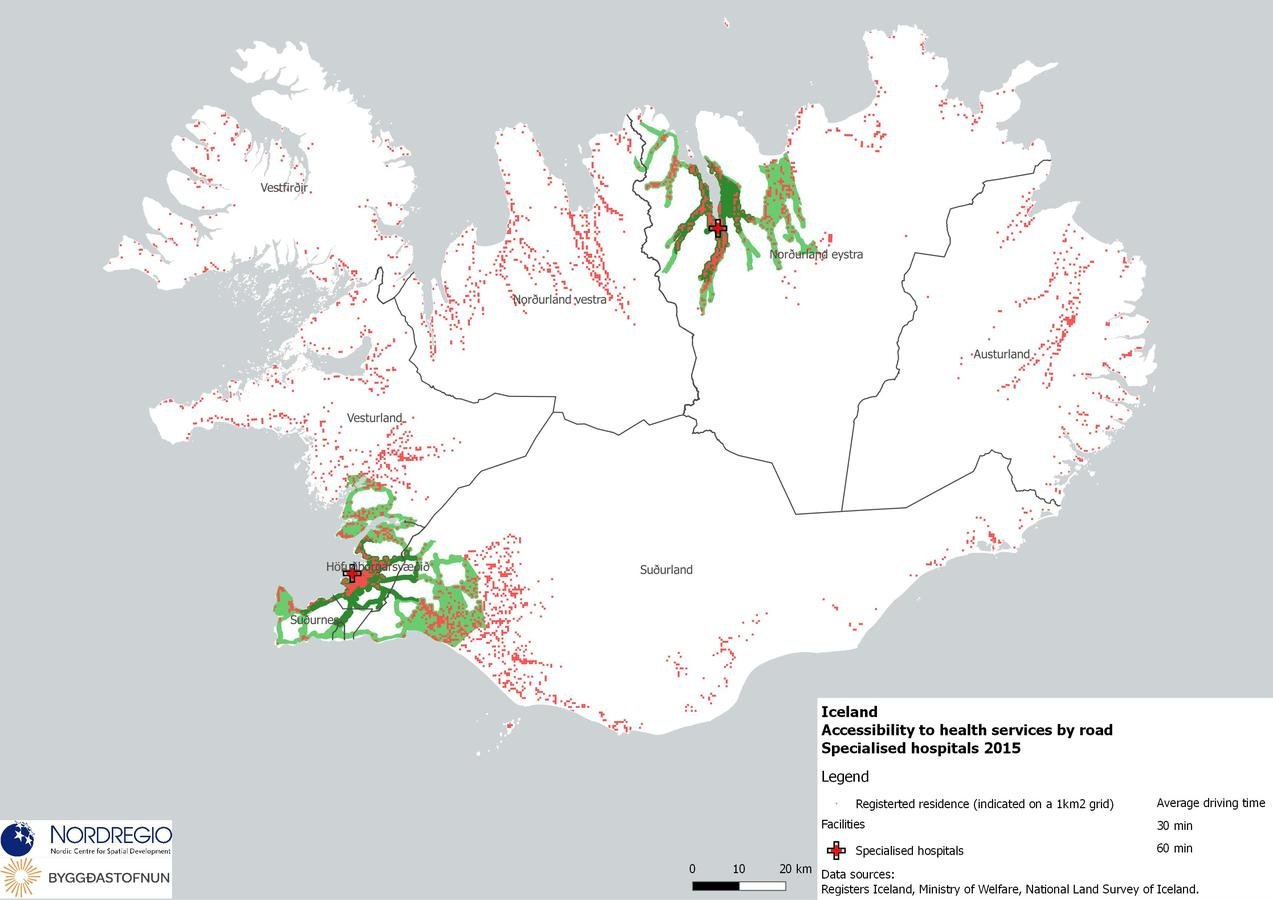
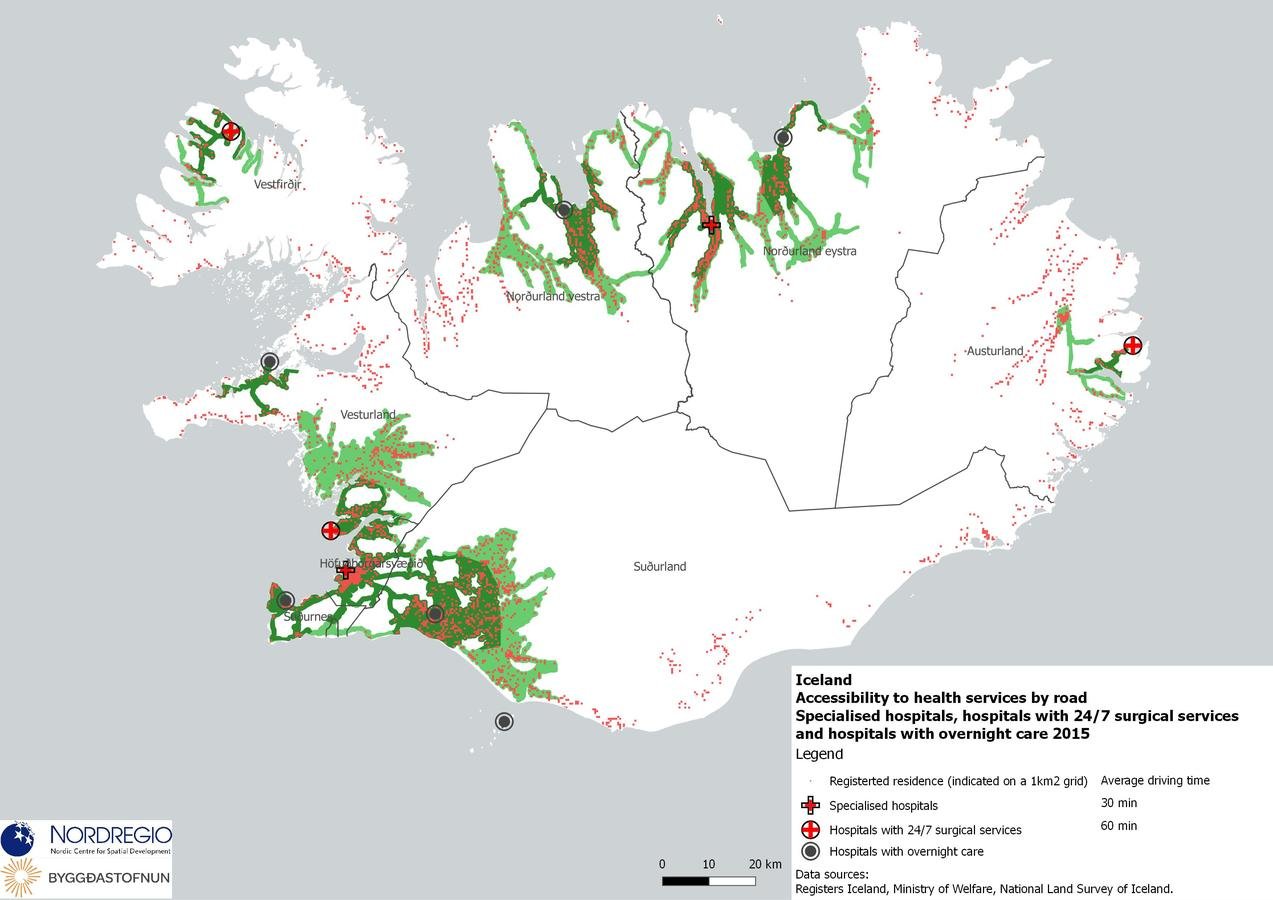
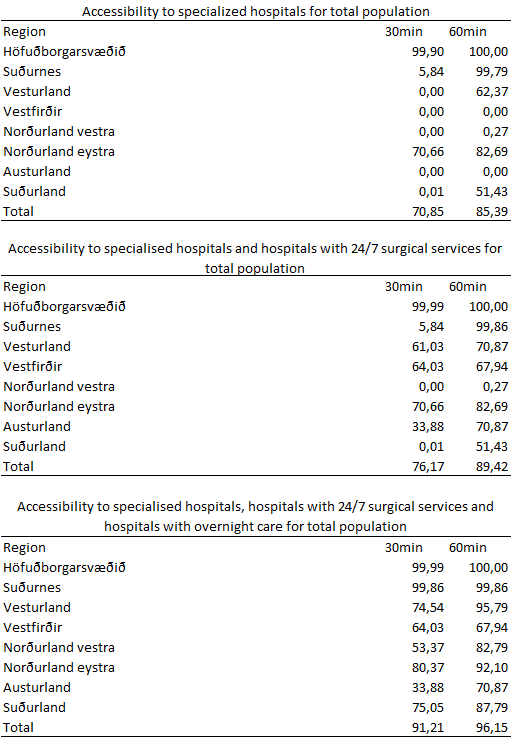
1.Specialised hospitals
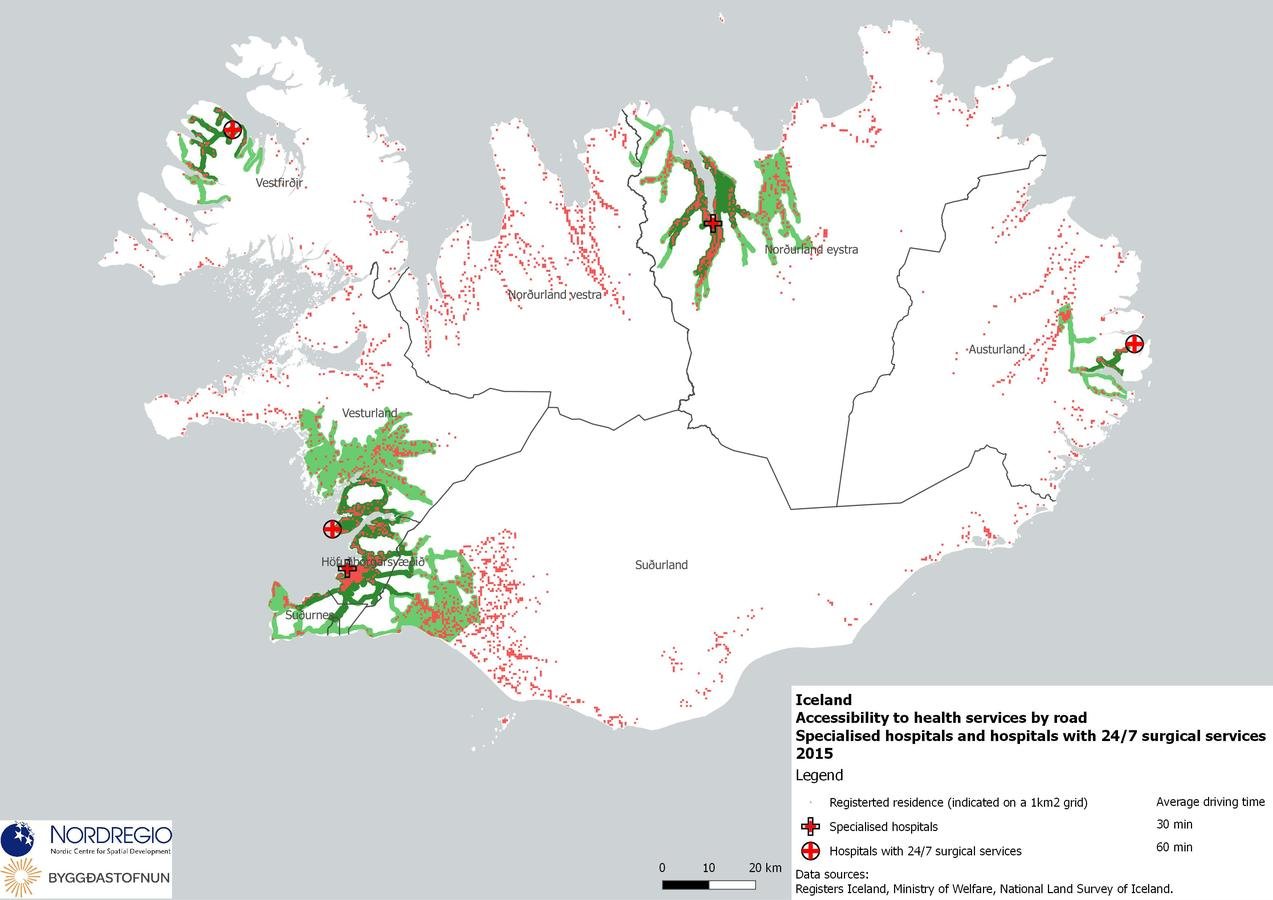
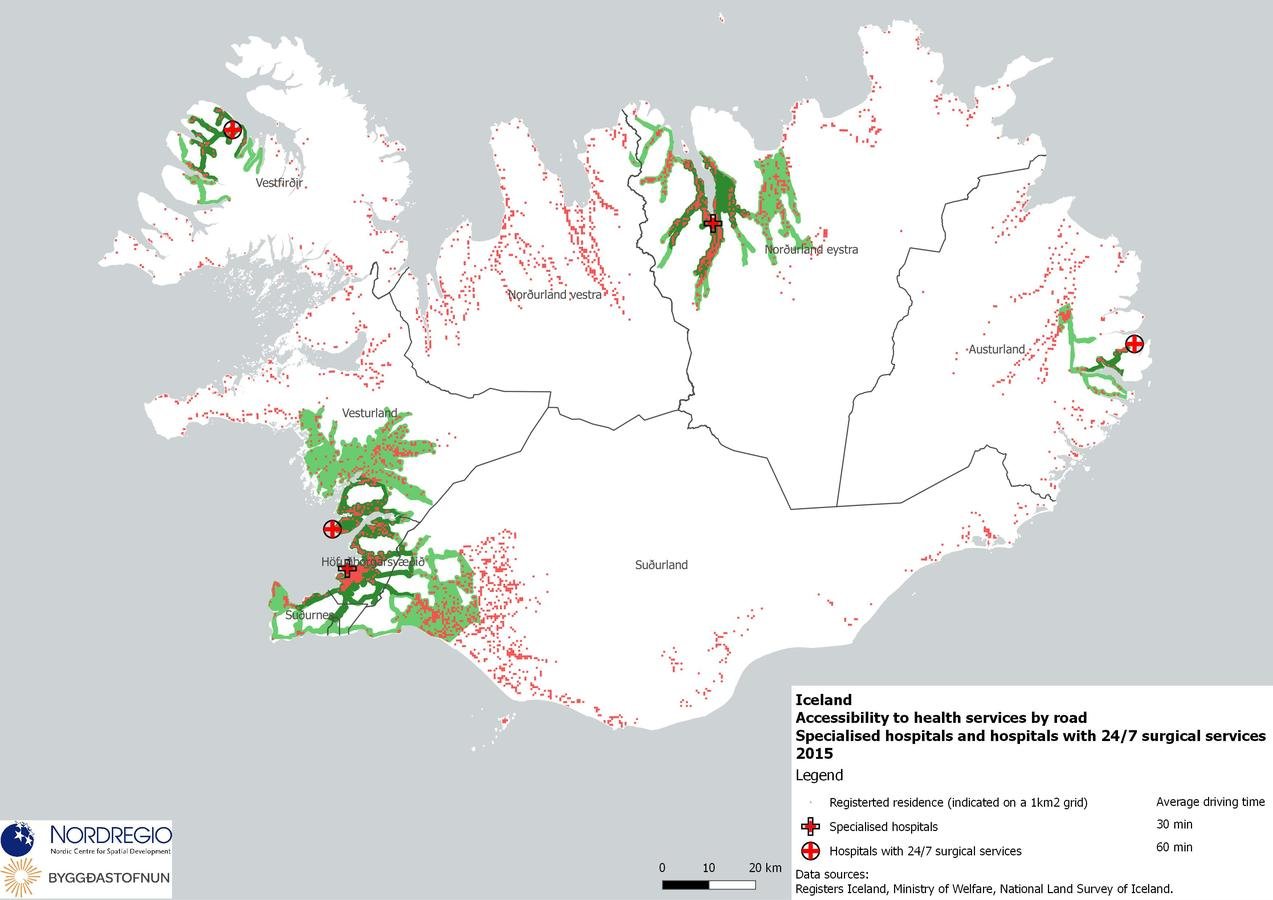
2.Specialised hospitals & Hospitals with 24/7 surgical services
3.Specialised hospitals & Hospitals with 24/7 surgical services & Hospitals with overnight care
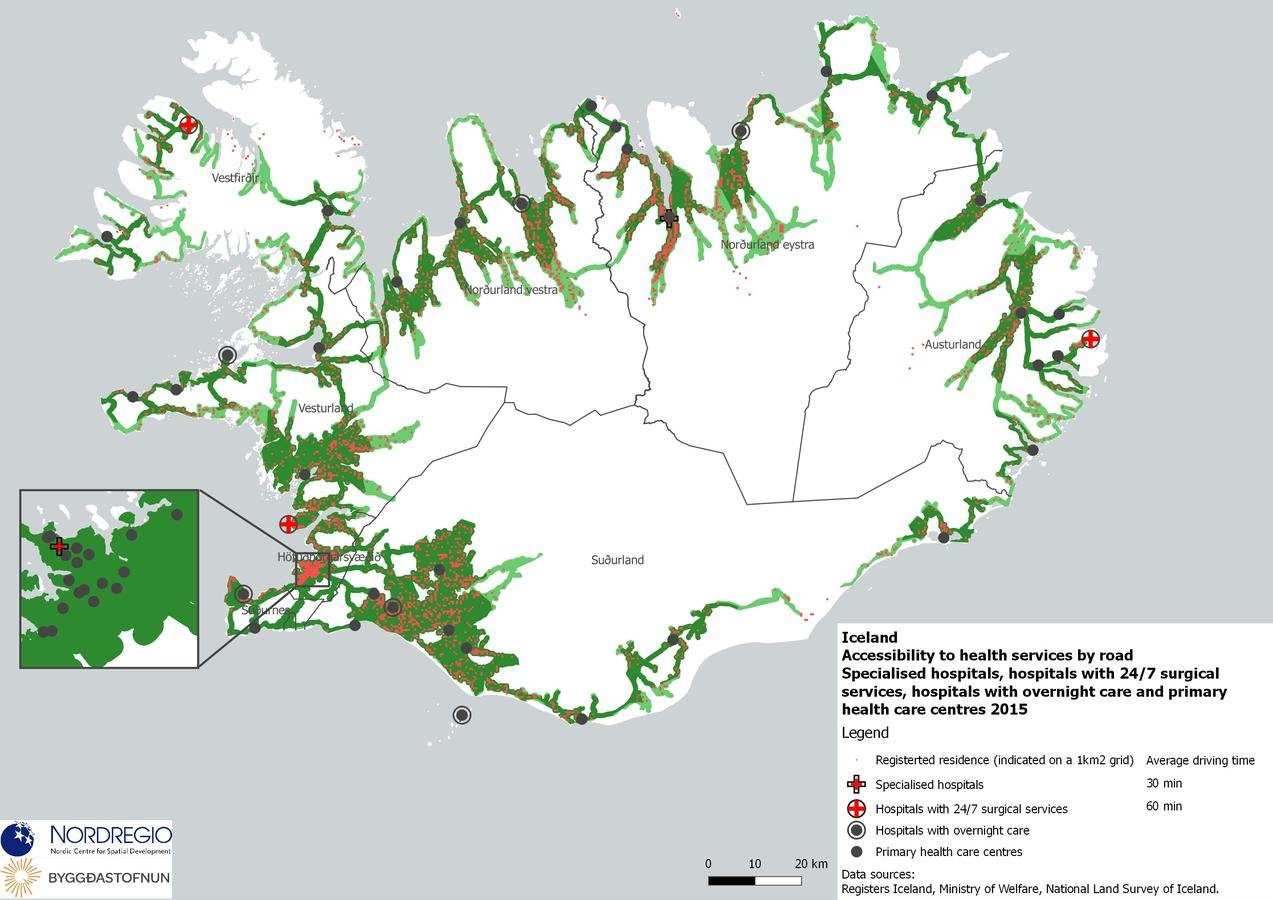
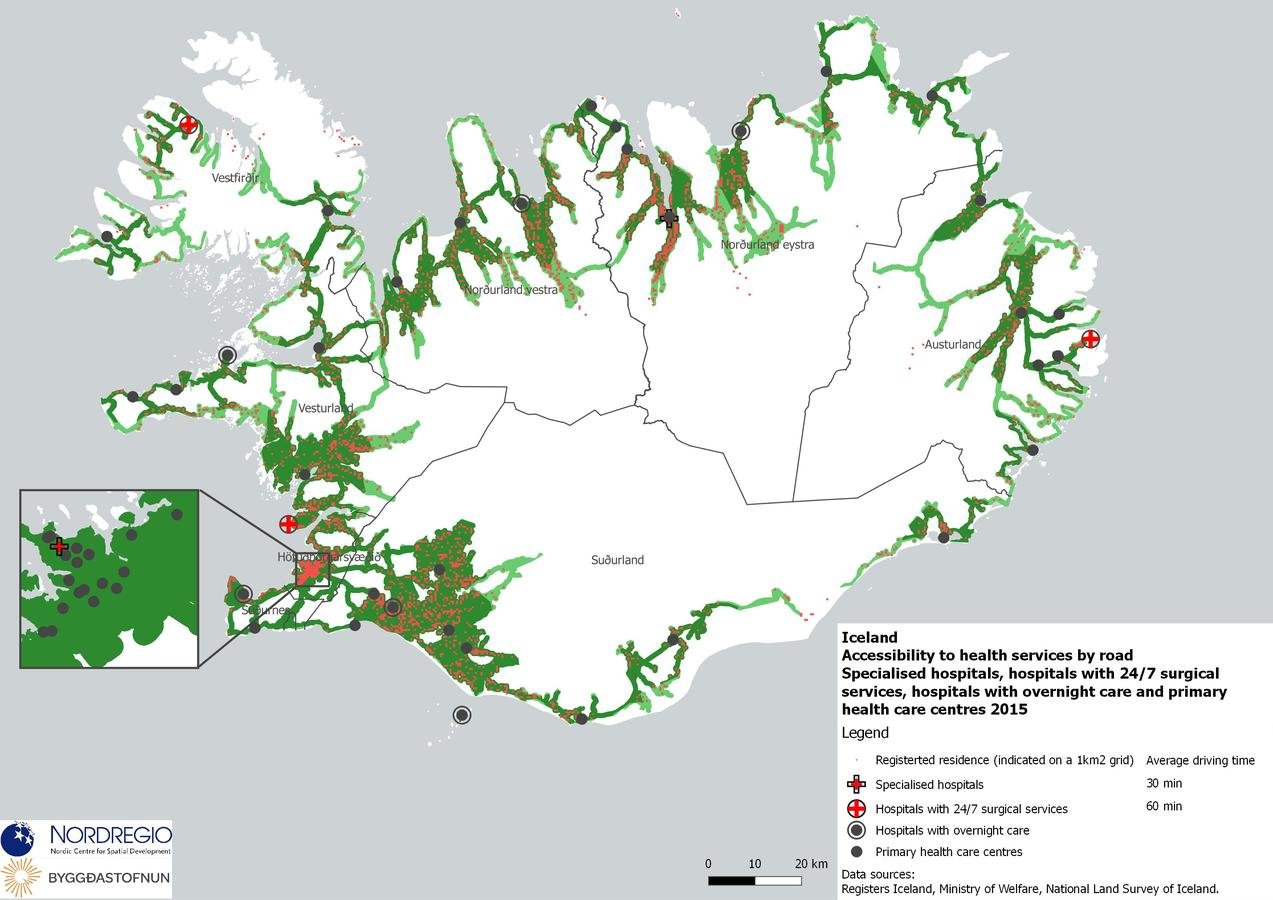
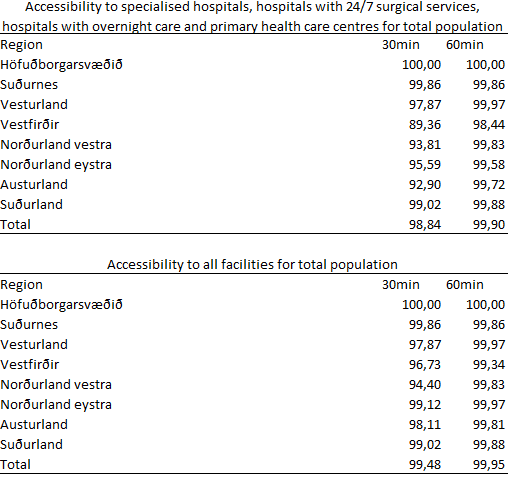
4.Specialised hospitals & Hospitals with 24/7 surgical services & Hospitals with overnight care & Primary health care centres
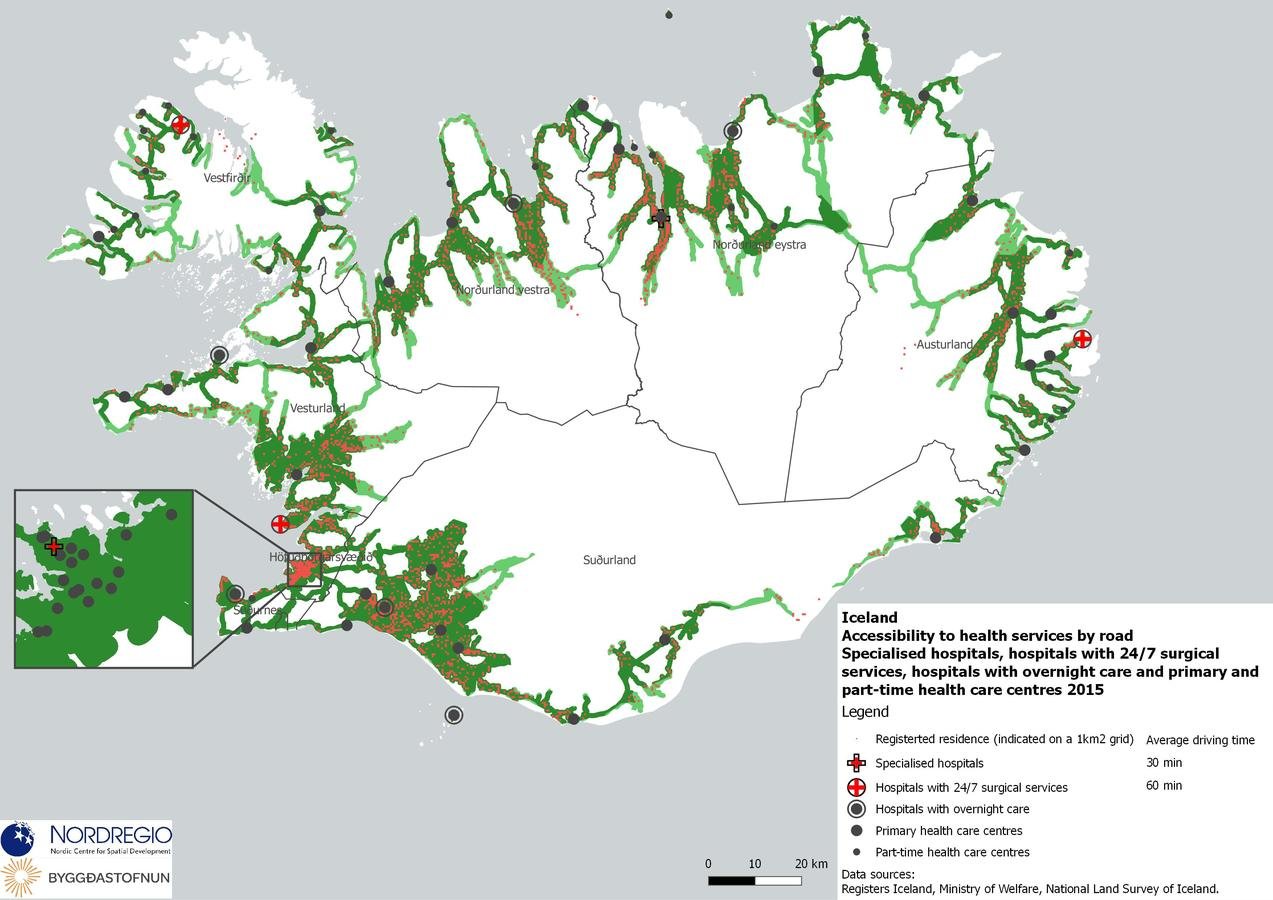
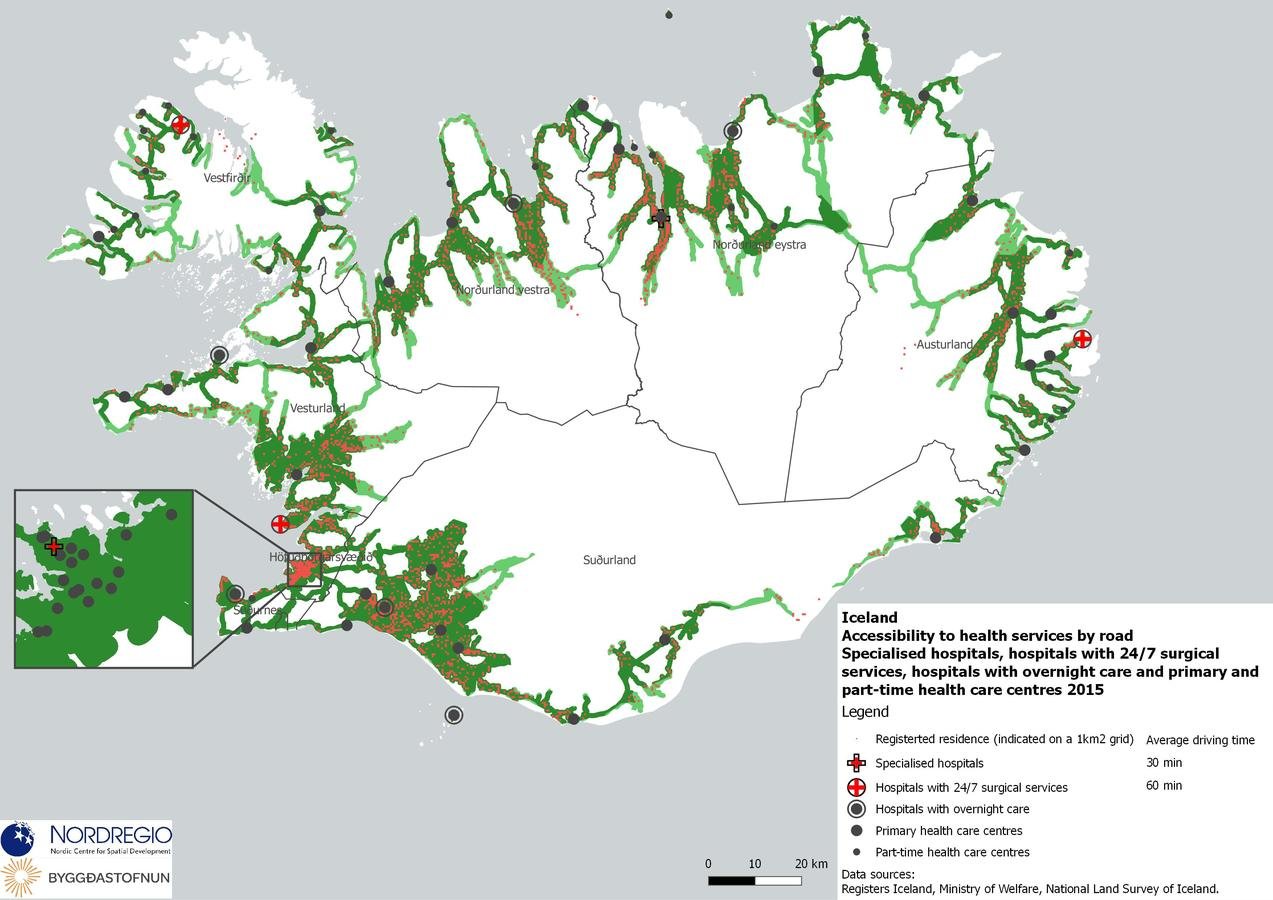
5.Specialised hospitals (2) & Hospitals with 24/7 surgical services (3) & Hospitals with overnight care (6) & Primary health care centres (47) & Part time health care centres (22)
Coverage
Comprehensiveness
Main Policy Findings
1. Spatial patterns and potential solutions to alleviate imbalances
2. Distribution of decision-making for the health sector, including administrative changes and even structural reforms.
Spatial analysis and results
Experiences in other Nordic countries offer a knowledge base for proceeding with potential spatial changes and health care governance reforms in Iceland.
Similar accessibility studies have been conducted, but each one offers different methodological approaches, particularly in terms of differentiation between types of health care locations.
In the future, a Nordic benchmarking of accessibility using a consistent method would appear to be of great benefit.
“all residents should have good access to health care” prevail over concrete policy statements such as “all residents should be located within x minutes driving distance from a doctor or emergency care.”
The issue of rurality and peripheral communities having low access to a range of basic services is perhaps foremost in Iceland compared to Sweden Finland, Denmark and Norway.
But each of these countries are dealing with same types of issues.
Health service provision through internet and telephone, digitization of medical records and air transport are common in the country profiles.
Distinctions between primary and specialized care are required, including potential differences in the level of government responsible for administering such services.
Spatial analysis and results
It is likely not going to be possible to make pronounced changes to the distribution of specialized services, whereby hospitals at the forefront of medical service provision and innovation will centralized in the most populated areas.
Focus must be placed on innovative solutions for responding to medical needs in rural and peripheral locations, especially focussing on elderly care, as well as investment in efficient means of patient transport, particularly in terms of aircraft and helicopter.
Spatial analysis and results
Distribution of decision-making
Finland - debate over the distribution of decision making is on-going.
Health sector privatisation in Sweden
Administrative reform in Denmark.
Generally a two-tier approach, with primary care (often including elderly and long-term care) being handled at the municipal level, with specialized care and hospitals organized at the regional or national level
(with the exception of Finland where the aforementioned reforms are addressing this issue).
Methodology
- Gather locational data for health care sector
- Population density data (2015)
- Road network and speed data
- A fairly simple routing algorithm to determine accessibility to any spatial defined object or grouping/classification of objects.
- Network analysis determining if each populated cell is accessible to a selection of healthcare services.
- Regional assessments consider population density to determine the percentage of populations that are accessible to given services.
Methodology
- Routing algorithm: calculates shortest paths from a given set of points, in this case locations of health care facilities, and finds the paths and nodes of the network that can be reached within the given cost limits.
- So-called alpha shapes were created for these nodes of reachability, in other words minimum enclosing polygons for the furthermost reachable network nodes from each given facility.
- Locations along the road network were selected and enclosed with a service area polygon that could be reached from a given facility within 30 or 60 minutes driving time.
- Unpopulated mountainous areas (> 500 m.a.s.l.), areas far from population (>10 km) and sea areas were removed from the polygons.
Health Services in Iceland
By Ryan Weber
Health Services in Iceland
- 775


