Mrs P
Matt Silsby
Con Yiannikas
The Case
-
49 year old right handed lady
-
Knee pain on climbing stairs 4 years ago
-
GP assessment: concerns re intermittent leg heaviness, referred to Neurologist
Past History
-
No previous medical history
-
No family history
-
Teachers aid
-
Lives with husband and 4 children (20-->15)
-
Non smoker
-
Glass of wine with dinner
The Case
-
Initial review 2014: no focal neurology
-
MRI Brain: a few non-specific subcortical white matter hyperintensities
-
Repeat review shortly thereafter: symptoms had largely resolved
-
There was mild discomfort in her lower limbs and back after a hard day at work
-
Examination remained normal
-
Encouraged to continue exercising and strengthening abdominal and back muscles
The Case
-
Symptoms didn’t seem to leave her alone
-
Ongoing heaviness and weakness in limbs
-
Difficulty walking upstairs due to fatigue
-
Felt “unco” – needed to concentrate on balance at times
-
Symptoms worst in the middle of the day
New Symptoms
- 1 year ago (mid 2015)
- Intermittent diplopia, noted most in bright settings
- Significant fatigue
- Difficulty taking a deep breath
- Blocked ears
- No dysphagia, dysarthria, dysphonia
- Re-reviewed by Neurologist:
Examination
- Mild left upper lid ptosis
- Mild restriction of right eye abduction
- Otherwise normal cranial nerves
- Normal tone and power in limbs. No fatigable weakness
- Reflexes normal, no incoordination
- No sensory loss
- Gait unremarkable
Thoughts??
Investigations
- MRI Brain repeated
- Normal apart from previously noted non-specific white matter hyperintensities
- No brainstem lesions, no periventricular lesions
- CK 161 (NR: <175)
- ACh receptor and MUSK antibodies: negative
- Routine bloods normal
Further Progress
- Noted softening of voice, no slurring, no dysphagia
- Ongoing difficulty with dyspnoea
- Intermittent headaches
- No longer complaining of diplopia
- No vertigo
- No bladder or bowel symptoms
- No rash or arthralgia
- No recent systemic illness
Further Progress
- End of last year (Dec 2015)
- Progression of weakness, felt things were declining quickly
- Summer months, felt her symptoms were worse with hot weather
- Now weak lower > upper limbs, proximal > distal
- Difficulty sit-to-stand, couldn’t ascend a slight incline, stairs without handrails
- Unable to safely drive due to arm weakness
- Impaired balance causing three falls on turning, without significant injury
Examination
- Cranial nerves normal. No ptosis
- 4+/5 shoulder abduction
- 4+/5 elbow flex, 4/5 elbow ext
- 4/5 intrinsic hand muscles/APB
- Hip flexion 3-4/5, hip extension 4/5
- Knee ext 3-4/5, knee flex 4-4+/5
- Ankle DF, PF 5/5
- Reflexes absent
- Cerebellar + sensory normal
Thoughts??
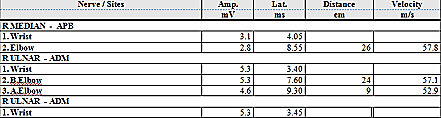
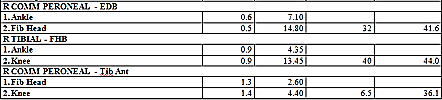
Motor Conduction Studies
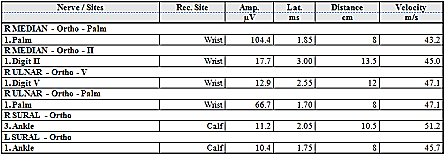
Sensory Conduction Studies
EMG Vastus Lateralis
Investigations
- Vasculitis/Immunological screen negative
- VGKC negative
- Antineuronal antibodies negative
- Antiganglioside antibodies: GM1 IgG and GQ1B IgG antibodies positive
- MRI whole spine: NAD
Reflexes
Ulnar CMAP
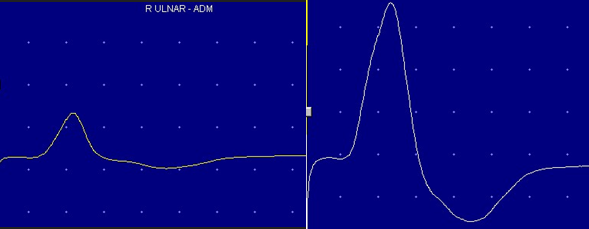
Pre-Exercise
Post-Exercise
Repetitive Stimulation
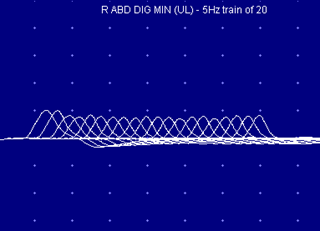

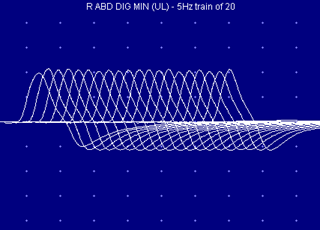
Pre-Exercise
3 min Post-Exercise
30 sec Post-Exercise
Progress
- VGCC antibodies positive – 281pM {< 30}
- 20 kg weight loss over the preceding 2 years
- No change in appetite, no night sweats
- CT CAP – NAD
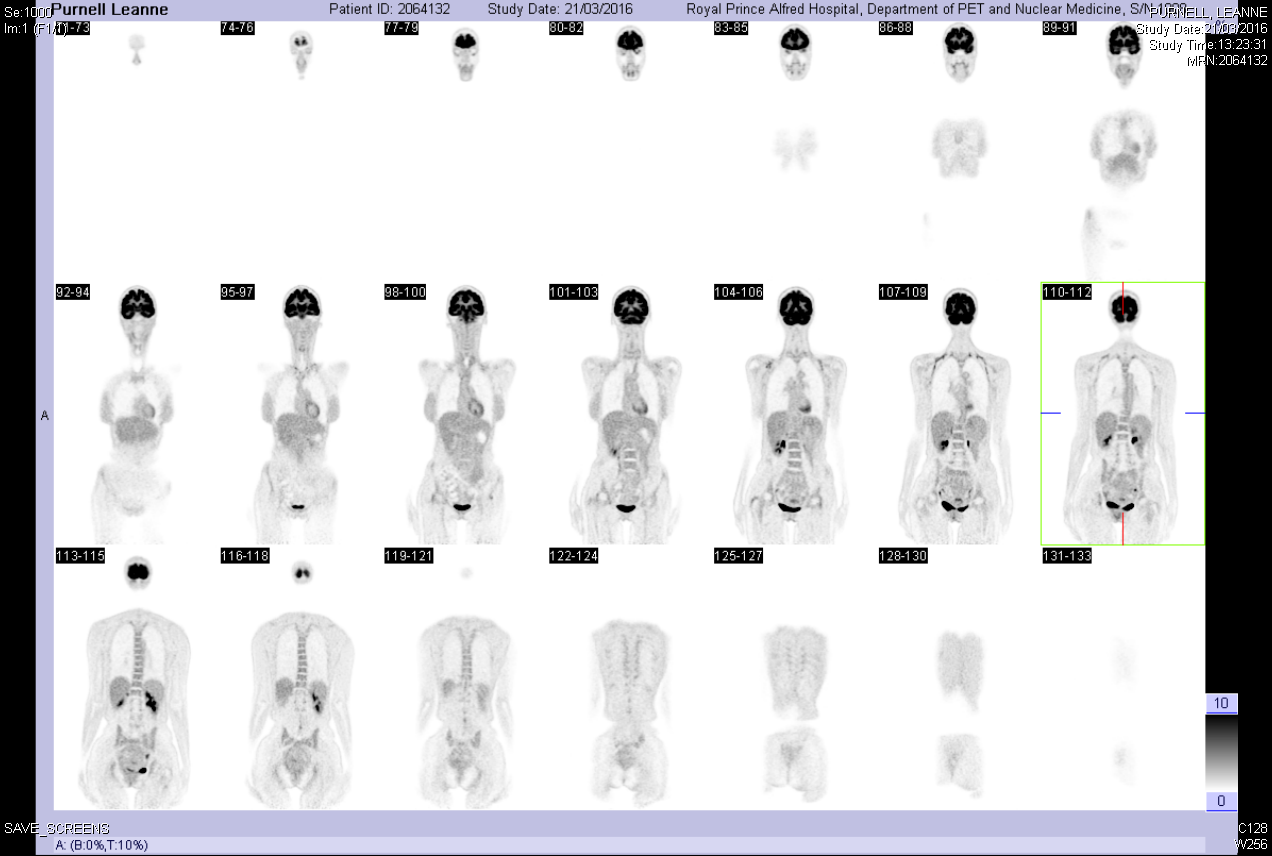
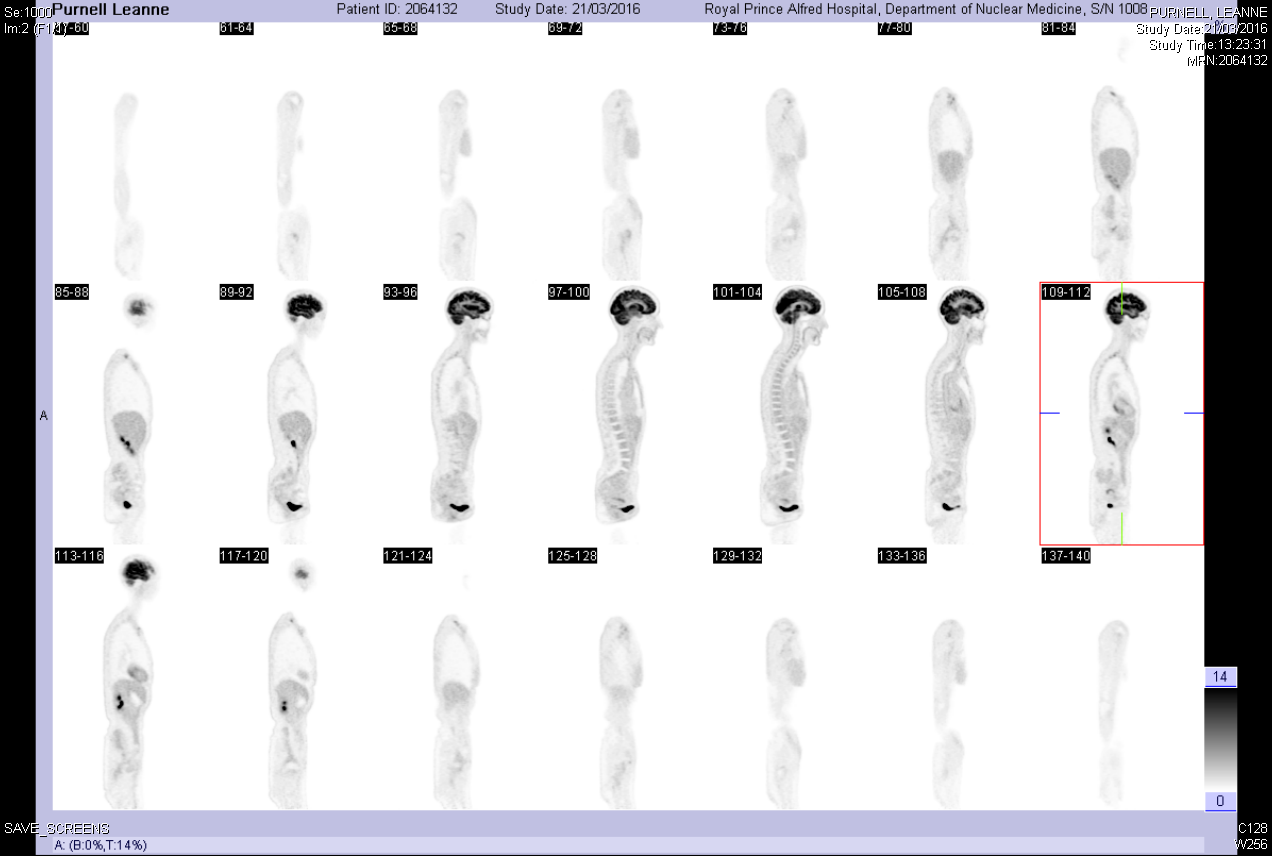
- PET scan:
Management
- Plasmapheresis daily for 3 days
- Weekly since then
- Application with TGA for 3,4-DAP
-
- Making some improvements
LEMS 1
- Rare disorder affecting 3 per 1 million described by Lambert, Eaton and Rooke 1956
- Paraneoplastic in 50-60%
- SCLC most commonly, median age of onset is 60 and majority (65%) are men
-
Non-tumour LEMS of autoimmune aetiology also described, peak incidence at 35 and 60 years old, 52% female
-
Other implicated tumours incl NSCLC, prostate cancer, thymoma, lymphoproliferative
- However few reports only, statistical chance rather than correlation?
1: Titulaer et al, Lancet Neurol 2011; 10: 1098–107
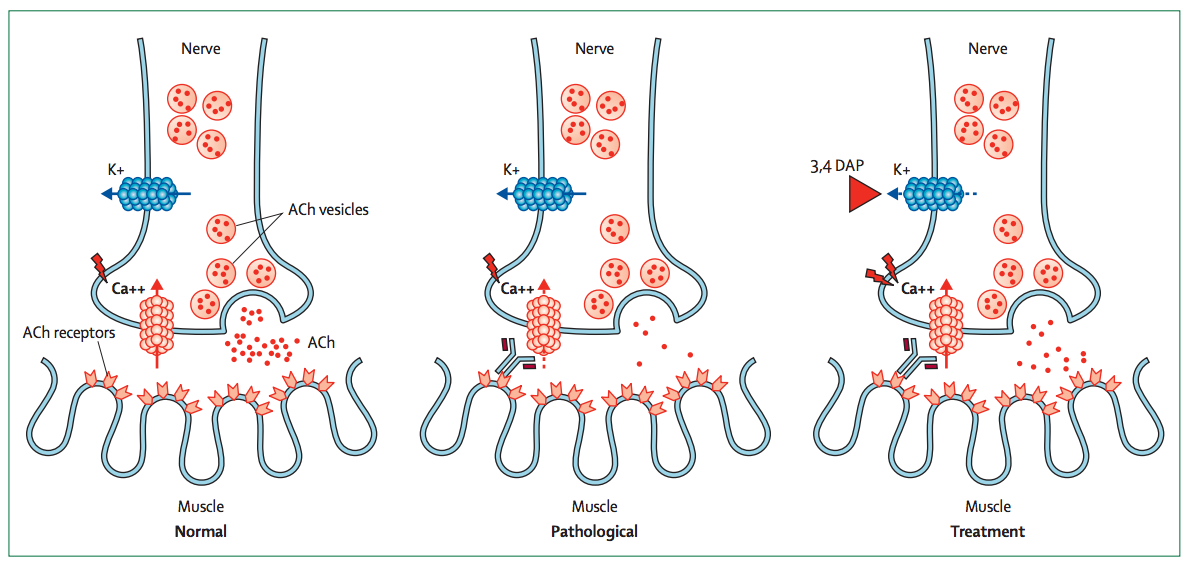
Pathophysiology
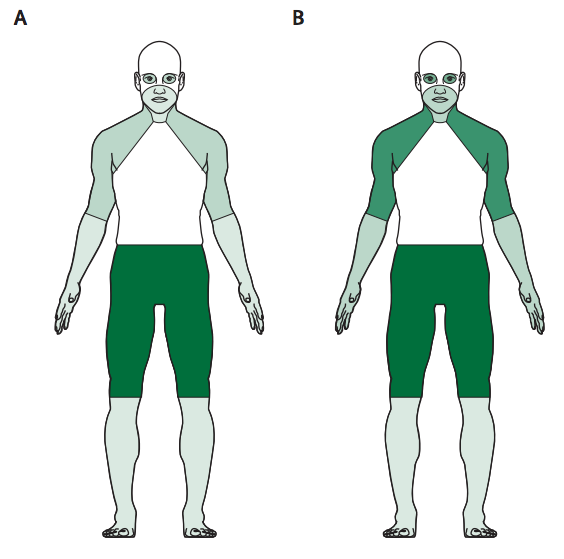
Clinical Features
- Triad typically consisting of proximal muscle weakness, areflexia and autonomic features
- Proximal leg weakness is usually the first symptom noted by the patient (in 80%)
- Weakness of the arms is present on initial assessment or develops quickly
- Weakness normally spreads proximally to distally, involving feet and hands, and caudally to cranially, finally reaching the oculobulbar region
- The speed of progression is much more pronounced in SCLC-LEMS than in NT-LEMS
- Occurrence of ocular symptoms ranges from 0–80%, and bulbar symptoms from 5–80%
- By contrast with MG, isolated ocular symptoms is rare
LEMS
NT-LEMS
SCLC-LEMS
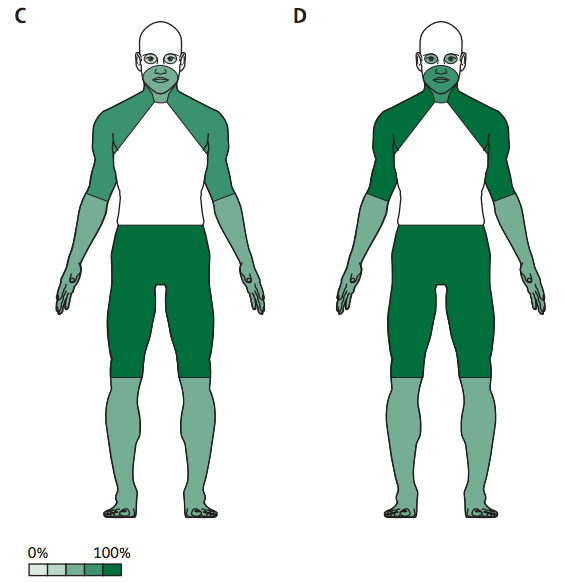
NCS
- Repetitive stimulation is the electrophysiological study of choice
- The first CMAP amplitude is already low, and becomes even lower at low stimulating frequencies (2–5 Hz)
- Decrement can be present at frequencies as low as 0·1 Hz and 94-98% of patients have at least 10% decrement
- To discriminate between LEMS and MG, high frequency stimulation (50 Hz) or, preferably, post-exercise stimulation is done
- An increment in CMAP amplitude higher than 100% is considered abnormal
- Post-exercise stimulation has a sensitivity of 84–96% and specificity 100% for LEMS
Management
- Find the SCLC
- If present, treating the malignancy can improve symptoms
- If this is not present, or symptoms are not improving, add pharmacotherapy:
- 3,4 DAP
- Prednisone + Azathioprine + above
- IVIG or plasmapheresis + above
Prognosis
- 2008 series of 100 patients with biopsy-proven SCLC
- Median survival of LEMS patients was 19.6 months vs. antibody negative patients, 8.9 months
- Median survival of LEMS patients was 19.6 months vs. antibody negative patients, 8.9 months
- 2001 series of 47 patients with NT-LEMS, 45% of patients in remission at 10 years
- Only 14% were not taking Prednisone at final follow up
- 50% taking 3,4-DAP alone
- 25% on AZA and 3,4-DAP
- 25% on no treatment
- Only 14% were not taking Prednisone at final follow up
SCLC Screening
- Screening may not find a tumour
- Sabata, et al (2008) in Barcelona isolated antibodies to SOX1, anti-glial nuclear antibody
- SOX1 present in 64% of SCLC-LEMS vs 0% patients with NT-LEMS (p 0.0001)
- Present in 22% of patients with SCLC without LEMS
Novel therapy
- Tarr, et al, 2014, Philadelphia
- Developed a novel Ca2+ channel agonist, GV-58, that selectively affects P/Q- and N-type, but not L-type, Ca2+ channels as a possible alternative treatment strategy for LEMS
-
3,4-DAP plus GV-58 combination was tested using a mouse passive transfer model of LEMS
- Supra-additive effect that completely reversed the deficit in neurotransmitter release
-
There was less significant improvement observed with either compound alone
- Combination 3,4-DAP and GV-58 a future treatment option for LEMS?
Mrs P
By Integra
Mrs P
- 67


