Outcomes of stereotactic body radiotherapy 60 Gy in 8 fractions when prioritizing organs at risk for central and ultracentral lung tumors
Zhao et al.
Radiation Oncology 2020
Background
- SBRT is standard for early stage inoperable NSCLC
- Central tumors (within 2cm of proximal airways) have higher toxicity risk
- Ultracentral tumors (abutting proximal airways) carry even higher risk
- No consensus on optimal dose/fractionation for central/ultracentral tumors
- Key question: Should we prioritize target coverage or OAR constraints?
Study Design
- Retrospective analysis of provincial protocol
- All central/ultracentral lung tumors treated with SBRT 60 Gy in 8 fractions from 2013-2017
- Practice was to compromise target coverage to meet OAR constraints if needed
- Primary lung tumors and metastases included
- 4D-CT based planning with motion encompassing ITV approach
Patient Selection Criteria
Inclusion Criteria
- Central tumors (either):
- Within 2cm of proximal bronchial tree
- PTV overlapping mediastinal/pericardial pleura
- Ultracentral tumors (PTV overlapping):
- Proximal bronchial tree
- Esophagus
- Pulmonary artery/vein
- Primary lung tumors or metastases
- Treatment from 2013-2017
Exclusion Criteria
- Multiple lesions in single PTV
- Prior treatment to target area
- Non-standard dose/fractionation
- Must be 60 Gy in 8 fractions
Patient Population
- 98 total patients
- 57 central tumors (58.2%)
- 41 ultracentral tumors (41.8%)
- 76 primary lung tumors (77.6%)
- 22 metastases (22.4%)
- Median follow-up: 22.9 months
- Patient characteristics well-balanced between groups
Treatment Planning
- 60 Gy in 8 fractions prescribed to 90% isodose line
- 4D-CT based ITV with 5mm PTV margin
- Planning goals:
- 95% of PTV covered by prescription dose
- 99% of PTV receiving 54 Gy
- OAR constraints prioritized over target coverage
- 3D conformal, IMRT or VMAT planning allowed
| Structure | Constraint | Value |
|---|---|---|
| Spinal cord | Dmax | < 30.6 Gy |
| Proximal bronchial tree | D0.035 cc | < 46.3 Gy |
| Proximal trachea | D0.035 cc | < 46.3 Gy |
| Esophagus | D0.035 cc | < 40 Gy |
| Great vessels | D0.035 cc | < 65 Gy |
| Brachial plexus | D0.035 cc | < 35 Gy |
| Heart | D0.035 cc | < 46 Gy |
| V39 Gy | < 15 cc | |
| Both lungs | Dmean | < 7 Gy |
| V26 Gy | < 10% | |
| Normal lung | > 1500 cc < 14 Gy | |
| Chest wall* | D0.035 cc | < 68 Gy |
| V45 Gy | < 30 cc |
Planning Dose Constraints - 60 Gy in 8 Fractions
Primary Results
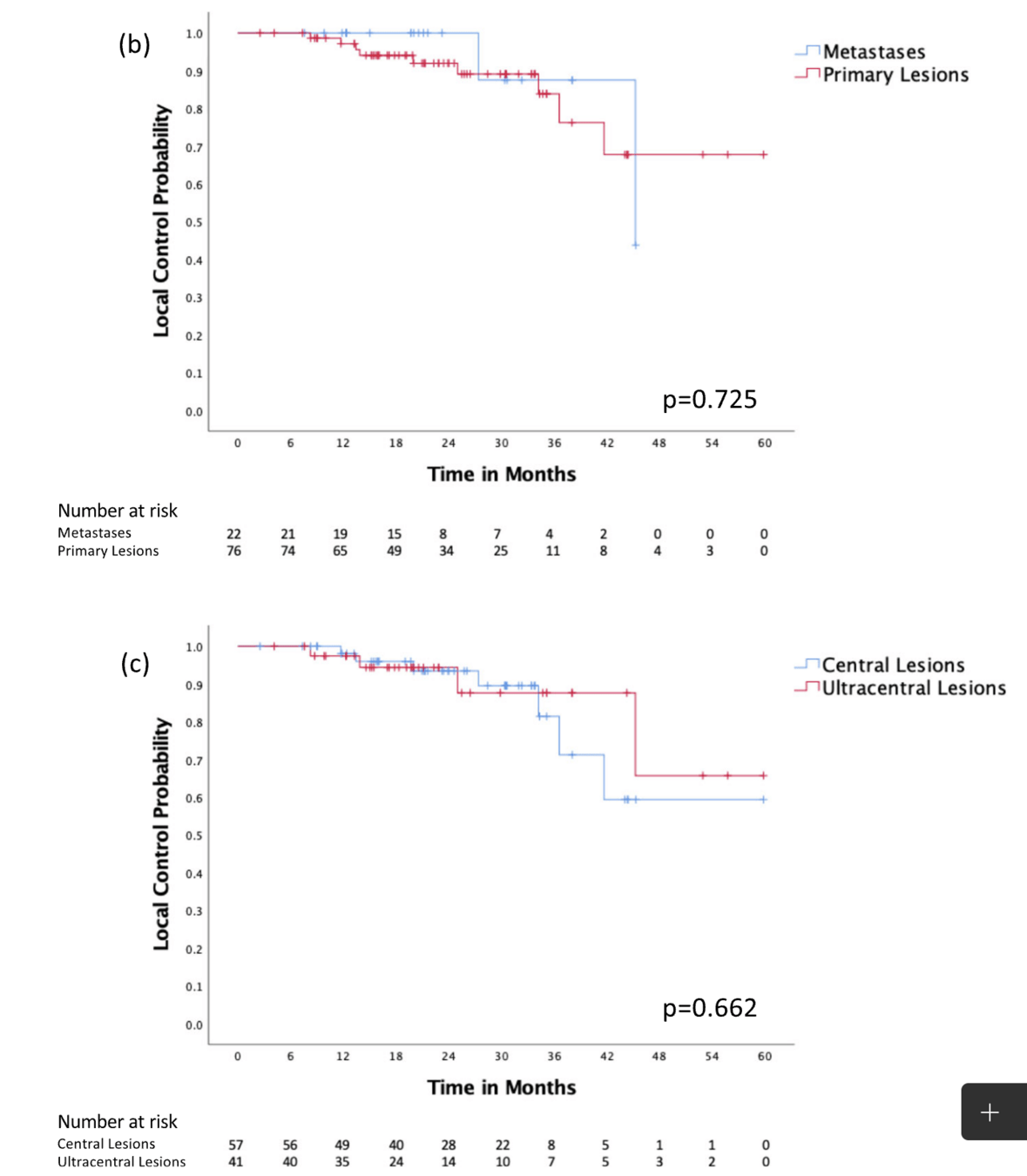
Local Control:
- 1-year: 97.8%
- 2-year: 93.7%
- 3-year: 84.5%
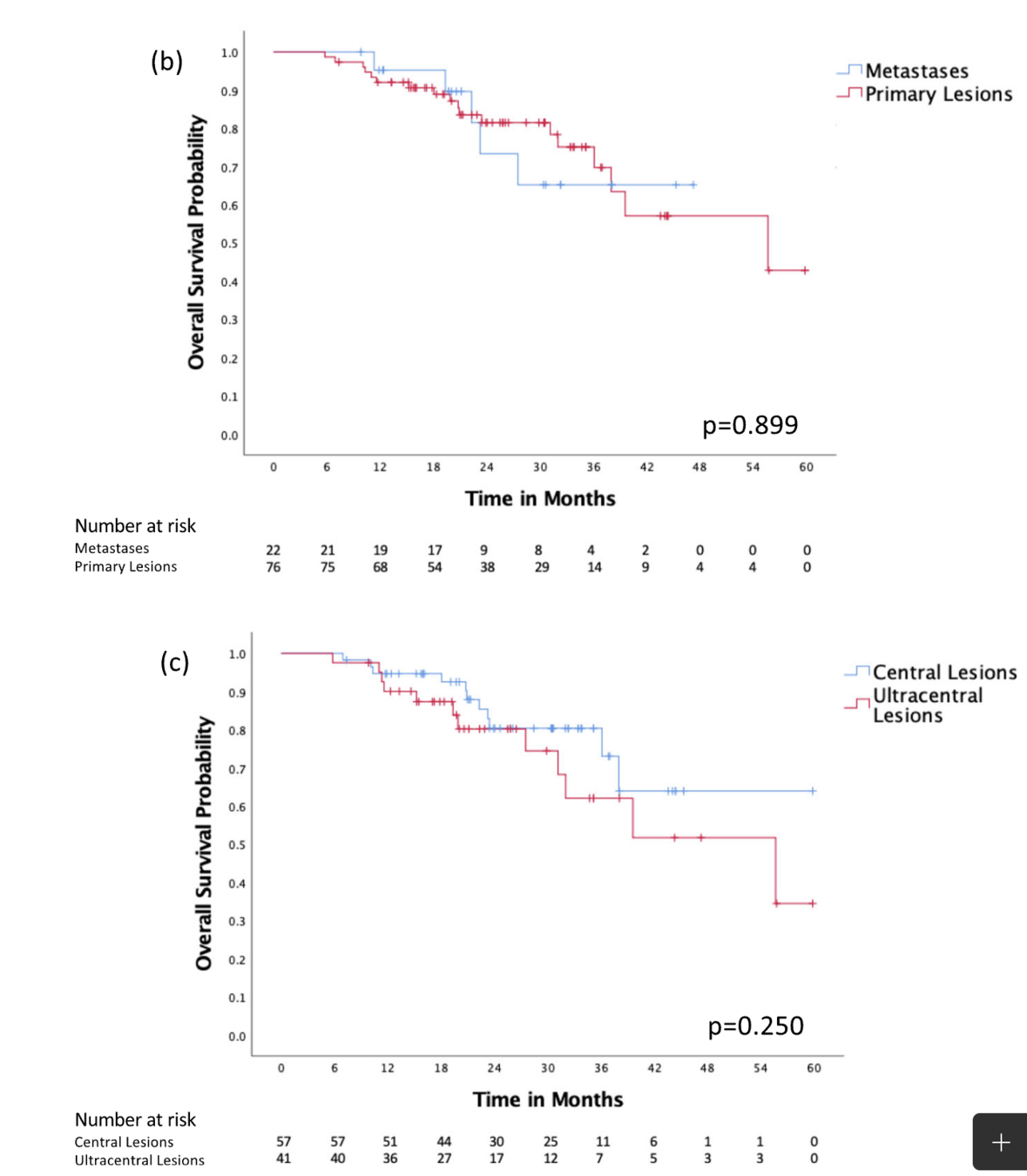
Overall Survival:
- 1-year: 92.7%
- 2-year: 79.8%
- 3-year: 72.9%
- Median: 55.6 months
Primary Results
Local Control:
- 1-year: 97.8%
- 2-year: 93.7%
- 3-year: 84.5%
Overall Survival:
- 1-year: 92.7%
- 2-year: 79.8%
- 3-year: 72.9%
- Median: 55.6 months
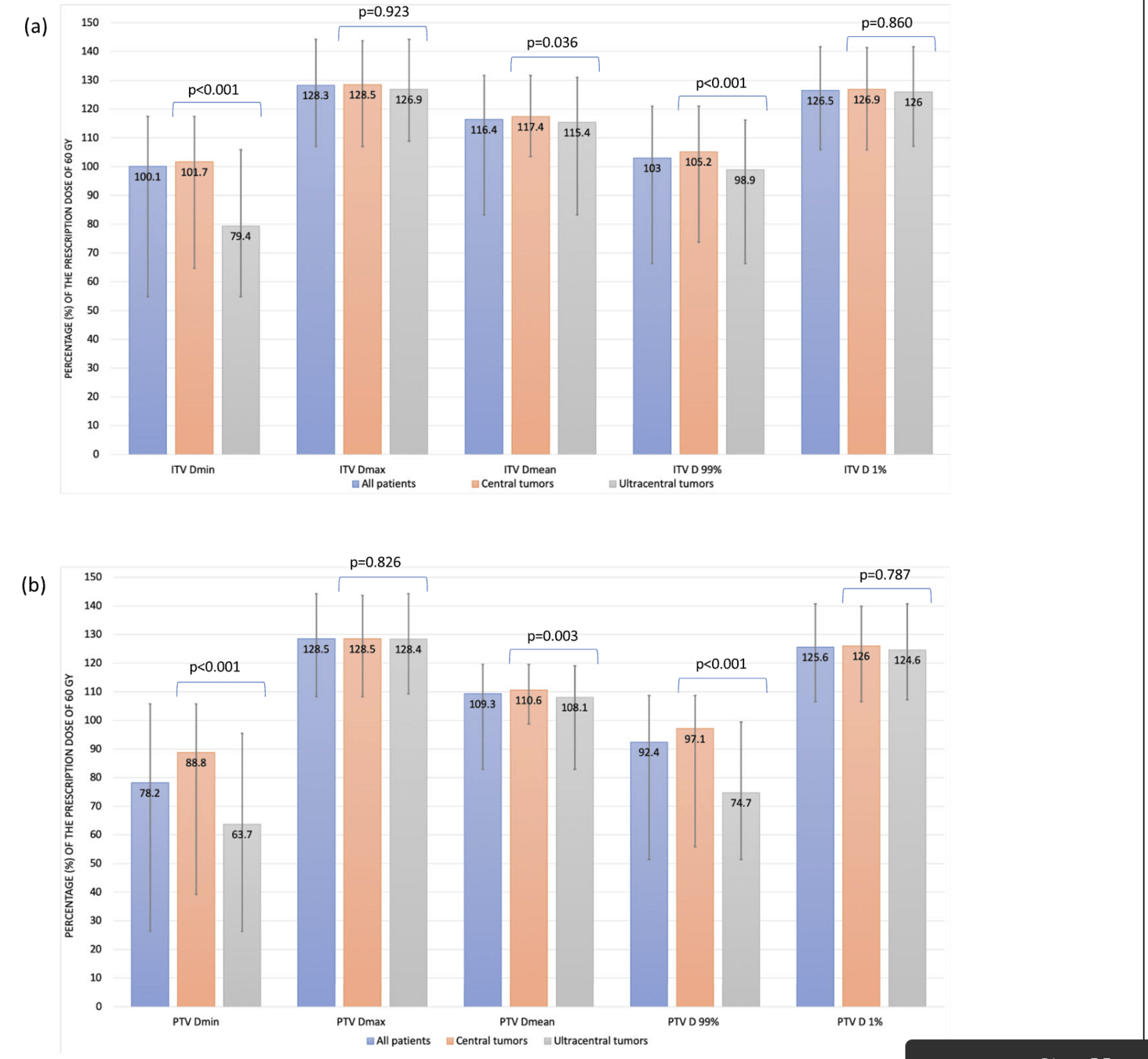
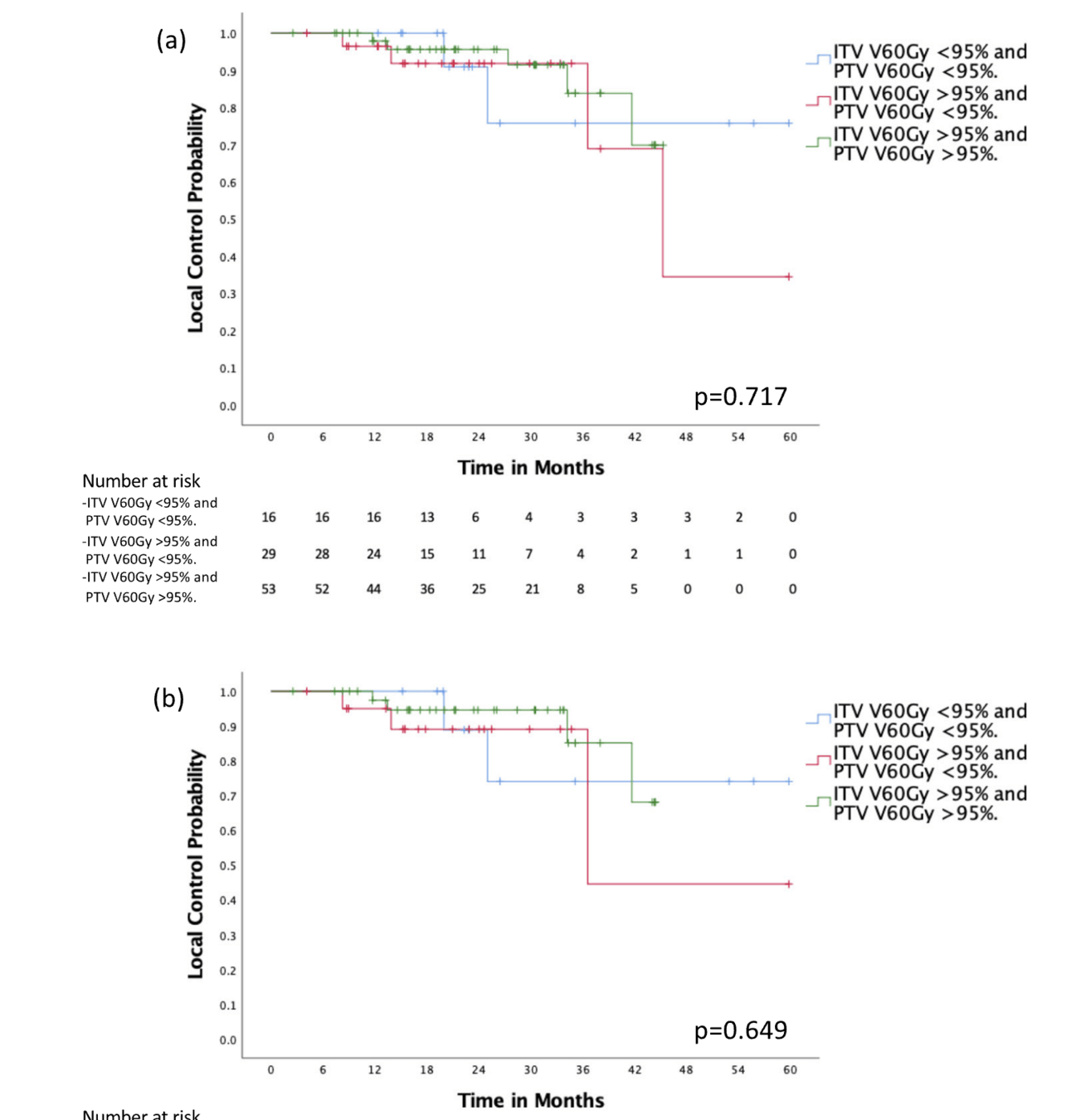
Target Coverage Analysis
- 54.1% - Optimal coverage (ITV & PTV V60Gy >95%)
- 29.6% - Compromised PTV only (ITV V60Gy >95%, PTV <95%)
- 16.3% - Compromised ITV & PTV (both <95%)
- No significant difference in local control between groups (p=0.717)
- ITV size was only significant predictor of local control on multivariate analysis
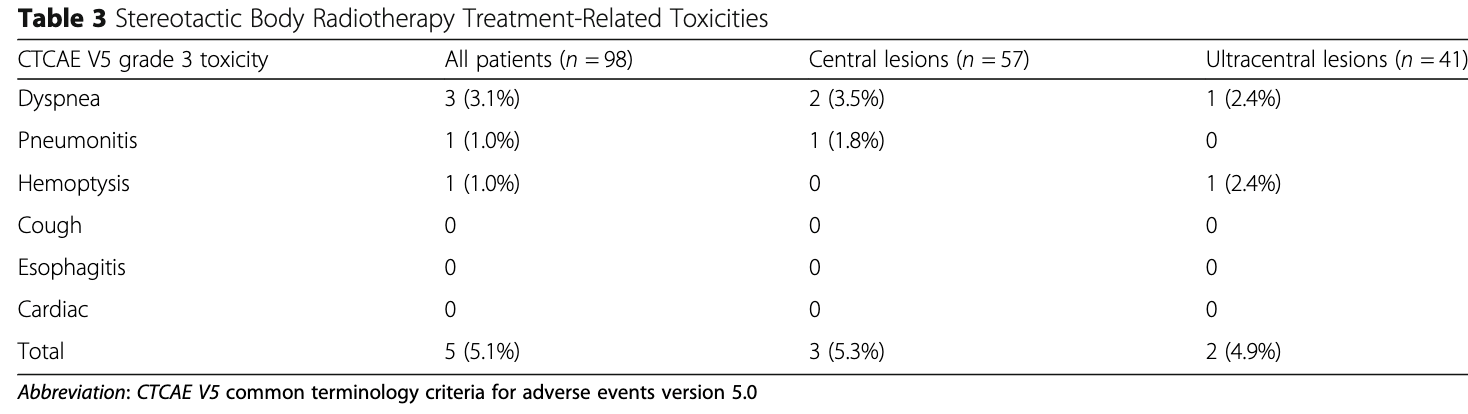
Treatment-Related Toxicity
Central Tumors (n=57)
- Total Grade 3 Events: 3 patients (5.3%)
- Chronic dyspnea requiring O2: 2 patients
- Radiation pneumonitis: 1 patient
- Timing:
- Pneumonitis: 45 days post-RT
- Dyspnea: 117 and 790 days post-RT
Ultracentral Tumors (n=41)
- Total Grade 3 Events: 2 patients (4.9%)
- Chronic dyspnea requiring O2: 1 patient
- Recurrent hemoptysis: 1 patient
- Timing:
- Dyspnea: 182 days post-RT
- Hemoptysis: 346 days post-RT
DVH Parameters and Associated Toxicity
Pulmonary Toxicity
- Grade 3 pneumonitis associated with:
- Mean lung dose > 7 Gy
- V20 > 10%
- Pre-existing ILD increased risk
Bronchial Toxicity
- Hemoptysis risk increased with:
- D0.035cc > 46.3 Gy to bronchial tree
- Tumor abutting bronchial structures
Other Critical Structures
- No high-grade esophageal toxicity
- D0.035cc kept < 40 Gy
- No cardiac toxicity observed
- V39 < 15cc respected
- D0.035cc < 46 Gy maintained
- No great vessel complications
- D0.035cc < 65 Gy achieved
High-Grade & Life-Threatening Toxicities
Study Results
- No Grade 4-5 toxicities observed
- One case of significant hemoptysis (Grade 3)
- Ultracentral location
- Required multiple hospitalizations
- Onset at 346 days post-treatment
- No bronchial/esophageal perforations
- No treatment-related deaths
Risk Mitigation Strategies
- Prioritization of OAR constraints over target coverage
- Use of protracted fractionation (8 fractions)
- Careful patient selection
- Assessment of pre-existing conditions
- Evaluation of tumor location relative to critical structures
- Comparison to Literature:
- Lower rate of severe toxicity than other series
- Particularly compared to 5-fraction regimens
Limitations
- Retrospective design
- Relatively short median follow-up (22.9 months)
- Small number of local failure events (n=11)
- Potential selection bias in patient selection
- Late toxicities may not be captured
- No respiratory gating/tracking used
Outcomes of stereotactic body radiotherapy 60 Gy in 8 fractions when prioritizing organs at risk for central and ultracentral lung tumors
By RadMedSkiier
Outcomes of stereotactic body radiotherapy 60 Gy in 8 fractions when prioritizing organs at risk for central and ultracentral lung tumors
Journal club presentation on Zhao et al. Radiation Oncology 2020
- 38



