ACCSAP Questions:
Stenotic Valves
A 44-year-old man with a history of bicuspid aortic valve (BAV) comes in to your office for initial evaluation. He plays basketball regularly and reports no cardiovascular symptoms. His family history is significant for aortic dissection and repair in his father. On exam his blood pressure is 132/72 mm Hg, heart rate is 68 bpm, and body mass index is 26 kg/m2. He has a 3/6 mid-to-late peaking systolic murmur heard best at the base. He undergoes an echocardiogram which reveals normal biventricular size and function. His peak transaortic velocity is 3.4 m/sec, peak transaortic gradient is 46 mm Hg, and mean trans aortic gradient is 29 mm Hg. His calculated aortic valve area is 1.1 cm2. His ascending aorta measures 5.1 cm.
Which of the following is the next most appropriate step in the care of this patient?
| A. |
Transesophageal echocardiogram. |
| B. |
Cardiac magnetic resonance imaging. |
| C. |
Repeat the echocardiogram in 2 years. |
| D. |
Exercise stress testing. |
| E. |
Surgical referral. |
- Bullet One
- Bullet Two
- Bullet Three
A 44-year-old man with a history of bicuspid aortic valve (BAV) comes in to your office for initial evaluation. He plays basketball regularly and reports no cardiovascular symptoms. His family history is significant for aortic dissection and repair in his father. On exam his blood pressure is 132/72 mm Hg, heart rate is 68 bpm, and body mass index is 26 kg/m2. He has a 3/6 mid-to-late peaking systolic murmur heard best at the base. He undergoes an echocardiogram which reveals normal biventricular size and function. His peak transaortic velocity is 3.4 m/sec, peak transaortic gradient is 46 mm Hg, and mean trans aortic gradient is 29 mm Hg. His calculated aortic valve area is 1.1 cm2. His ascending aorta measures 5.1 cm.
Which of the following is the next most appropriate step in the care of this patient?
| A. |
Transesophageal echocardiogram. |
4.73% |
| B. |
Cardiac magnetic resonance imaging. |
4.14% |
| C. |
Repeat the echocardiogram in 2 years. |
8.28% |
| D. |
Exercise stress testing. |
1.78% |
| E. |
Surgical referral. |
- Bullet One
- Bullet Two
- Bullet Three
In this patient with BAV and aortopathy, consideration of surgical repair should occur when the aortic size is >5.5 cm, there is rapidly increasing size (>0.5 cm/year), or as in this patient, a family history of dissection (Class IIa). If the transthoracic imaging quality is adequate, imaging with magnetic resonance or transesophageal imaging is not indicated. If the patient does not elect to undergo surgery, then repeating the echocardiogram in 1 year is indicated. Given his high level of activity, exercise stress testing is not likely to add additional information about his functional status.
- Bullet One
- Bullet Two
- Bullet Three
A 50-year-old man presents to your office for follow-up of aortic stenosis (AS) and an aortic aneurysm. He is active and exercises regularly without symptoms. He takes no medications.
On physical examination his blood pressure is 110/70 mm Hg with a heart rate of 66 bpm. The carotid contour is normal. A systolic click and grade 2/6 early-peaking systolic ejection murmur are heard at the right upper sternal border. The aortic component of the S2 is preserved. There is no diastolic murmur and no S3 or S4. His peripheral examination shows no edema.
His transthoracic echocardiogram demonstrates bicuspid aortic valve (BAV) and the following:
- Left ventricular ejection fraction of 60%
- Left ventricular end-diastolic dimension of 5.0 cm
- Ascending aorta dimension of 4.6 cm
- Aortic root diameter of 3.8 cm
- Left atrial volume index of 32 ml/m2
- Mean aortic valve gradient of 10 mm Hg
- Aortic valve area of 2.0 cm2
When should the next echocardiogram for surveillance be performed on this patient?
| A. |
2 years. |
|
| C. |
3 years. |
37.87% |
| D. |
5 years. |
1.18% |
- Bullet One
- Bullet Two
- Bullet Three
A 50-year-old man presents to your office for follow-up of aortic stenosis (AS) and an aortic aneurysm. He is active and exercises regularly without symptoms. He takes no medications.
On physical examination his blood pressure is 110/70 mm Hg with a heart rate of 66 bpm. The carotid contour is normal. A systolic click and grade 2/6 early-peaking systolic ejection murmur are heard at the right upper sternal border. The aortic component of the S2 is preserved. There is no diastolic murmur and no S3 or S4. His peripheral examination shows no edema.
His transthoracic echocardiogram demonstrates bicuspid aortic valve (BAV) and the following:
- Left ventricular ejection fraction of 60%
- Left ventricular end-diastolic dimension of 5.0 cm
- Ascending aorta dimension of 4.6 cm
- Aortic root diameter of 3.8 cm
- Left atrial volume index of 32 ml/m2
- Mean aortic valve gradient of 10 mm Hg
- Aortic valve area of 2.0 cm2
When should the next echocardiogram for surveillance be performed on this patient?
| A. |
2 years. |
|
- Bullet One
- Bullet Two
- Bullet Three
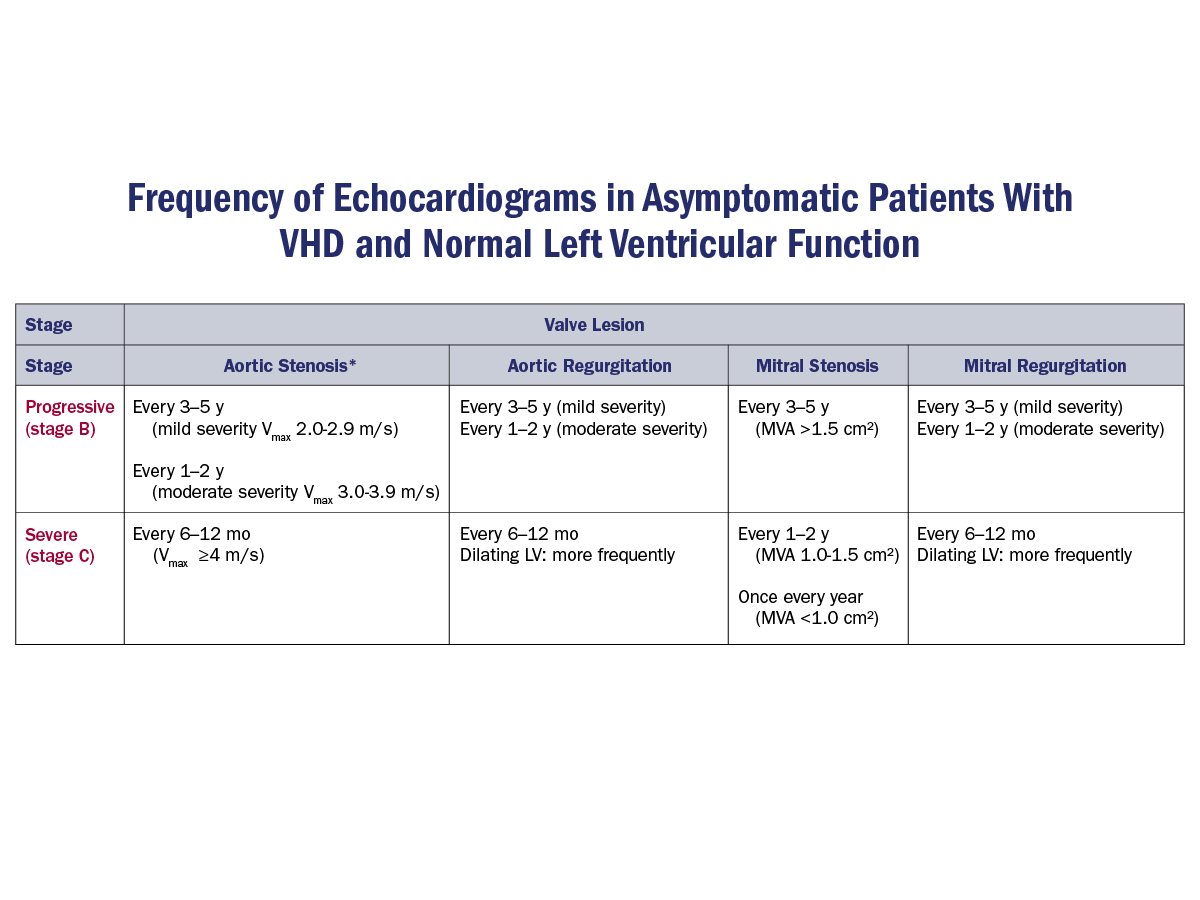
For patients with a BAV and an ascending aortic aneurysm >4.5 cm, annual imaging of the aneurysm is recommended (Class I). Transthoracic echocardiography is considered first-line imaging but cardiac magnetic resonance angiography or computed tomography angiography may be indicated when the morphology of the aortic sinuses, sinotubular junction, and ascending aorta cannot be adequately visualized (Class 1). For patients with mild AS without an ascending aortic aneurysm, serial echocardiography every 3-5 years is recommended in the absence of a change in clinical status or physical findings. Echocardiography is recommended annually for asymptomatic patients with severe AS and every 1-2 years in those with moderate AS. Patients should be advised to report changes in symptoms promptly.
- Bullet One
- Bullet Two
- Bullet Three
Q14.
The patient is an 85-year-old man who presents to the emergency department with dyspnea and malaise. He has a past medical history of severe aortic stenosis status post transcatheter aortic valve replacement approximately 5 years ago. He describes increasing fatigue, dyspnea, and a low grade fever for the past 7 days. On exam, his temperature is 38.1 degrees Celsius (100.6 degrees Fahrenheit), heart rate is 98 bpm, blood pressure is 112/50 mm Hg, respiratory rate is 18 respirations per minute, pulse oximetry is 96% on room air. He has normal S1 and S2 heart sounds with a 2/4 decrescendo diastolic murmur present along the left sternal border. His lungs are clear. The remainder of his physical examination is normal.
In addition to a transthoracic echocardiogram, which of the following is the most appropriate next step in the management of this patient?
|
|
A. |
Empiric antibiotics. |
|
|
|
B. |
Obtain two sets of blood cultures. |
|
|
|
C. |
Administer intravenous furosemide. |
|
|
|
D. |
An influenza nasal swab. |
|
|
|
E. |
A chest X-ray. |
|
- Bullet One
- Bullet Two
- Bullet Three
Q14.
The patient is an 85-year-old man who presents to the emergency department with dyspnea and malaise. He has a past medical history of severe aortic stenosis status post transcatheter aortic valve replacement approximately 5 years ago. He describes increasing fatigue, dyspnea, and a low grade fever for the past 7 days. On exam, his temperature is 38.1 degrees Celsius (100.6 degrees Fahrenheit), heart rate is 98 bpm, blood pressure is 112/50 mm Hg, respiratory rate is 18 respirations per minute, pulse oximetry is 96% on room air. He has normal S1 and S2 heart sounds with a 2/4 decrescendo diastolic murmur present along the left sternal border. His lungs are clear. The remainder of his physical examination is normal.
In addition to a transthoracic echocardiogram, which of the following is the most appropriate next step in the management of this patient?
|
|
A. |
Empiric antibiotics. |
|
|
|
B. |
Obtain two sets of blood cultures. |
|
|
|
C. |
Administer intravenous furosemide. |
|
|
|
D. |
An influenza nasal swab. |
|
|
|
E. |
A chest X-ray. |
|
- Bullet One
- Bullet Two
- Bullet Three
Q14.
The patient has a prosthetic aortic valve and is at risk for infective endocarditis (IE). It is important that two sets of blood cultures are obtained in patients who are at risk for IE, including those with congenital or acquired valvular heart disease, previous IE, prosthetic heart valves, certain congenital or heritable heart malformations, immunodeficiency states, or who are injection drug users. Blood cultures are positive in >90% of patients with IE and should be obtained at separate time intervals prior to the administration of antibiotics. This patient has an unexplained fever for >48 hours and a left-sided regurgitant murmur with a high likelihood for IE. Thus, the most appropriate next step in management is to obtain two sets of blood cultures.
Blood cultures must be obtained before starting empiric antibiotics. He has no evidence of pulmonary edema and therefore furosemide is not warranted. While a chest X-ray and a flu swab may be considered, neither are the essential first steps in management of this patient.
- Bullet One
- Bullet Two
- Bullet Three
A 76-year-old man with a past history of coronary artery bypass grafting 20 years ago is admitted with progressive dyspnea on exertion. He has diabetes mellitus, stage 3 chronic kidney disease, hypertension, dyslipidemia, and had a stroke 5 years ago that left him with residual left-sided weakness. His echocardiogram shows a mildly dilated left ventricle, a left ventricular ejection fraction of 25-30% with regional variations, and severe aortic stenosis (AS) with a mean gradient of 50 mm Hg and a calculated valve area of 0.8 cm2. Coronary angiography demonstrates patent grafts and severe native vessel disease.
What is the most appropriate next step in the management of this patient?
| A. |
Transcatheter aortic valve replacement. |
| B. |
Valved apical-aortic conduit. |
| C. |
Balloon aortic valvuloplasty. |
| D. |
Left ventricular assist device. |
| E. |
Dobutamine infusion. |
- Bullet One
- Bullet Two
- Bullet Three
A 76-year-old man with a past history of coronary artery bypass grafting 20 years ago is admitted with progressive dyspnea on exertion. He has diabetes mellitus, stage 3 chronic kidney disease, hypertension, dyslipidemia, and had a stroke 5 years ago that left him with residual left-sided weakness. His echocardiogram shows a mildly dilated left ventricle, a left ventricular ejection fraction of 25-30% with regional variations, and severe aortic stenosis (AS) with a mean gradient of 50 mm Hg and a calculated valve area of 0.8 cm2. Coronary angiography demonstrates patent grafts and severe native vessel disease.
What is the most appropriate next step in the management of this patient?
| A. |
Transcatheter aortic valve replacement. |
| B. |
Valved apical-aortic conduit. |
| C. |
Balloon aortic valvuloplasty. |
| D. |
Left ventricular assist device. |
| E. |
Dobutamine infusion. |
- Bullet One
- Bullet Two
- Bullet Three
This patient has severe symptomatic AS. The recommendation for either surgical aortic valve replacement (AVR) or transcather AVR among patients aged 65 to 80 years old with severe, symptomatic AS (stage D), after consideration by a heart valve team, is a Class I (LOE A) in the 2020 guideline for patients with valvular heart disease.
Percutaneous aortic balloon dilation has an important role in treating children, adolescents, and young adults with AS, but its role in treating older patients is very limited. The mechanism by which balloon dilation modestly reduces the severity of stenosis in older patients is by fracturing calcific deposits within the valve leaflets and, to a minor degree, stretching the annulus and separating the calcified or fused commissures. Immediate hemodynamic results include a moderate reduction in the transvalvular pressure gradient, but the postdilation valve area rarely exceeds 1.0 cm2. Despite the modest change in valve area, an early symptomatic improvement usually occurs. However, serious acute complications, including acute severe aortic regurgitation, restenosis, and clinical deterioration, occur within 6-12 months in most patients. Therefore, in patients with AS, percutaneous aortic balloon dilation is not a substitute for AVR.
Apico-aortic conduits to bypass the diseased aortic valve are a historical curiosity and no longer performed in the era of transcatheter aortic valve therapy.
Left ventricular assist devices (LVAD) are indicated for end-stageheart failure patients only when all other therapeutic options have been exhausted. In this case AVR would be expected to result in improvement in symptoms, myocardial performance, and mortality, so AVR would be preferred to LVAD.
Palliative care with inotropic support would not be expected to improve quality of life or mortality in a patient with severe symptomatic AS.
- Bullet One
- Bullet Two
- Bullet Three
A 48-year-old man presents for evaluation of bicuspid aortic stenosis because of worsening shortness of breath over the past few months. He is an avid motorcyclist and despite a recent accident, would never consider not riding. His echocardiogram 6 months ago showed normal biventricular function, a peak transaortic velocity of 4.2 m/sec, peak transaortic gradient of 72 mm Hg, mean gradient of 48 mm Hg, and calculated aortic valve area of 0.8 cm2. His aortic root is a normal size. His past medical history is significant for hypothyroidism. On exam today his blood pressure is 128/66 mm Hg, heart rate is 72 bpm, and he has a normal S1 and a late peaking harsh systolic murmur. His lungs are clear to auscultation bilaterally and he has no peripheral edema.
In a shared decision-making approach, which of the following is the most likely approach to be aligned with the patient's preferences?
| A. |
Transesophageal echocardiogram. |
| B. |
Repeat transthoracic echocardiogram in 1 year. |
| C. |
Bioprosthetic aortic valve replacement. |
| D. |
Exercise stress testing. |
| E. |
Mechanical aortic valve replacement. |
- Bullet One
- Bullet Two
- Bullet Three
A 48-year-old man presents for evaluation of bicuspid aortic stenosis because of worsening shortness of breath over the past few months. He is an avid motorcyclist and despite a recent accident, would never consider not riding. His echocardiogram 6 months ago showed normal biventricular function, a peak transaortic velocity of 4.2 m/sec, peak transaortic gradient of 72 mm Hg, mean gradient of 48 mm Hg, and calculated aortic valve area of 0.8 cm2. His aortic root is a normal size. His past medical history is significant for hypothyroidism. On exam today his blood pressure is 128/66 mm Hg, heart rate is 72 bpm, and he has a normal S1 and a late peaking harsh systolic murmur. His lungs are clear to auscultation bilaterally and he has no peripheral edema.
In a shared decision-making approach, which of the following is the most likely approach to be aligned with the patient's preferences?
| A. |
Transesophageal echocardiogram. |
| B. |
Repeat transthoracic echocardiogram in 1 year. |
| C. |
Bioprosthetic aortic valve replacement. |
| D. |
Exercise stress testing. |
| E. |
Mechanical aortic valve replacement. |
- Bullet One
- Bullet Two
- Bullet Three
A 29-year-old woman presented for prenatal counseling. She exercises by running three miles 5 days per week without limitations. She has a history of a heart murmur since childhood and a previous echocardiogram suggesting ‘enlargement of the heart'.
Her physical exam reveals normal jugular venous pressure and contour. Precordial palpation is unremarkable. Auscultation along the left sternal border reveals a high-pitched sound just after S1 followed by a murmur.
Which of the following maneuvers will best identify the associated valvular abnormality in this patient?
| A. |
Standing. |
| B. |
Inspiration. |
| C. |
Hand grip. |
| D. |
Valsalva. |
| E. |
Squatting. |
- Bullet One
- Bullet Two
- Bullet Three
A 29-year-old woman presented for prenatal counseling. She exercises by running three miles 5 days per week without limitations. She has a history of a heart murmur since childhood and a previous echocardiogram suggesting ‘enlargement of the heart'.
Her physical exam reveals normal jugular venous pressure and contour. Precordial palpation is unremarkable. Auscultation along the left sternal border reveals a high-pitched sound just after S1 followed by a murmur.
Which of the following maneuvers will best identify the associated valvular abnormality in this patient?
| A. |
Standing. |
| B. |
Inspiration. |
| C. |
Hand grip. |
| D. |
Valsalva. |
| E. |
Squatting. |
- Bullet One
- Bullet Two
- Bullet Three
This patient has a right-sided ejection click and ejection murmur. Ejection clicks are high-pitched sounds that occur at the moment of maximal opening of the aortic or pulmonary valves. They are heard just after the first heart sound. The sounds occur in the presence of a dilated aorta or pulmonary artery or in the presence of a bicuspid or flexible stenotic aortic or pulmonary valve. In this case, the ejection click and murmur are heard only at the left sternal border, consistent with pulmonic rather than aortic stenosis.
The most helpful distinguishing feature of a pulmonary ejection sound is its decreased intensity, or even its disappearance during the inspiratory phase of respiration. During expiration, the valve opens rapidly from its fully closed position; sudden "halting" of this rapid opening movement is associated with a maximal intensity of the ejection sound. With inspiration, the increased venous return to the right ventricle (RV) augments the effect of right atrial systole and causes partial opening of the pulmonary valve prior to ventricular systole. The lack of a sharp opening movement of the pulmonary valve explains the decreased intensity of the pulmonary ejection sound during inspiration. Thus, the best way to confirm that the patient has pulmonic stenosis is to assess the intensity of the murmur on inspiration.
The other maneuvers listed would not be expected to affect the auscultation of a right-sided murmur.
- Bullet One
- Bullet Two
- Bullet Three
Sustained hand grip for 20-30 seconds leads to an increase in systemic vascular resistance, arterial pressure, cardiac output, and left ventricular (LV) volume and filling pressure. Hand grip is most useful in differentiating between the ejection systolic murmur of aortic stenosis and the regurgitant murmur of mitral regurgitation (MR). Intensity of the murmur of aortic stenosis tends to decrease along with a decreased transvalvular pressure gradient, while the severity and murmur of MR increase.
During the straining phase, phase 2, of Valsalva there is a decrease in venous return, RV and LV volumes, stroke volumes, mean arterial pressure, and pulse pressure; this is associated with a reflex increase in heart rate. The murmur of hypertrophic cardiomyopathy (HCM) increases in intensity as the LV outflow size decreases with a decreased venous return. In mitral valve prolapse (MVP) there is an early onset of the click and murmur due to the decrease in LV volume.
Abrupt standing from the supine position decreases venous return to the heart and, consequently, RV and LV diastolic volumes and stroke volumes decline. There also may be a fall in arterial pressure and a reflex increase in heart rate. This will cause similar effects to phase 2 of a Valsalva maneuver.
Squatting from a standing position is associated with a simultaneous increase in venous return (preload) and systemic vascular resistance (afterload) and a rise in arterial pressure. In HCM, intensity of the ejection systolic murmur declines because of an increased LV volume and arterial pressure, which increase the effective orifice size of the outflow tract. In patients with MVP there is a delay in the onset of the click and a shortening of the late systolic murmur. These changes reflect the delay in prolapse induced by the increase in preload. However, as MR becomes more severe, the murmur may increase in intensity with squatting because of the increase in afterload.
- Bullet One
- Bullet Two
- Bullet Three
Sustained hand grip for 20-30 seconds leads to an increase in systemic vascular resistance, arterial pressure, cardiac output, and left ventricular (LV) volume and filling pressure. Hand grip is most useful in differentiating between the ejection systolic murmur of aortic stenosis and the regurgitant murmur of mitral regurgitation (MR). Intensity of the murmur of aortic stenosis tends to decrease along with a decreased transvalvular pressure gradient, while the severity and murmur of MR increase.
During the straining phase, phase 2, of Valsalva there is a decrease in venous return, RV and LV volumes, stroke volumes, mean arterial pressure, and pulse pressure; this is associated with a reflex increase in heart rate. The murmur of hypertrophic cardiomyopathy (HCM) increases in intensity as the LV outflow size decreases with a decreased venous return. In mitral valve prolapse (MVP) there is an early onset of the click and murmur due to the decrease in LV volume.
Abrupt standing from the supine position decreases venous return to the heart and, consequently, RV and LV diastolic volumes and stroke volumes decline. There also may be a fall in arterial pressure and a reflex increase in heart rate. This will cause similar effects to phase 2 of a Valsalva maneuver.
Squatting from a standing position is associated with a simultaneous increase in venous return (preload) and systemic vascular resistance (afterload) and a rise in arterial pressure. In HCM, intensity of the ejection systolic murmur declines because of an increased LV volume and arterial pressure, which increase the effective orifice size of the outflow tract. In patients with MVP there is a delay in the onset of the click and a shortening of the late systolic murmur. These changes reflect the delay in prolapse induced by the increase in preload. However, as MR becomes more severe, the murmur may increase in intensity with squatting because of the increase in afterload.
- Bullet One
- Bullet Two
- Bullet Three
You are asked to see a 59-year-old woman with aortic stenosis (AS). For the past 3 months she has noted progressive shortness of breath with daily household chores. Her medical history is significant for hypertension. She currently takes losartan 50 mg and aspirin 81 mg daily.
Her vital signs are a blood pressure of 124/72 mm Hg with a heart rate of 84 bpm. Her jugular veins are not distended. Carotid upstrokes are delayed. Her lungs are clear to auscultation. The apical impulse is sustained and displaced 2 cm to the left of the mid-clavicular line. A grade 3/6 harsh, late-peaking systolic ejection murmur is heard throughout the precordium, loudest at the right upper sternal border, and radiates to the carotids. There is no diastolic murmur. The rest of her physical examination is normal.
Her laboratory studies include a hemoglobin of 13.1 g/dl and a creatinine of 0.8 mg/dl. Her echocardiogram demonstrates concentric left ventricular hypertrophy with an ejection fraction of 65%. There is a bicuspid aortic valve with AS; peak velocity is 4.2 m/sec with a mean gradient of 42 mm Hg and a calculated valve area of 0.7 cm2. Coronary angiography reveals a 60% angiographic stenosis of the mid left anterior descending (LAD) artery; fractional flow reserve (FFR) was 0.89. Her estimated operative mortality for cardiac surgery is calculated at 1.6%.
Which of the following is the next best step in the management of this patient?
| A. |
Surgical aortic valve replacement plus coronary artery bypass grafting. |
| B. |
Transcatheter aortic valve implantation plus percutaneous coronary intervention. |
| C. |
Surgical aortic valve replacement. |
| D. |
Transcatheter aortic valve implantation. |
- Bullet One
- Bullet Two
- Bullet Three
You are asked to see a 59-year-old woman with aortic stenosis (AS). For the past 3 months she has noted progressive shortness of breath with daily household chores. Her medical history is significant for hypertension. She currently takes losartan 50 mg and aspirin 81 mg daily.
Her vital signs are a blood pressure of 124/72 mm Hg with a heart rate of 84 bpm. Her jugular veins are not distended. Carotid upstrokes are delayed. Her lungs are clear to auscultation. The apical impulse is sustained and displaced 2 cm to the left of the mid-clavicular line. A grade 3/6 harsh, late-peaking systolic ejection murmur is heard throughout the precordium, loudest at the right upper sternal border, and radiates to the carotids. There is no diastolic murmur. The rest of her physical examination is normal.
Her laboratory studies include a hemoglobin of 13.1 g/dl and a creatinine of 0.8 mg/dl. Her echocardiogram demonstrates concentric left ventricular hypertrophy with an ejection fraction of 65%. There is a bicuspid aortic valve with AS; peak velocity is 4.2 m/sec with a mean gradient of 42 mm Hg and a calculated valve area of 0.7 cm2. Coronary angiography reveals a 60% angiographic stenosis of the mid left anterior descending (LAD) artery; fractional flow reserve (FFR) was 0.89. Her estimated operative mortality for cardiac surgery is calculated at 1.6%. Which of the following is the next best step in the management of this patient?
| A. |
Surgical aortic valve replacement plus coronary artery bypass grafting. |
| B. |
Transcatheter aortic valve implantation plus percutaneous coronary intervention. |
| C. |
Surgical aortic valve replacement. |
| D. |
Transcatheter aortic valve implantation. |
- Bullet One
- Bullet Two
- Bullet Three
You are asked to see a 59-year-old woman with aortic stenosis (AS). For the past 3 months she has noted progressive shortness of breath with daily household chores. Her medical history is significant for hypertension. She currently takes losartan 50 mg and aspirin 81 mg daily.
Her vital signs are a blood pressure of 124/72 mm Hg with a heart rate of 84 bpm. Her jugular veins are not distended. Carotid upstrokes are delayed. Her lungs are clear to auscultation. The apical impulse is sustained and displaced 2 cm to the left of the mid-clavicular line. A grade 3/6 harsh, late-peaking systolic ejection murmur is heard throughout the precordium, loudest at the right upper sternal border, and radiates to the carotids. There is no diastolic murmur. The rest of her physical examination is normal.
Her laboratory studies include a hemoglobin of 13.1 g/dl and a creatinine of 0.8 mg/dl. Her echocardiogram demonstrates concentric left ventricular hypertrophy with an ejection fraction of 65%. There is a bicuspid aortic valve with AS; peak velocity is 4.2 m/sec with a mean gradient of 42 mm Hg and a calculated valve area of 0.7 cm2. Coronary angiography reveals a 60% angiographic stenosis of the mid left anterior descending (LAD) artery; fractional flow reserve (FFR) was 0.89. Her estimated operative mortality for cardiac surgery is calculated at 1.6%. Which of the following is the next best step in the management of this patient?
| A. |
Surgical aortic valve replacement plus coronary artery bypass grafting. |
| B. |
Transcatheter aortic valve implantation plus percutaneous coronary intervention. |
| C. |
Surgical aortic valve replacement. |
| D. |
Transcatheter aortic valve implantation. |
- Bullet One
- Bullet Two
- Bullet Three
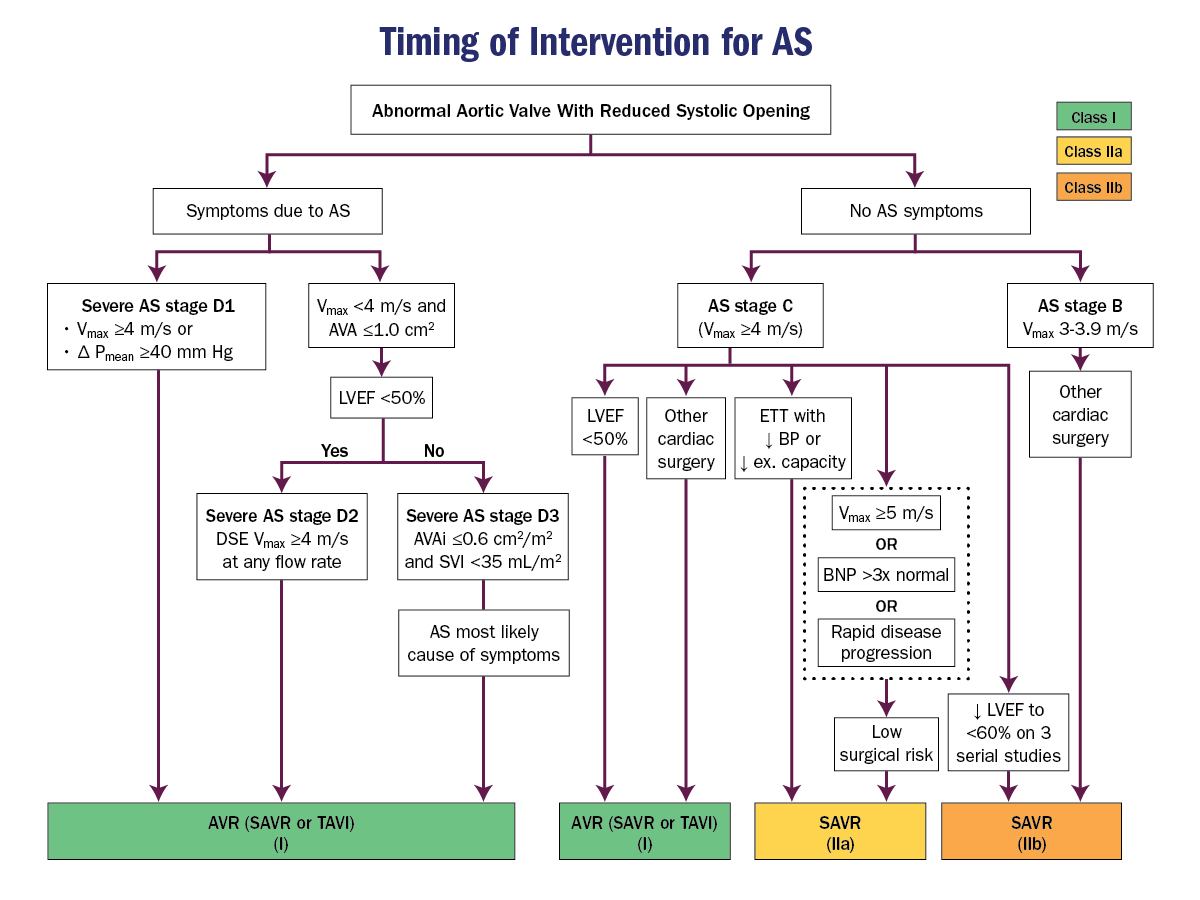
The patient has symptomatic, severe AS and nonobstructive coronary artery disease involving her LAD artery based on an FFR of >0.8. Her surgical risk is low (<4%). The most appropriate therapy is surgical aortic valve replacement (AVR; Class I) (Figure 1). Transcather aortic valve implantation (TAVI) is a Class I indication for treating AS in patients at prohibitive surgical risk as well as high surgical risk (Society of Thoracic Surgeons Predicted Risk of Mortality score >8%), but also patient age and life expectancy, depending on patient values and preferences. TAVI is not currently recommended for the treatment of patients with AS and low surgical risk and age <65. This patient needs medical therapy for her coronary disease.
- Bullet One
- Bullet Two
- Bullet Three
- Bullet One
- Bullet Two
- Bullet Three
- Bullet One
- Bullet Two
- Bullet Three
A 30-year-old woman presents to your clinic with progressive shortness of breath. The symptoms started 2 years ago and now occur with minimal activity. She has no significant past medical history. She is on no medications. Her physical exam reveals an early opening snap followed by a low frequency murmur.
A cardiac echocardiogram showed thickening of the mitral valve leaflets with doming. The mean gradient was 5 mm Hg at a ventricular rate of 60 bpm.
What is the next best step in the management of this patient?
| A. |
Exercise stress myocardial perfusion imaging. |
| B. |
Transesophageal echocardiography. |
| C. |
Right heart catheterization. |
| D. |
Exercise stress echocardiography. |
| E. |
Polysomnography. |
- Bullet One
- Bullet Two
- Bullet Three
A 30-year-old woman presents to your clinic with progressive shortness of breath. The symptoms started 2 years ago and now occur with minimal activity. She has no significant past medical history. She is on no medications. Her physical exam reveals an early opening snap followed by a low frequency murmur.
A cardiac echocardiogram showed thickening of the mitral valve leaflets with doming. The mean gradient was 5 mm Hg at a ventricular rate of 60 bpm.
What is the next best step in the management of this patient?
| A. |
Exercise stress myocardial perfusion imaging. |
| B. |
Transesophageal echocardiography. |
| C. |
Right heart catheterization. |
| D. |
Exercise stress echocardiography. |
| E. |
Polysomnography. |
- Bullet One
- Bullet Two
- Bullet Three
A 30-year-old woman presents to your clinic with progressive shortness of breath. The symptoms started 2 years ago and now occur with minimal activity. She has no significant past medical history. She is on no medications. Her physical exam reveals an early opening snap followed by a low frequency murmur.
A cardiac echocardiogram showed thickening of the mitral valve leaflets with doming. The mean gradient was 5 mm Hg at a ventricular rate of 60 bpm.
What is the next best step in the management of this patient?
| A. |
Exercise stress myocardial perfusion imaging. |
| B. |
Transesophageal echocardiography. |
| C. |
Right heart catheterization. |
| D. |
Exercise stress echocardiography. |
| E. |
Polysomnography. |
- Bullet One
- Bullet Two
- Bullet Three
This patient has symptoms and exam findings consistent with significant mitral stenosis (MS), but her resting echocardiographic findings are suggestive of mild MS. Exercise testing with Doppler or invasive hemodynamic assessment is recommended to evaluate the response of the mean mitral gradient and pulmonary artery pressure in patients with MS when there is a discrepancy between resting Doppler echocardiographic findings and clinical symptoms or signs.
Right heart catheterization is an invasive test and should be reserved for cases of indeterminate noninvasive test findings. Furthermore, direct measurement of left ventricular diastolic pressure would be required to assess the mitral valve; right heart catheterization alone would be inadequate in this case.
She does not report any daytime somnolence that point to sleep apnea, so polysomnography would not be the next best step.
Stress perfusion imaging to test for coronary ischemia would not be expected to explain her valve findings.
Transesophageal echocardiography will be required to plan therapy once a diagnosis of severe MS is made, but will not resolve the discrepancy between her resting echocardiogram findings and her symptoms.
- Bullet One
- Bullet Two
- Bullet Three
A 60-year-old man presents for evaluation of a murmur. He exercises by walking his dog two miles daily without limitations. He has a history of hypertension and hyperlipidemia. His medications include amlodipine 5 mg daily and atorvastatin 20 mg daily.
On examination, his heart rate is 70 bpm, blood pressure is 128/80 mm Hg, and jugular venous pressure is 4 cm H20. His lungs are clear. His cardiac exam shows a soft systolic ejection murmur radiating to the carotid arteries. His extremities have no edema.
His echocardiogram shows an ejection fraction of 60% and aortic stenosis (AS) with a peak velocity of 2.3 m/sec, mean gradient of 13 mm Hg, and a valve area of 1.8 cm2.
In the absence of new symptoms, what is the appropriate interval for a repeat echocardiogram in this patient?
| A. |
2 years. |
| B. |
6 months. |
| C. |
3 years. |
| D. |
6 years. |
| E. |
1 year. |
- Bullet One
- Bullet Two
- Bullet Three
A 60-year-old man presents for evaluation of a murmur. He exercises by walking his dog two miles daily without limitations. He has a history of hypertension and hyperlipidemia. His medications include amlodipine 5 mg daily and atorvastatin 20 mg daily.
On examination, his heart rate is 70 bpm, blood pressure is 128/80 mm Hg, and jugular venous pressure is 4 cm H20. His lungs are clear. His cardiac exam shows a soft systolic ejection murmur radiating to the carotid arteries. His extremities have no edema.
His echocardiogram shows an ejection fraction of 60% and aortic stenosis (AS) with a peak velocity of 2.3 m/sec, mean gradient of 13 mm Hg, and a valve area of 1.8 cm2.
In the absence of new symptoms, what is the appropriate interval for a repeat echocardiogram in this patient?
| A. |
2 years. |
| B. |
6 months. |
| C. |
3 years. |
| D. |
6 years. |
| E. |
1 year. |
- Bullet One
- Bullet Two
- Bullet Three
The timing of periodic clinical evaluation of patients with severe asymptomatic AS depends on comorbidities and patient-specific factors. Transthoracic echocardiogram for re-evaluation of asymptomatic patients with AS with normal left ventricular systolic function who have no change in signs or symptoms is performed at intervals of 6 months to 1 year when aortic velocity is greater than equal to 4.0 m/sec (stage C), 1-2 years when aortic velocity is 3.0-3.9 m/sec (stage B), and 3-5 years when aortic velocity is 2.0-2.9 m/sec (stage B; Table 1).
Valvular AS is a progressive disease, and an increase in hemodynamic severity is inevitable once even mild AS is present. The rate of progression of the stenotic lesion has been estimated in a variety of invasive and noninvasive studies. When severe AS is present (aortic velocity of 4.0 m/sec), the rate of progression to symptoms is high with an event-free survival of only 30-50% at 2 years. Therefore, patients with asymptomatic severe AS require frequent monitoring for progressive disease because symptom onset may be insidious and not recognized by the patient.
Once even moderate AS is present (aortic velocity between 3.0-3.9 m/sec), the average rate of progression is an increase in velocity of 0.3 m/sec per year, an increase in mean pressure gradient of 7 mm Hg per year, and a decrease in valve area of 0.1 cm2 per year. There is marked individual variability in the rate of hemodynamic change. Progression of AS can be more rapid in older patients and in those with more severe leaflet calcification. Because it is not possible to predict the exact rate of progression in an individual patient, regular clinical and echocardiographic follow-up is mandatory in all patients with asymptomatic mild-to-moderate AS.
In his patient with mild (Stage B) AS, a repeat echocardiogram in 3-5 years is appropriate.
ACCSAP Questions:
By Seana Nelson
ACCSAP Questions:
- 95



