Atrial Fibrillation
Case
You are seeing a 68 year old male in the emergency medicine department who presents with anxiety. His brother developed atrial fibrillation and he is wondering whether he should have screening. How do you counsel him and if screening is appropriate how would you do so?

Screening

Screening in Stroke
- At least 24 hours of ambulatory ECG monitoring
- Prolonged monitoring in select older patients if AF is still suspected
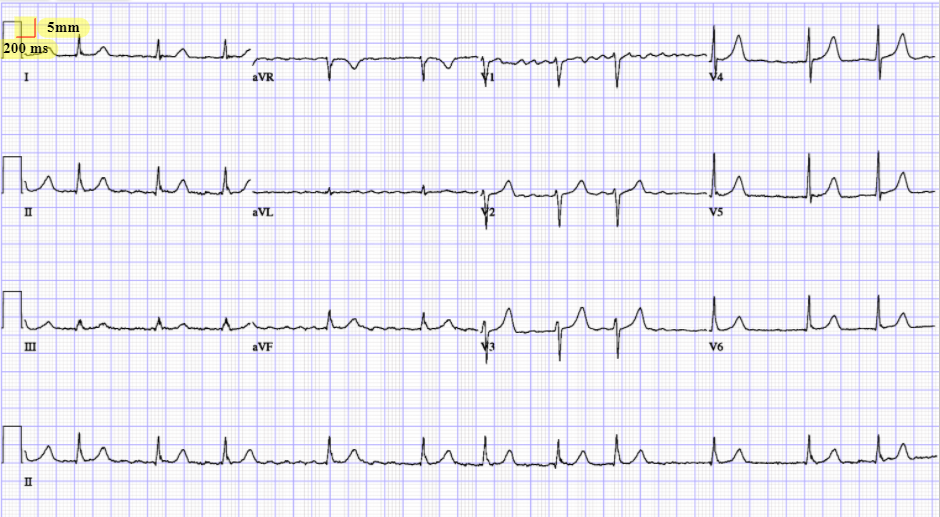
ECG
How will you workup this patient in Emerg?
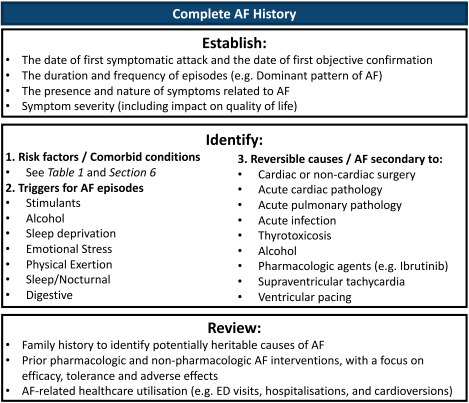
Workup
CCC QoL
- Know the score exists and that you would assess QoL
- Important aspect of outpatient management

Case
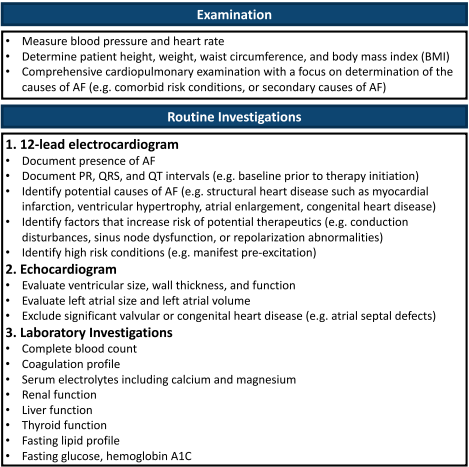
What are risk factors for atrial fibrillation and how would you counsel the patient on modifying them?

We suggest a structured, integrated, multidisciplinary, patient-focused approach to care should be implemented for patients with AF (Weak Recommendation; Moderate-Quality Evidence).
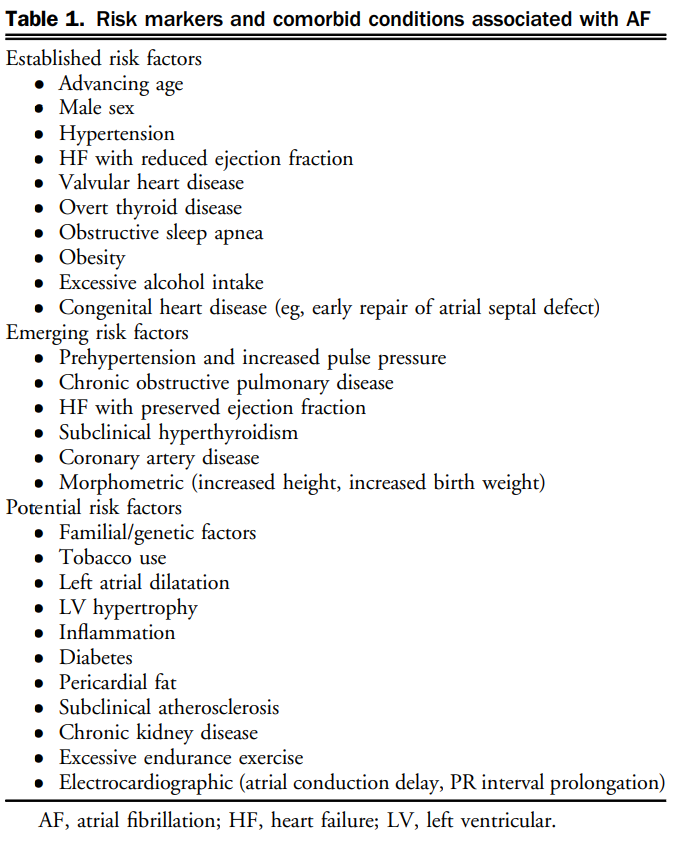
Risk Factors
Case
You have initiated a multi-disciplinary non-pharmacologic plan for the patient and now move to the pharmacologic component. How will you manage this patient?

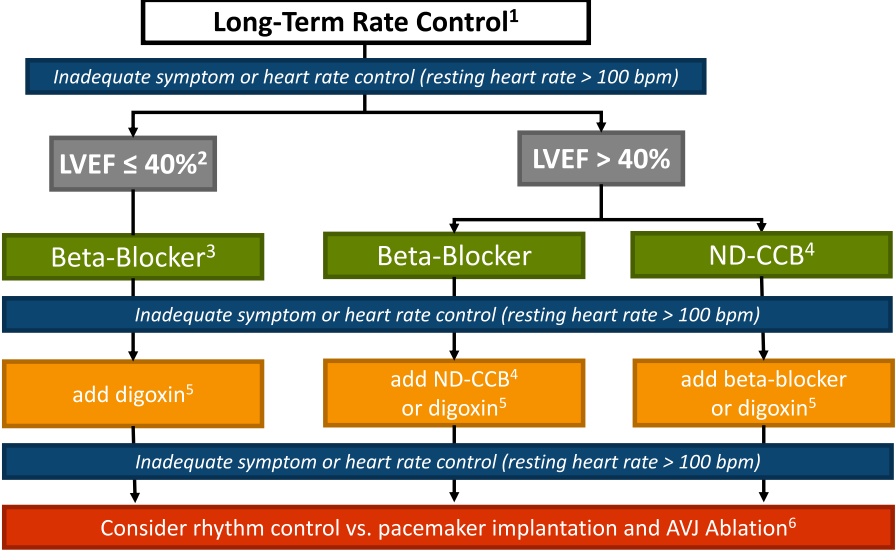
Rate vs Rhythm Control

I.V Procainamide
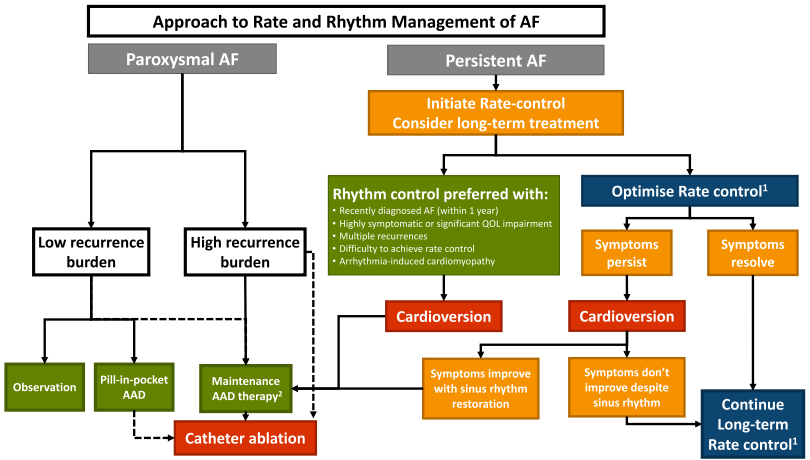
- New recommendation: We suggest that a rhythm control strategy be considered for most stable patients with recent-onset AF (<1 year)
- Evolving evidence, but broadly consider rhythm control in symptomatic, cannot rate control or paroxysmal. Unlikely to have to prescribe.

Anticoagulation
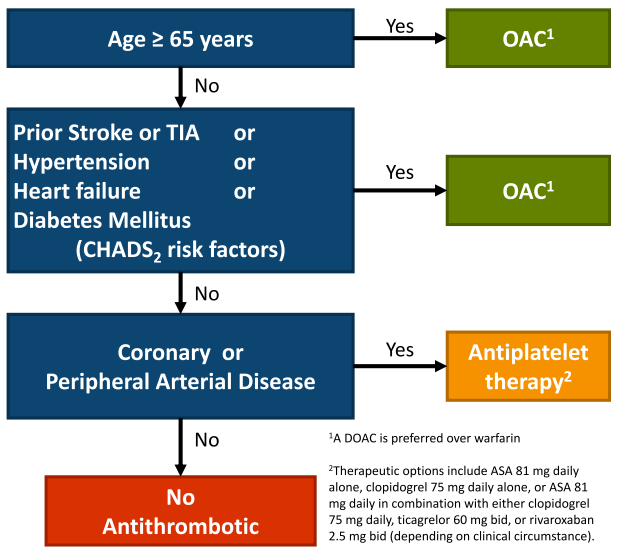
- Note: annual reassessment
- NVAF is defined as AF in the absence of mechanical heart valves or moderate to severe mitral stenosis (rheumatic or non-rheumatic)
Special Circumstances
Renal Failure
- Stage 3 CKD or better (eGFR > 30 mL/min): we recommend that such patients receive antithrombotic therapy as determined by the “CCS algorithm” (YES)
- Stage 4 CKD (eGFR 15-30 mL/min): we suggest that such patients receive antithrombotic therapy as determined by the “CCS algorithm” (YES)
- Stage 5 CKD (eGFR < 15mL/min or dialysis dependent): we suggest that such patients not routinely receive antithrombotic therapy for stroke prevention in AF (NO)
Renal Failure
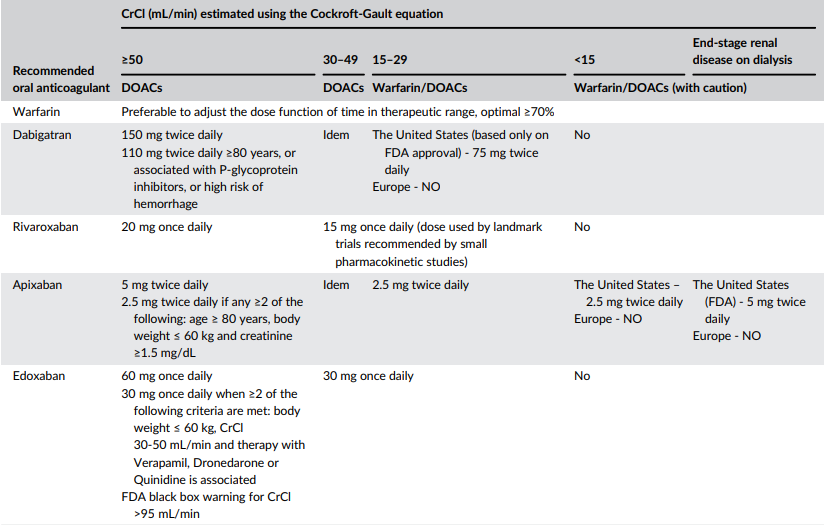
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6671778/
CAD
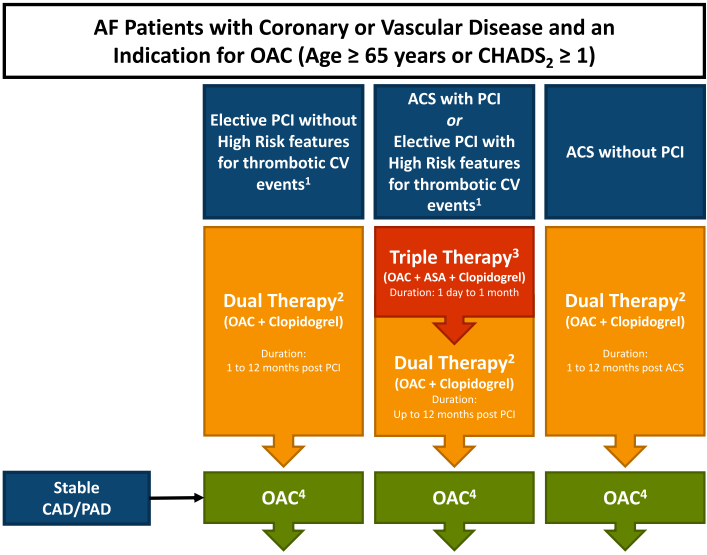
Dual: warfarin, apixaban 5mg, dabigatran 110/150, edoxaban 60, rivaroxaban 15
Triple: warfarin INR 2-2.5, apixaban 5, rivaroxaban 2.5 (DOAC preferred)
Duration of Triple Therapy
- Interventionalist will dictate when
- Balance risk of bleeding to risk of ischemic events
- patients factors, angiographic factors, ACS
- Exam: discuss with Cardiology while weighing risks and benefits
Other Special Populations
- Liver disease: “We recommend that OAC not be routinely prescribed in Child-Pugh class C or liver disease associated with significant coagulopathy.”
- Cancer: Individualize OAC treatment in pts with active cancer. Consider DOAC> VKA.
-
Frail Elderly
- OAC for most frail elderly – individualizing recommendations if high risk bleed
-
Secondary AF (clearly provoked by a transient/reversible risk factor such as severe sepsis, thyrotoxicosis):
- No OAC:
- Exceptions: patient’s underlying ‘abnormal substrate’ and risk for recurrence estimated to be high
• OAC for “most patients during acute thyrotoxicosis until euthyroid state is restored”
- Exceptions: patient’s underlying ‘abnormal substrate’ and risk for recurrence estimated to be high
- No OAC:
Case
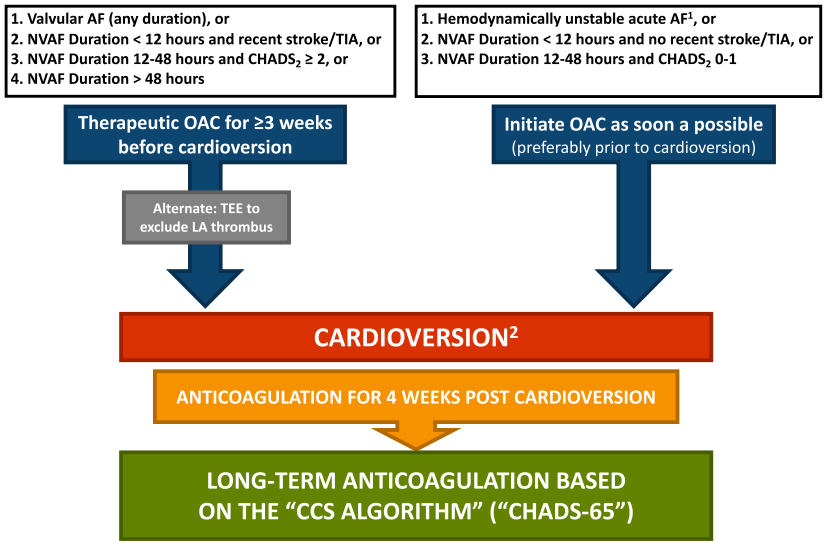
You are called to see a patient in the emergency department with rapid atrial fibrillation. He is hemodynamically stable. Emergency medicine doctors asks if it is safe to cardiovert. His CHADS65 score is 2 and the symptoms clearly started 15 hours ago. How would you proceed?

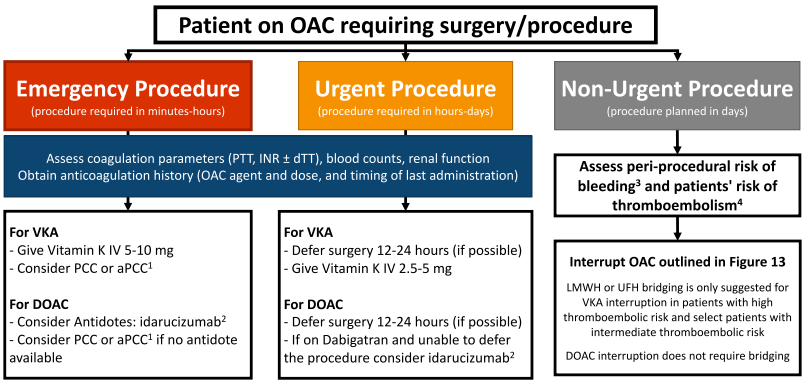
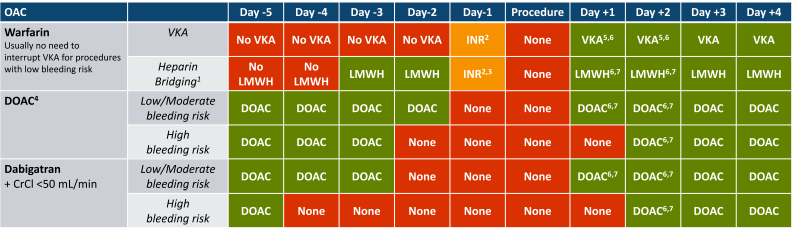
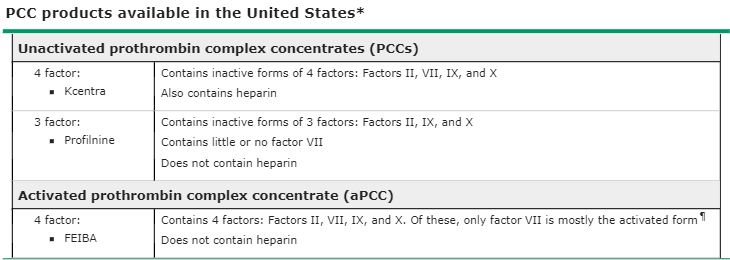
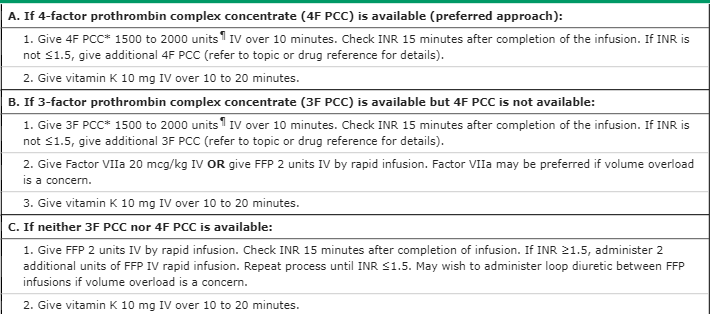
Interrupting Anticoagulation
Evaluation form: Please evaluate me to mark your attendance!
Atrial Fibrillation
By Seana Nelson
Atrial Fibrillation
Afib
- 92



