Syncope
Dr. Seana Nelson PGY 5
Cardiology
Objectives
- Understand etiologies of syncope
- Review syncope work up
- Review management of cardiac syncope
- Review manamgement of other forms of syncope
- Driving and Syncope
Key References
-
Brignole, M., Moya, A., de Lange, F.J., Deharo, J.C., Elliott, P.M., Fanciulli, A., Fedorowski, A., Furlan, R., Kenny, R.A., Martín, A. and Probst, V., 2018. Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope. European heart journal, 39(21), pp.e43-e80.
- Sandhu, R.K., Raj, S.R., Thiruganasambandamoorthy, V., Kaul, P., Morillo, C.A., Krahn, A.D., Guzman, J.C., Sheldon, R.S., Banijamali, H.S., MacIntyre, C. and Manlucu, J., 2020. Canadian Cardiovascular Society clinical practice update on the assessment and management of syncope. Canadian Journal of Cardiology, 36(8), pp.1167-1177.
- Shen, W.K., Sheldon, R.S., Benditt, D.G., Cohen, M.I., Forman, D.E., Goldberger, Z.D., Grubb, B.P., Hamdan, M.H., Krahn, A.D., Link, M.S. and Olshansky, B., 2017. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology, 70(5), pp.e39-e110.
Syncope: Definition
Total loss of consciousness due to cerebral hypoperfusion.
Onset is rapid.
Duration is short.
Recovery is spontaneous and complete.
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope
Total loss of consciousness Definition
Loss of awareness =
amnesia for the period of loss of consciousness
+ unresponsive
Associated with abnormal motor control
Duration is short
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope
Syncope Mechanism
Reduced blood flow for 6-8 seconds.
Reduced SBP 50-60 mmHg at the level of the heart or
SBP 30-45 mmHg at the level of the brain
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope

Total loss of consciousness Differential
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope

Syncope Differential
Reflex Mediated
- Vasovagal
- Situational
- Carotid Sinus
- Non-classical forms
Orthostatic hypotension
- Drug-induced
- Volume depletion
- Primary autonomic (neurogenic)
- Secondary autonomic (neurogenic
Cardiac
- Bradycardia
- Tachycardia
- Structural
- Cardiopulmonary
- Great vessel (e.g. PE, dissection)
Syncope due to a reflex: Differential
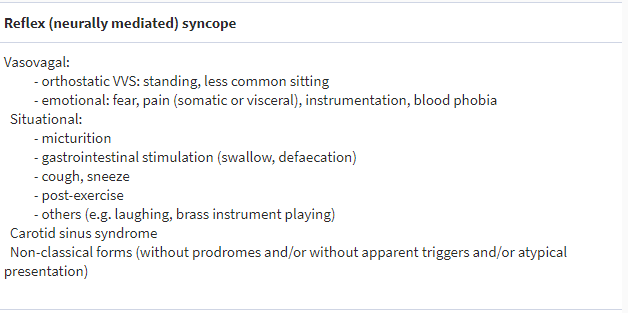
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope
Syncope due to Orthostatic Hypotension: Differential
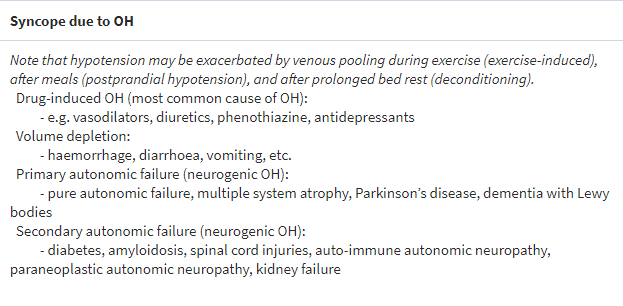
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope
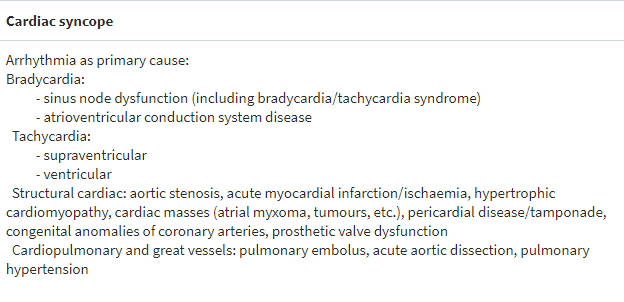
Syncope due to Cardiac causes: Differential
Clinical Syncope Assessment
Key clinical features
- Was there actual loss of consciousness
- If loss of consciousness- was it syncopal or non-syncopal: historical clues
- If syncope- is the cause clear?
- Is the patient high risk for cardiovascular events or death
Key clinical features
-
Was there actual loss of consciousness
- Short duration?
- Loss of awareness and responsiveness?
- If loss of consciousness- was it syncopal or non-syncopal: historical clues
- If syncope- is the cause clear?
- Is the patient high risk for cardiovascular events or death
Key clinical features
- Was there actual loss of consciousness
-
If loss of consciousness- was it syncopal or non-syncopal? Some historical clues-
- Features of the attack
- The onset of the attack
- Occurred during the attack or reported from bystanders
- After the attack
- If syncope- is the cause clear?
- Is the patient high risk for cardiovascular events or death
Key clinical features
- Was there actual loss of consciousness
- If loss of consciousness- was it syncopal or non-syncopal
-
If syncope- is the cause clear?
- History & Physical (*include supine and standing BP)
- ECG
- Additional testing based on findings
- Is the patient high risk for cardiovascular events or death
Syncope: Key historical features
Reflex Syncope
- Long history, starting <40 yo
- After unpleasant sight, sound, smell
- Prolong standing
- During a meal
- In crowded, hot places
- Autonomic activation before: pallor, sweating, N/V
- No HD
Orthostatic hoTN
- While or after standing
- Prolonged standing
- Standing after exertion
- Post-prandial hypotension
- Temporal relationship with start/stop of related medication
- Autonomic neuropathy or PD
Cardiac
- During exercise
- Supine
- Sudden onset palpitations--> syncope
- FHx of sudden death at a young age
- Structural HD
- Coronary HD
- ECG findings
N/V = nausea and or vomiting; HD = heart disease;
PD = Parkinson's disease; FHx = family history
Key clinical features
- Was there actual loss of consciousness
- If loss of consciousness- was it syncopal or non-syncopal
- If syncope- is the cause clear?
- Is the patient high risk for cardiovascular events or death
Diagnostic Criteria
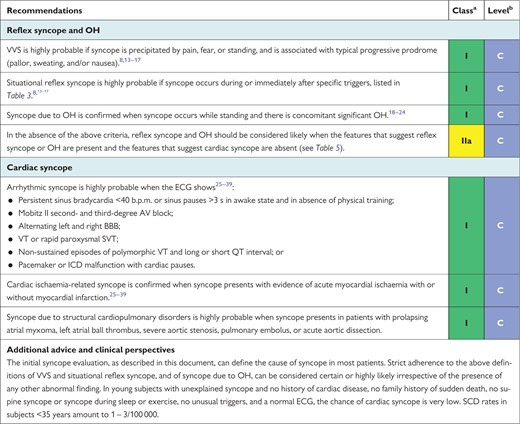
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope
Syncope Risk
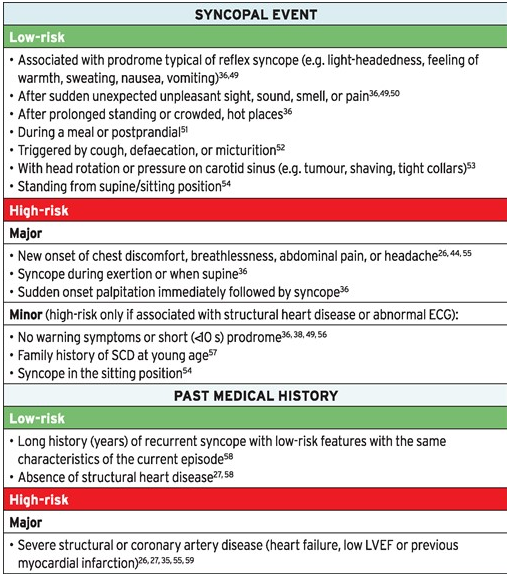
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope
Syncope Risk
| Low Risk | High Risk | |
|---|---|---|
| History | Prodrome typical of reflex Triggers/specific situations Positional syncope Absense of CVD |
Symptoms suggestive of CVD Syncope with exertion or supine without prodrome History of CVD: ischemic, arrhythmic, obstructive, valvular Trauma Family Hx of sudden death (age <50) |
| Physical exam | Normal | Abnormal vitals Abnormal cardiac exam |
| 12- Lead ECG | Normal | Any bradyarrhythmia, tachyarrhythmia or conduction disease |
| Lab values | Normal | Elevated TnT, BNP |
Sandhu et al. 2020 CCS Syncope Guidelines Clinical Practice Update
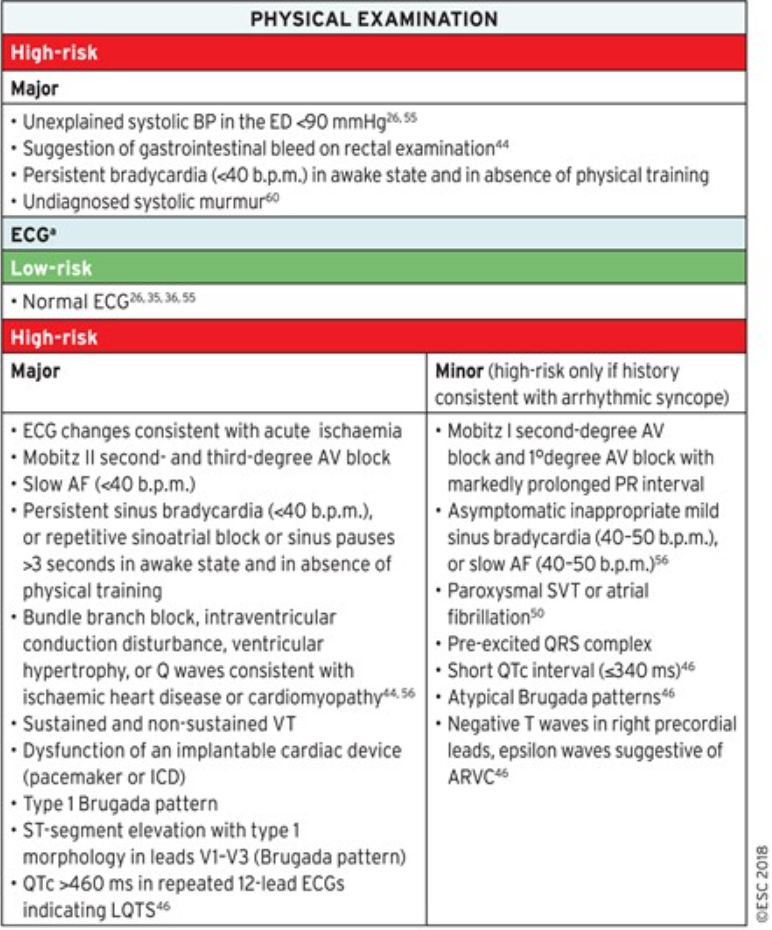
Syncope Risk: ECG
| High Risk | |
|---|---|
| Bradycardia | Asymptomatic inappropriate sinus rate < 50 bpm or slow AF (40-50 bpm), Sinus block Sinus pause > 3 seconds without negatively chronotropic medications |
| Conduction disease | Bifascicular block Intraventricular conduction delay (QRS 120 ms) Second-degree AV block type 1 with prolonged PR interval Second-degree AV block type 2 Third-degree AV block |
| Tachyarrhythmia | |
| Supraventricular tachycardia | Ventricular pre-excitation Supraventricular tachycardia or AF |
| Ventricular tachycardia | Nonsustained ventricular tachycardia Evidence of acute ischemia or previous myocardial infarction Long (> 460 ms) QT on repetitive ECGs or short (< 340 ms) QT interval Type 1 Brugada Brugada pattern (RBBB with ST elevation V1-V3) Arrhythmogenic right ventricular cardiomyopathy features (negative T waves in right precordial leads, epsilon wave, ventricular late potentials) Ventricular hypertrophy |
Sandhu et al. 2020 CCS Syncope Guidelines Clinical Practice Update
Syncope: Arrhythmic ECG features
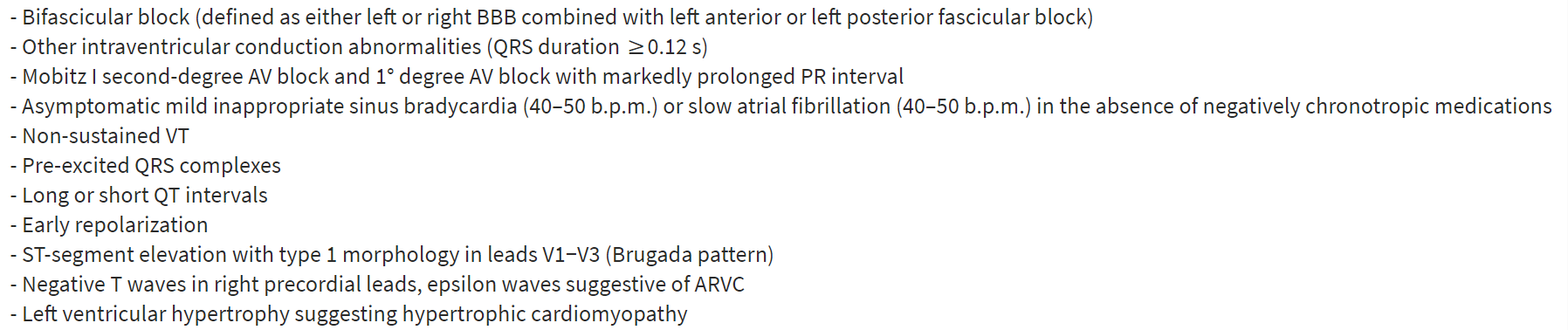
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope
Syncope Decision Tool?
- There are numerous tools, e.g. Canada Syncope Tool
- Outside of Canada perform no better than clinical judgement
- Features consistently associated with poor outcomes:
- older age
- heart disease
- abnormal vital signs
- abnormal ECG
-
abnormal lab values—
- hemoglobin/hematocrit, troponin, or natriuretic peptides;
- presumed etiology
To admit or not to admit?

Sandhu et al. 2020 CCS Syncope Guidelines Clinical Practice Update
Possible specific testing
- Carotid hypersensitivity
- Orthostatic Challenges:
-
Autonomic function testing
- Valsalva manoeuvre
- Deep breathing
- 24-hour ambulatory blood pressure monitoring
- Arrhythmia monitoring
- Structural disease
- Echocardiography
- Stress echocardiography
**Persued based on clinical suspicion**
Tilt Table Testing
- Syncope triggered by prolonged standing.
- Confirm reflex syncope diagnosis
- Assessment of autonomic failure by initial evaluation
- Postural orthostatic tachycardia syndrome
- Delayed orthostatic hypotension
Specific testing: Arrhythmia monitoring
Specific testing:
Arrhythmia monitoring

Sandhu et al. 2020 CCS Syncope Guidelines Clinical Practice Update
Specific testing:
Arrhythmia monitoring
- Symptom rhythm correlation
- Finding of a significant rhythm:
- Pause > 3 seconds
- Rapid SVT (>160 bpm for >32 beats)
- Ventricular tachycardia
Specific testing: EP Study
-
In the broad population, there is limited use of EPS
- Often etiology can be identified by rhythm monitoring
- Indications per ESC:
- Asymptomatic sinus bradycardia (suspected sinus arrest)
- Bifascicular bundle branch block- concern for impending high-degree AV block
- Suspected tachycardia
Specific testing: EP Study Indications for PM
- Asymptomatic sinus bradycardia (suspected sinus arrest)
- High pre-test probability
- if sinus bradycardia HR < 50
- Sinoatrial block
- Prolong sinus node recovery time on EPS >1.6 or 2 seconds or >525 ms corrected
- High pre-test probability
- Bifascicular bundle branch block- concern for impending high-degree AV block
- Suspected tachycardia
Specific testing: EP Study Indications for PM
- Asymptomatic sinus bradycardia (suspected sinus arrest)
-
Bifascicular bundle branch block- concern for impending high-degree AV block
- Prolonged His-Purkinje conduction time (HV interval) >70 ms
- Induction of 2' or 3' AV block with procainamide or disopyramide
- Suspected tachycardia
Specific testing: EP Study Indications for PM/ICD
- Asymptomatic sinus bradycardia (suspected sinus arrest)
- Bifascicular bundle branch block- concern for impending high-degree AV block
-
Suspected tachycardia
- Induction of VT in patients with previous MI and Normal LVEF
Managemenent of Cardiac syncope
Cardiac pacing
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope

Cardiac pacing in SND
2018 ACC/AHA/HRS bradycardia and conduction guidelines


Cardiac pacing
2018 ACC/AHA/HRS Bradycardia and conduction delay guidelines

Cardiac syncope due to tachyarrhythmias
Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope


Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope
Management of Syncope in structural heart disease
- ICD for low EF following OMT >3 months, if syncope occurs ICD can be considered or monitoring (ILR ) (ESC IIa)
- HCM patients should have ICD following syncope if HCM (2a AHA/ACC)
- ICD for ARVC with syncope, or ILR if low risk based on multiparametric analysis
-
Long QT Syndrome with syncope: ICD + Beta-blockers
- Left cardiac sympathetic denervation in symptomatic LQTS: beta-blockers not tolerated, ICD contraindicated, on beta-blockers and multiple ICD shocks
- Brugada Syndrome: ICD for type 1 ECG pattern and syncope
LQTS: Long QT Syndrome
Management of Non-Cardiac Syncope
Vasovagal syncope management
- Reassurance of benign nature
- Avoidance of triggers
- Lying down at the onset of pre-syncope symptoms
- Failure of non-pharmacologic treatment occurs in 15-20%
- Combination therapy is occasionally needed for patients with refractory VVS.
- β-Blockers may be used in patients older than 42 years
- Fludrocortisone (0.2 mg/d once a day) or midodrine (5-15 mg every 4 hours, 3 times a day)
-
Pacemaker indications for vagal syncope: only if very symptomatic and other options have been exhausted.
- Documented symptomatic asystole > 3 seconds or asymptomatic asystole > 6 seconds
- Tilt-induced: asystole > 3 seconds or heart rate < 40 beats per minute for > 10 seconds.
Management of syncope from orthostatic hypotension
- Reassurance
- Salt + Water intake (if no contraindications)
- Discontinue offending medications
- Counter pressure manoeuvres, compression stockings
- Failure of non-pharmacologic interventions:
- Fludrocortisone
- Midrodine
Syncope and Driving
Syncope and Driving
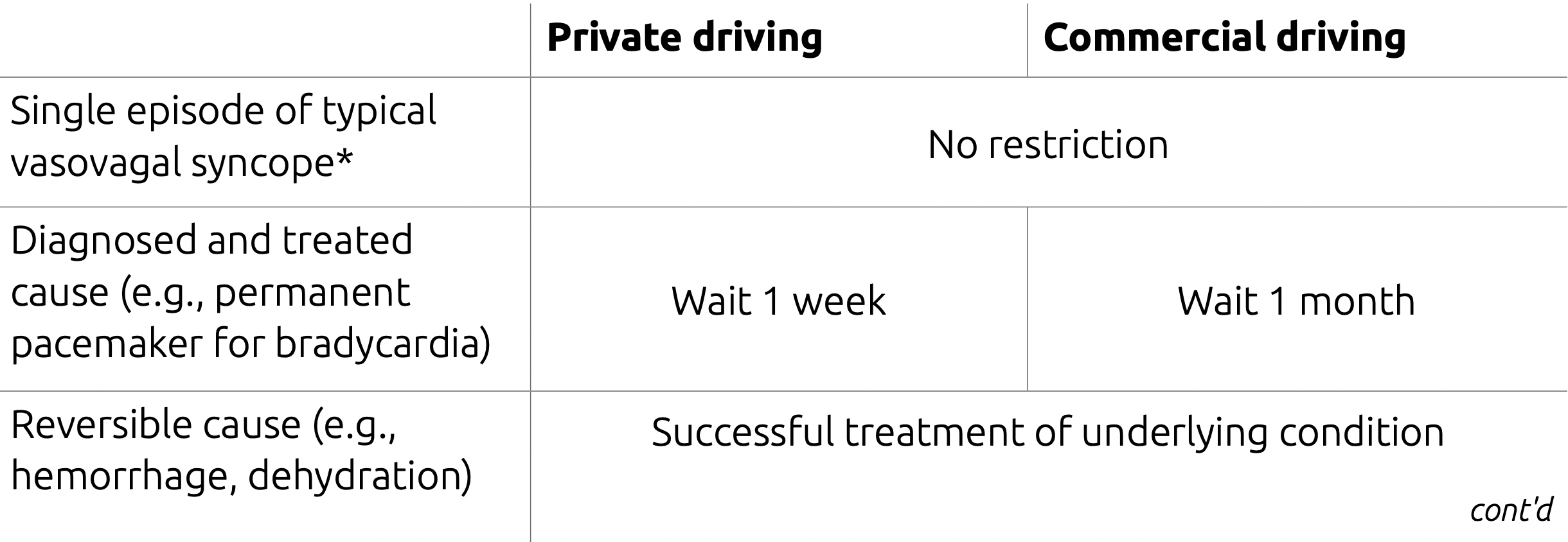
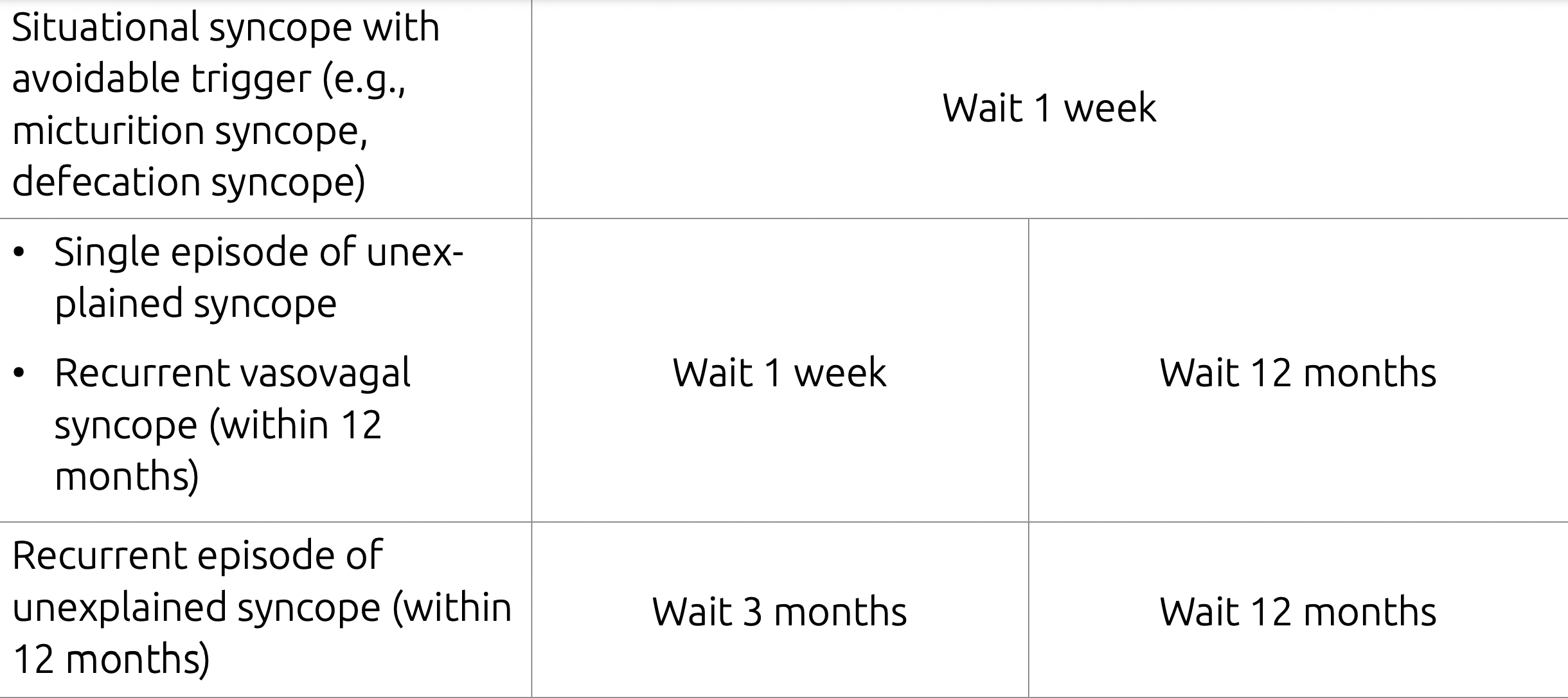
CMAJ 2017 Driver's guide 9th Ed.
deck
By Seana Nelson
deck
- 98



